Browse our range of reports and publications including performance and financial statement audit reports, assurance review reports, information reports and annual reports.
The Management, Administration and Monitoring of the Indemnity Insurance Fund

Please direct enquiries relating to reports through our contact page.
The audit objective was to assess the departments of Health and Human Services’ administration, including oversight and monitoring arrangements, for the Indemnity Insurance Fund.
Summary and recommendations
Background
1. The Indemnity Insurance Fund was established in 2011 to consolidate seven existing government assistance schemes providing medical and professional indemnity support for medical practitioners and midwives. The relevant schemes, established between 2003 and 2010, aimed to address market failure and stabilise the medical indemnity industry after Australia’s largest provider of medical indemnity cover, United Medical Protection, was placed in provisional liquidation in May 2002. From 1 July 2003, all providers of medical indemnity insurance were required to be licensed under the Insurance Act 1973, supervised by the Australian Prudential Regulatory Authority.
2. Priorities for the Indemnity Insurance Fund are: promoting stability in the medical indemnity insurance industry; keeping premiums affordable for doctors; and ensuring availability of professional indemnity insurance for eligible midwives.
3. Funding for the Indemnity Insurance Fund is provided from special appropriations and departmental appropriations to the departments of Health and Human Services. Total expenditure under the schemes since the commencement is estimated to be under $0.45 billion.
4. In February 2014, the National Commission of Audit recommended that the Commonwealth scale back its subsidies for medical indemnity insurance and reported that there is evidence that the market is normalising—average premiums had declined since 2003–04 to become more affordable and net assets and reported profits in the industry had increased. The Government’s response to the National Commission of Audit report was that ‘Reforms to Medical Indemnity will be considered following the 2014–15 Budget’.1
Audit objective and criteria
5. The audit objective was to assess the departments of Health and Human Services’ administration, including oversight and monitoring arrangements, for the Indemnity Insurance Fund.
6. To form a conclusion against the objective, the ANAO adopted the following high level criteria:
- the Department of Health has in place and ensures adequate oversight and probity for the Indemnity Insurance Fund.
- the Department of Health has implemented a proper system for monitoring, review and reporting to the Minister including assessing priorities for the Indemnity Insurance Fund, consistent with the aims and objectives of the Indemnity Insurance Fund; and
- the Indemnity Insurance Fund and associated schemes are supported by sound administrative arrangements.
Conclusion
7. The government’s package of regulatory and financial measures, established to address market failure in the early 2000s, was informed by a range of expert advice and subject to monitoring and a number of independent reviews during the first five years of its implementation. Overall, the design and implementation of these measures significantly improved the financial viability of insurers and ensured the availability and general affordability of indemnity insurance. The measures implemented however, resulted in a significant financial risk transfer to the Commonwealth.
8. The Department of Health does not have fit-for-purpose monitoring and reporting arrangements in place to assess the impact of the measures—including regulatory and other legal reforms on the stability of the indemnity insurance market, the affordability of premiums or importantly, the government’s exposure to risk. The departments of Health and Human Services developed and documented bilateral management and administrative arrangements to support the delivery of the Indemnity Insurance Fund’s support measures. While these arrangements set out each entity’s roles and responsibilities, documented mechanisms for cross-entity risk management were not in place. Both entities’ internal and external guidance materials need to be reviewed and updated.
9. There is scope for the entities to review and put measures in place to ensure that the information and data collected from insurers against the schemes is accurate and relevant to better inform actuarial assessments, risk analysis and the measurement and reporting of the performance of the schemes against the Indemnity Insurance Fund’s objectives. There is also a need for the entities to improve the relevancy and completeness of public and internal performance indicators, including implementing measures to monitor and report the actual cost to the government to administer the Indemnity Insurance Fund.
Supporting findings
10. A range of expert analysis, advice and stakeholder consultations informed the government’s response to the financial crisis in the medical indemnity insurance market. Following the early phases of this response, monitoring and a number of reviews by experts were conducted examining the financial and other measures adopted. However, there was limited consideration of the risk exposure to the Commonwealth and a longer-term exit strategy for a point in time when the market was determined to have stabilised and insurance premiums were considered affordable.
11. Overall, the financial strength of the medical indemnity insurance market has improved significantly since the Indemnity Insurance Fund schemes and Australian Prudential Regulation Authority’s regulatory oversight were introduced in 2002. In the years following the government’s response, net assets and capital holdings of insurance providers has improved markedly, with providers’ market share also largely stabilised.
12. Since 2003–04, there have also been improvements in the affordability of average insurance premiums paid by most medical specialities. Professional indemnity insurance for midwives continues to be available.
13. The Department of Health however, does not have an effective monitoring arrangement in place or a strategy for consulting stakeholders to support its policy and administrative responsibilities for assessing the stability of the indemnity insurance market. Information received by the Department of Health on professional indemnity insurance for midwives is also limited.
14. To date, the Department of Health has not reviewed or evaluated the Indemnity Insurance Fund legislation, supporting regulatory and other legal reforms, or the schemes’ financial assistance packages for their impact on the availability and affordability of indemnity insurance. The Department of Health’s reporting to its Minister on the Indemnity Insurance Fund’s performance and risks is largely ad hoc and driven by external processes, for example the annual Budget process. Overall, the Department of Health’s arrangements for review, analysis and advice to its Minister on the Indemnity Insurance Fund schemes, including risks and performance against the Indemnity Insurance Fund’s objectives and priorities, are limited.
15. Although, the roles of the Australian Government entities, including contracted insurers, for delivery of Indemnity Insurance Fund-related regulation and administrative responsibilities are generally clear, the Department of Health has not established any regular intragovernmental or stakeholder engagement arrangements to coordinate or communicate Indemnity Insurance Fund-related policy and regulatory developments.
16. There is no coordinated cross-entity risk management arrangement in place for medical indemnity matters, including the Indemnity Insurance Fund and related schemes. Bilateral management arrangements for the medical indemnity programs between the departments of Health and Human Services are governed by joint agreements. However, no overarching bilateral risk management plans or formal arrangements have been established for the Indemnity Insurance Fund schemes.
17. The Department of Health does not have any risk management plans, including regular assessment, monitoring and mitigation arrangements in place to support its Indemnity Insurance Fund-related policy responsibilities. The Department of Human Services has established suitable risk management plans and review arrangements to support its Indemnity Insurance Fund-related administrative responsibilities.
18. The bilateral agreements between the departments of Health and Human Services set out key administrative arrangements intended to support the operation and delivery of the Indemnity Insurance Fund schemes.
19. There is scope to improve the relevancy and completeness of the departments of Health and Human Services’ public and internal performance indicators.
20. The Department of Health published the Indemnity Insurance Fund guidelines which outline key aspects of the Indemnity Insurance Fund’s administrative arrangements. The Department of Human Services established a range of internal guidance materials to assist its administration of the Indemnity Insurance Fund’s schemes. However, some of the guidance materials contain inaccuracies and need to be reviewed and updated.
21. The Department of Human Services’ claims assessment process, a series of manual and paper-based processes, was supported by a reasonable quality assurance process. Human Services delayed the development of a medical indemnity online claiming system, which is intended to realise efficiencies for both insurers and the department; the department’s new electronic claiming system was expected to be delivered by October 2016. However, the department advised the ANAO that the project has been further delayed and a new implementation date has not yet been identified.
22. During 2014–15, due to problems with the functionality of its Health Professional Online System, the Department of Human Services implemented data transfer arrangements, albeit temporarily, and did not document its consideration of the risk of any compromise of the confidentiality of midwives’ personal information.
23. There is scope to improve the Department of Human Services’ Indemnity Insurance Fund data integrity controls. In particular, the relevance, accuracy, and consistency of data provided by insurers, including to the Australian Government Actuary.
24. The departments of Health and Human Services do not report on the costs of administering the Indemnity Insurance Fund and related schemes in a consistent and transparent manner.
25. While the department of Health publicly reports its Indemnity Insurance Fund departmental costs, Human Services does not report on its own Indemnity Insurance Fund-related costs.
26. The Department of Health has not recently reviewed the basis on which the administration fees paid to insurers are calculated to ensure ongoing value for money to the government. To improve transparency, there would be particular benefit in the departments of Health and Human Services’ analysing and reporting on the costs of Indemnity Insurance Fund administration over time.
27. Further, the reasonableness of the current administration costs needs to be considered by the Department of Health in undertaking a ‘first principles review’ of the Indemnity Insurance Fund and related schemes.
Recommendations
|
Recommendation No. 1 Paragraph 2.93 |
The Department of Health should conduct a ‘first principles review’ of the Indemnity Insurance Fund and related schemes prior to the 2017–18 Budget. Health’s response: Agreed with qualification. |
|
Recommendation No. 2 Paragraph 2.95 |
Subject to the outcome of this ‘first principles review’, the Department of Health should develop and implement a fit-for-purpose monitoring and reporting arrangement for the Indemnity Insurance Fund, legislation, and related schemes that provides its Minister with timely, robust analysis of the Indemnity Insurance Fund’s performance and risks to government. Health’s response: Agreed. |
|
Recommendation No. 3 Paragraph 3.17 |
That the Department of Health establish suitable governance and stakeholder engagement arrangements, including risk management plans, to support its and other shared responsibilities for the administration of the Indemnity Insurance Fund and related schemes. Health’s response: Agreed. |
|
Recommendation No. 4 Paragraph 3.44 |
That the departments of Health and Human Services review their Indemnity Insurance Fund administrative arrangements to:
Health’s response: Agreed. Human Services’ response: Agreed. |
Summary of entity responses
The Department of Health
I am pleased that the ANAO found that the medical indemnity and midwife professional indemnity schemes continue to improve the affordability of medical indemnity insurance premiums. The Government’s contribution strengthens the medical indemnity industry, and ensures professional indemnity for private midwives remains available, which are key objectives of the Indemnity Insurance Fund schemes. The report has highlighted important areas for improvement, particularly with regard to re-establishing appropriate frameworks to ensure good governance, stakeholder engagement and risk management.
The Department of Health’s implementation of the ANAO ‘s recommendations, including those in partnership with the Department of Human Services, will provide sound and timely advice to the Australian Government on the operation of and risks associated with, the Medical Indemnity and Midwife Professional Indemnity schemes.
The Department of Human Services
The Department of Human Services (the department) welcomes this report and notes that the ANAO found that the department has established suitable risk management plans and review arrangements to support the administration of payments under the Indemnity Insurance Fund (IIF). The report also concluded that the department’s claims assessment process is supported by reasonable quality assurance processes.
The department considers that implementation of the audit recommendations will further enhance the department’s administration of the IIF, and will work with the Department of Health to improve its shared administrative responsibilities.
1. Background
What is medical indemnity insurance?
1.1 Medical indemnity insurance provides financial protection (to the extent set out in the insurance contract) to both medical practitioners and patients in circumstances where a patient sustains an injury (or ‘adverse outcome’) caused by negligence or an otherwise unlawful act.
1.2 All medical practitioners are required to hold medical indemnity insurance in order to practice privately, as a condition of their professional registration. In this regard, the availability of affordable medical indemnity insurance contributes to the stability in supply of Australia’s health services. Further, it supports patients’ access to relevant medical services, including mitigating the potential for additional fees stemming from high insurance costs.2
The medical indemnity ‘crisis’
1.3 Until 2001, most medical indemnity insurance cover was provided by medical defence organisations—which differed from general insurance providers as cover was provided on a discretionary basis.3 The 2001 financial collapse of HIH Insurance Limited—a major reinsurer of United Medical Protection Limited/Australasian Medical Insurance Limited (UMP/AMIL), Australia’s largest medical defence organisation—was a critical event for the medical indemnity insurance industry. It was also a catalyst for increased government intervention in the medical indemnity insurance industry, including substantial legal, regulatory and funding reform.
1.4 UMP/AMIL was placed into provisional liquidation in May 2002 ‘…which resulted in a potential lack of indemnity cover for many doctors’ in Australia’.4 At the same time, medical practitioners experienced significant increases in the insurance premiums being levied by all medical indemnity providers. In extreme cases, some medical practitioners were paying indemnity insurance premiums representing over a third of their incomes while others left the profession or ceased certain high-risk procedures like obstetrics.5
1.5 For the Australian Government, these events created two broad, inter-related and complex policy issues that needed immediate attention while recognising that any longer-term solution would require a whole-of-government approach.
The development of appropriate policy responses to these issues presents serious challenges, because of the complexity of contributing factors and the range of interested stakeholders, including not only Commonwealth and state and territory governments but also patients, doctors, insurers and other groups.6
1.6 Between 2002 and 2010, the Australian Government implemented a range of financial and regulatory measures to prevent an immediate collapse of the insurance industry and to support the availability and affordability of medical indemnity insurance. These measures were underpinned by tort law reform7 at the state and territory level.
The Indemnity Insurance Fund
1.7 The Indemnity Insurance Fund (IIF) was an Australian Government initiative administered by the Department of Health (Health) designed to consolidate funds that provide Commonwealth support for medical and professional indemnity insurance for medical practitioners.8 Funding was previously separately administered through five general medical indemnity schemes and two professional indemnity for midwives schemes.9 In this context, the IIF’s primary objective was to streamline the administration of the existing schemes with the following priorities:
- promote stability of the medical indemnity insurance industry—to ensure the ongoing stability of the medical indemnity insurance industry, the department will continue to monitor the operations and activities of medical indemnity insurers;
- keep premiums affordable for doctors—a stable and competitive medical indemnity industry assists in keeping medical indemnity premiums affordable for doctors; and
- ensure availability of professional indemnity insurance for eligible midwives—the government contracted an insurer, Medical Insurance Group Australia, to provide professional indemnity insurance to eligible midwives.10
1.8 As of July 2016, the financial support measures in place, consolidated under the IIF, include the: Premium Support Scheme; High Cost Claims Scheme; the Exceptional Claim Scheme; Run-off Cover Scheme; Incurred-But-Not-Reported Scheme; Midwife Professional Indemnity Commonwealth Contribution Scheme; and the Midwife Professional Indemnity Run-off Cover Scheme. A summary of each of the schemes under the IIF and their purpose is set out in Table 1.1.
Table 1.1: Schemes within the Indemnity Insurance Fund
|
Scheme |
Purpose and key features |
|
Incurred-But-Not-Reported (IBNR) Scheme |
To cover unfunded medical indemnity insurers’ liabilities that were incurred but not reported as at 30 June 2002. The government covers the costs of claims from unfunded liabilities. Members contributed to these costs through support payments. UMP/AMIL has been the only provider to participate in the scheme. UMP support payments ceased in 2007–08. |
|
Premium Support Scheme (PSS) |
To assist eligible practitioners with the cost of medical indemnity insurance through payment of subsidies (through insurers applying a reduction in premiums), where medical indemnity costs exceed 7.5 per cent of their gross private medical income. The relevant premium periods and applicable subsides were:
|
|
High Cost Claim Scheme (HCCS)(a) |
To place downward pressure on premiums, particularly for doctors in high-risk areas by lowering the amount insurers pay out and reducing the amount of reinsurance insurers need to buy to fund large claims. For each claim over $300 000, the government reimburses medical indemnity insurers 50 per cent of the insurance pay out over $300 000 up to the limit of the practitioner’s cover. Claims that exceed the insurance contract limit (generally $20 million) can trigger an ECS. |
|
Exceptional Claim Scheme (ECS) |
To remove risk from practitioners for very high claims so that practitioners are not personally liable. The government pays 100 per cent of the cost of private practice claims that are above the limit of a practitioner’s medical indemnity insurance (generally $20 million). |
|
Run-off Cover Scheme (ROCS) |
To provide secure insurance for doctors who have left private practice. The government pays the costs of valid medical indemnity insurance claims (including the costs related to managing claims) made against doctors eligible for ROCS including those that have retired, deceased or are on maternity leave. The ongoing cost of ROCS is met over time by a ROCS support payment paid by insurers to the Government. The Australian Government Actuary notes that ‘In practice, the cost is met by a loading on practitioners’ medical indemnity insurance premiums’. |
|
Midwife Professional Indemnity (Commonwealth Contribution) Scheme (MPIS) |
To ensure availability of professional indemnity insurance for privately practicing eligible midwives. The insurer pays the first $100 000 for each claim. The government will pay 80 per cent of the insurance pay out exceeding $100 000 up to $2 million, and 100 per cent of the amount exceeding $2 million. |
|
Midwife Professional Indemnity Run-off Cover Scheme (MPIROC) |
To provide secure indemnity insurance for midwives who have left private practice. The government will pay, via the insurer, 100 per cent of each eligible ROC claim that is notified after a midwife leaves the workforce or retires. |
Note a: This scheme has three threshold levels, which are dependent on the date the claim was first notified to the insurer: 1 January 2003 to 21 October 2003, $2 000 000; 22 October 2003 to 31 December 2003, $500 000 and on or after 1 January 2004, $300 000.
Source: Department of Health, Medical Indemnity website. Available from: <http://www.health.gov.au/internet/main/publishing.nsf/Content/budget2011-flexfund-indemnity19.htm>.
Administrative arrangements
1.9 Health has policy responsibility for the IIF, including its seven schemes, as well as defined responsibilities under relevant legislation.
1.10 The Department of Human Services (Human Services), under its Medicare program, is responsible for administering payments to relevant insurers for all of the medical indemnity package measures.
1.11 Under tripartite contracts with Health and Human Services, the premium support and professional indemnity for midwives schemes are jointly administered by Human Services and medical indemnity insurance providers, with Health retaining overall policy and financial responsibility.11
1.12 Within the Treasury portfolio, the Australian Prudential Regulation Authority (APRA) and the Australian Securities and Investment Commission (ASIC) provide regulatory supervision (see Appendix 3).12
1.13 Funding for the IIF is made through special appropriations for medical indemnity and midwives professional indemnity with separate appropriations for Health’s departmental expenses. Reported actual expenditure under the IIF schemes including special appropriations for the period 2004–05 to 2014–15 was under $0.45 billion13 with departmental expenses of $7.1 million over the same period.14 A summary of financial arrangements for the IIF schemes is set out in Appendix 2.
1.14 Human Services receives funding for administering its responsibilities under the IIF schemes through broader departmental appropriation.15
Audit approach
1.15 The audit objective was to assess the departments of Health and Human Services’ administration, including oversight and monitoring arrangements, for the Indemnity Insurance Fund.
1.16 To form a conclusion against the audit objective, the ANAO adopted the following high-level criteria including the:
- Department of Health has implemented a proper system for monitoring, review and reporting to the Minister including assessing priorities for the IIF, consistent with the aims and objectives of the IIF;
- Department of Health has in place and ensures adequate oversight and probity for the IIF; and
- the IIF and associated schemes are supported by sound administrative arrangements.
Audit methodology
1.17 The audit methodology included:
- interviewing key officials in the departments of Health and Human Services, the Treasury, as well as the Australian Government Actuary;
- interviewing and/or surveying key external stakeholders including: ASIC; APRA; relevant medical and professional midwife indemnity insurers; and peak medical and midwife organisations16;
- reviewing relevant documentation from the departments of Health and Human Services;
- analysis of data collected in relation to claims, payments and other reporting in relation to the IIF schemes; and
- reviewing available information technology design documentation for the proposed Department of Human Services electronic payment system for analysis of suitability of key quality and integrity controls.
1.18 The audit was conducted in accordance with ANAO auditing standards at a cost to the ANAO of approximately $563 750.
2. Design, monitoring and review of the Indemnity Insurance Fund and the Commonwealth’s exposure to risk
Areas examined
This chapter considers the government’s intervention in the medical indemnity insurance sector and the design of the various schemes; and whether the Department of Health is actively monitoring, reviewing and advising government on the Indemnity Insurance Fund schemes’ achievements, including the ongoing need for government assistance and the Commonwealth’s exposure to risk.
Conclusion
The government’s package of regulatory and financial measures, established to address market failure in the early 2000s, was informed by a range of expert advice and subject to monitoring and a number of independent reviews during the first five years of its implementation. Overall, the design and implementation of these measures significantly improved the financial viability of insurers and ensured the availability and general affordability of indemnity insurance. The measures implemented however, resulted in a significant financial risk transfer to the Commonwealth.
The Department of Health does not have fit-for-purpose monitoring and reporting arrangements in place to assess the impact of the measures—including regulatory and other legal reforms on the stability of the indemnity insurance market, the affordability of premiums or importantly, the government’s exposure to risk.
Areas for improvement
The ANAO has made two recommendations aimed at undertaking a ‘first principles review’ of the Indemnity Insurance Fund and schemes prior to the 2017–18 Budget, and consistent with undertaking the review, establishing fit-for-purpose monitoring and reporting arrangements.
Did sound analysis and advice support the government’s decision to establish the medical indemnity schemes?
A range of expert analysis, advice and stakeholder consultations informed the government’s response to the financial crisis in the medical indemnity insurance market. Following the early phases of this response, monitoring and a number of reviews by experts were conducted examining the financial and other measures adopted. However, there was limited consideration of the risk exposure to the Commonwealth and a longer term exit strategy for a point in time when the market was determined to have stabilised and insurance premiums were considered affordable.
2.1 In December 2001, the Prime Minister announced that ‘the government would convene, in early 2002, a high-level forum on medical indemnity insurance [the Medical Indemnity Review Panel] with the aim of developing a coordinated approach to issues including re-insurance, prudential arrangements, litigation and settlement levels’.17
2.2 In light of the cross jurisdictional nature of the issues, the government engaged with Commonwealth, state and territory forums18, and stakeholders including: legal associations, the Australian Medical Association and other peak medical bodies, along with medical indemnity insurers and lobby groups.
2.3 External advice was sought from various experts on options for, and the design of, the proposed financial schemes.
2.4 The initial government measures included: underwriting by government of all Incurred-But-Not-Reported (IBNR) liabilities not adequately provisioned for (IBNR Scheme);19 subsidies for medical practitioners in high risk specialties (Medical Indemnity Subsidy Scheme); assistance to medical indemnity providers to help reduce the impact of high cost claims (High Cost Claims and Exceptional Claims Schemes); and the introduction of a new regulatory framework for insurers, placing providers of medical indemnity insurance under the regulatory supervision of the Australian Prudential Regulatory Authority (APRA)20 underpinned by tort law reforms.
2.5 The introduction of these measures (in particular the High Cost Claims and Exceptional Claims Schemes) was, in effect, a financial risk transfer to the Commonwealth. While consideration of insurers’ medical indemnity outlays—including the level of risk that they carried, the integration of risk management into the insurance process, and risks associated with a doctor’s personal liability—were well documented, there was limited evidence of consideration of the risk exposure to the Commonwealth.
2.6 The government’s response to market failure in the medical indemnity insurance industry was phased over time, driven by events within the medical indemnity and broader insurance industries as illustrated in Figure 2.1.
Figure 2.1: Timeline of key indemnity insurance events from 2002 to 2016

Source: ANAO analysis.
Third party arrangements to monitor the indemnity insurers and the market
2.7 In 2002, the Australian Institute of Health and Welfare (AIHW) was commissioned to develop a national database of medical indemnity claims and their outcomes—referred to as the Medical Indemnity National Collection (MINC) and report on the data annually.21 The reports from 2008–09 to 2012–13 included both public and private sector claims data as available.22 The final report was published on 11 July 2014.
2.8 In 2002, APRA was also commissioned to establish the National Claims and Policies Database which provides aggregated, public data on public liability and professional indemnity insurance.23 The database was established to increase transparency and provide data for analysis by insurers and government for monitoring, review and policy development.
2.9 From 2003 to 2008, the Australian Competition and Consumer Commission (ACCC) monitored the schemes, and reported on the Australian Government’s medical indemnity reforms24 (including the High Cost Claims Scheme (HCCS) and the Run-off Cover Scheme (ROCS)) as well as Commonwealth, state and territory tort law reforms.25
2.10 The Australian Government Actuary (AGA) is also required to annually report to the Minister on the Run-off Cover Schemes26, as discussed at paragraph 2.61.
Reviews of the government’s support measures
2003 Medical Indemnity Policy Review
2.11 During 2002–03, the Medical Indemnity Review Panel (the Review Panel) held an inquiry into Australia’s medical indemnity insurance system, reporting in December 2003 with 15 recommendations—12 of which directly related to the schemes now consolidated under the IIF. The government accepted all recommendations, including that by mid-2005, an evaluation be conducted of the effectiveness of the new measures, including current market arrangements.27
2004 Review of Competitive Neutrality in the Medical Indemnity Insurance Market
2.12 In December 2004, the Minister for Health and Ageing, the Minister for Revenue and Assistant Treasurer commissioned the Review of Competitive Neutrality in the Medical Indemnity Insurance Market. The review concluded, among other things, that the specific assistance provided to United Medical Protection Limited/Australasian Medical Insurance Limited (UMP/AMIL) through the IBNR Indemnity Scheme (and not granted to any other medical indemnity provider) had resulted in a competitive advantage.28
2.13 The Australian Government accepted the review’s findings and legislated to remove the competitive advantage by requiring that UMP/AMIL, who had benefited from the IBNR Indemnity Scheme, make a series of repayments to the government. In 2005–06, UMP repaid to the government a sum of $56 million to settle its competitive advantage payment liability.29
2007 Medical Indemnity Policy Review
2.14 Consistent with its 2003 report, in December 2005, the Review Panel reconvened and conducted a post implementation review of the government’s medical indemnity measures. Key recommendations from the review were that the existing package of medical indemnity measures should continue and a stakeholder forum be established to monitor indemnity matters in a ‘…timely, proactive and consultative manner by the industry, medical profession and government.’30 The stakeholder forum is further discussed in paragraphs 2.20 and 2.31–2.32.
National Maternity Services Review and Plan
2.15 In 2008, Health undertook a national review of maternity services.31 These findings and recommendations informed the development of the National Maternity Services Plan. A key commitment under this plan was that the ‘Australian Government would oversee reforms to the maternity workforce, including support for professional indemnity insurance for eligible midwives’.32
2.16 In 2010 regulatory changes for midwives combined with the reported limited commercial availability of insurance for privately practicing midwives33, led to the government establishing two related indemnity insurance schemes—largely modelled on the existing High Cost Claims and Run-off Cover Schemes:
- The Midwife Professional Indemnity (Commonwealth Contribution) Scheme; and
- The Midwife Professional Indemnity Run-off Cover Scheme.
Legal arrangements
2.17 The gradual rollout of the government’s medical indemnity support measures resulted in amendments to or the passage of 12 pieces of primary legislation affecting medical indemnity insurance and regulation, supported by 20 regulatory instruments.
2.18 Policy and administrative responsibility for the legislative package is spread across Health and Human Services, and the relevant regulators—APRA and ASIC, within the Treasury portfolio.
2.19 The key pieces of legislation governing the Indemnity Insurance Fund’s administration and payments are the Medical Indemnity Act 2002 and the Midwife Professional Indemnity (Commonwealth Contribution) Scheme Act 2010. Details of primary legislation and allocated administrative responsibilities are set out in Appendix 3.
Longer term strategy for assessing government support
2.20 The government consulted widely when establishing the initial support measures; the Review Panels were convened (see paragraphs 2.1, 2.11 and 2.14) and review processes were in place for the first five years after the package of measures were implemented. The 2007 Review Panel was forward looking, recommending the establishment of a stakeholder forum (see paragraph 2.14) and on-going monitoring of the High Cost Claims Scheme to ensure ‘…it continued to be effective as a means for bringing about stability’ and tort law reform in States/Territories ‘…with particular reference to the impact of the reforms on the cost of medical indemnity insurance’. While the 2007 Review Panel noted it was too early to review some of the measures and therefore did not recommend a subsequent formal review, it did note that the stakeholder forum should ‘…refer matters as appropriate, including to a higher level policy forum’.34
2.21 An evaluation strategy was never developed and while a target of up to five years was set for medical defence organisations to meet APRA’s regulatory (capital) requirements,35 other key performance or impact metrics were not established to assist in determining, at a future point, when the market was stabilised, premiums were assessed as affordable, insurance was considered to be available. In this regard, a broader exit strategy for winding back government intervention was not defined.
Did the design of the Indemnity Insurance Fund schemes promote stability, availability and affordability of medical indemnity and professional indemnity?
Overall, the financial strength of the medical indemnity insurance market has improved significantly since the Indemnity Insurance Fund schemes and Australian Prudential Regulation Authority’s regulatory oversight were introduced in 2002. In the years following the government’s response, net assets and capital holdings of insurance providers has improved markedly, with providers’ market share also largely stabilised.
Since 2003–04, there have also been improvements in the affordability of average insurance premiums paid by most medical specialities. Professional indemnity insurance for midwives continues to be available.
2.22 The final reports from the Review Panel36 and the ACCC37 indicated that the design of the schemes, in conjunction with regulatory oversight and tort law reform, had improved the industry stability and the affordability and availability of medical indemnity cover.38
2.23 In 2002, prior to the introduction of regulatory oversight, the medical indemnity insurance industry reported a very low net asset position of $11 million and was struggling to cover its liability position of approximately $1750 million.39 APRA’s regulatory requirements included that insurers must have a minimum capital holding of 150 per cent of projected liabilities.40
2.24 Over the following two years, net assets of the industry improved rapidly, increasing to $119 million in 2003, and then to $280 million in 2004.41 In 2009, the ACCC reported that all of the insurers had exceeded APRA’s minimum capital requirements.42 In particular, the ACCC’s 2009 report also indicated that the solvency position across the five medical indemnity insurers43 was strong with total assets exceeding total liabilities by $619 million.44
2.25 The ANAO’s analysis of the industry’s market share of medical indemnity insurance, by premium revenue and by number of policies held as at 30 June 2015, showed that while Avant Insurance was the dominant provider, other insurers also held significant market positions (see Figure 2.2 below). ANAO analysis suggests that market share has been relatively stable over time.
Figure 2.2: Market concentration comparisons

Source: ANAO analysis of 2015 Annual Reports published by medical indemnity insurers.
2.26 The ACCC’s 2009 report indicated that average premiums—as a share of private income, were well below the 30 per cent level that some specialities were paying in the early 2000s.45 The ANAO’s analysis indicated improvement in the affordability of medical indemnity insurance premiums over time, with average premiums across a range of specialities either flat or having fallen. (See Figure 2.3 below).
Figure 2.3: Average premiums for medical indemnity insurance, by specialty, before the Premium Support Scheme subsidies
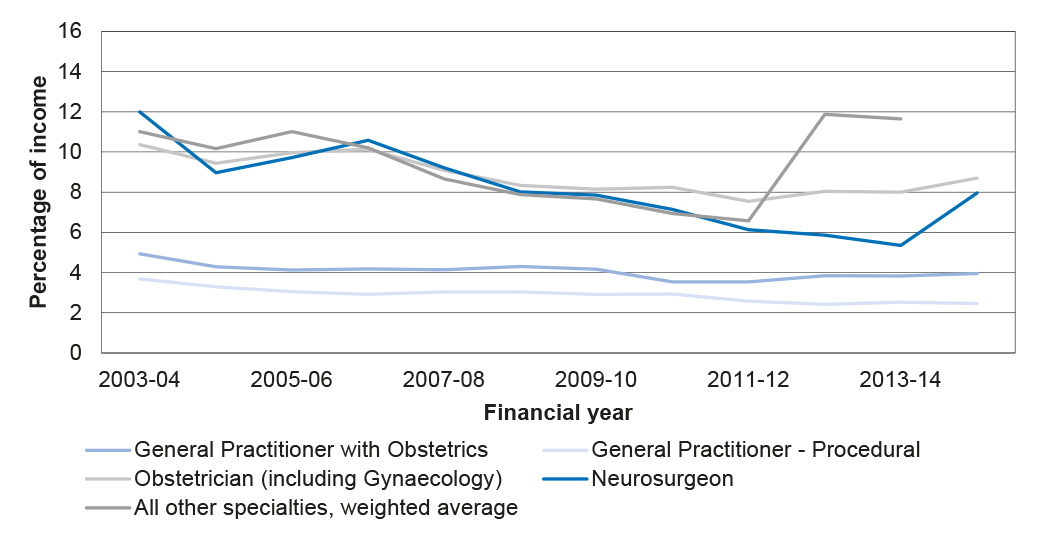
Source: ANAO analysis of Human Services’ data.
2.27 Similarly, in February 2014, the National Commission of Audit noted that there was evidence that the market was normalising, with a decline in average premiums since 2003 with net assets and reported profits in the industry increasing.46
2.28 The measures put in place by the Australian Government also supported the availability of insurance for practicing midwives, with consideration of affordability built into the design of the Midwife Professional Indemnity Scheme, with a cap of $7500 set on premiums. This is further discussed in paragraph 2.88.
Does Health monitor the performance of relevant insurers and the market?
The Department of Health does not have an effective monitoring arrangement in place or a strategy for consulting stakeholders to support its policy and administrative responsibilities for assessing the stability of the indemnity insurance market. Information received by the Department of Health on professional indemnity insurance for midwives is also limited.
2.29 Health’s Flexible Fund Guidelines: Indemnity Insurance Fund (IIF Guidelines) are publically available on its website and set out administrative details on the roles and responsibilities of the Minister for Health, including that the Minister was responsible for reviewing and setting Fund priorities.47 The IIF Guidelines further state that ‘these priorities will at all times reflect the aims and objectives of the Fund, but may change over time to address emerging issues that will support more effective indemnity insurance schemes’.48
2.30 Under the IIF Guidelines, Health is responsible for monitoring the operations and activities of medical indemnity insurers, regularly monitoring the industry, and liaising with medical indemnity insurers about their cost structures.49 More detail on the IIF Guidelines is discussed in paragraphs 3.29–3.31.
Stakeholder Forum
2.31 In response to the Medical Indemnity Policy Review Panel recommendation that a stakeholder forum be established to monitor medical indemnity measures (see paragraph 2.14),50 the Medical Indemnity Insurance Association of Australia (MIIAA) suggested to Health that its existing quarterly meetings with insurers and the Australian Medical Association could ‘…fulfil the requirement of a stakeholder forum with some minor changes’. Health agreed, noting that ‘…this would be a good feedback loop for government and that you [the MIIAA] intend to provide the Department with six monthly reports on the discussions you have’. Health further indicated to MIIAA that it wanted to be kept advised about further developments.
2.32 Health advised the ANAO that the stakeholder forum was established and teleconferences were ‘…held regularly through the transition period’. The MIIAA consulted stakeholders including for its half-yearly reports to the (then) Department of Health and Ageing on issues raised during the stakeholder forum.51 From 2007 to 2010, the MIIAA also held annual medical indemnity forums. Health officials had not attended the stakeholder or the annual medical indemnity forums in recent years and were unable to advise when attendance ceased, or provide any records of these stakeholder discussions, such as forum agendas, meeting outcomes or half yearly reports.52
Other monitoring arrangements
2.33 Health’s monitoring arrangements for medical indemnity include the AGA’s annual reports (see paragraph 2.61) providing information on:
- the Run-off Cover Schemes for medical indemnity and professional indemnity for midwives (a legislative requirement);
- an actuarial review of liabilities for Run-off Cover Schemes, the HCCS, the Exceptional Claims Scheme (ECS) which was principally for the purposes of annual Budgets, and Health’s financial statements; and
- ad hoc requests for advice on claims and liability estimates.53
2.34 The AGA reports and ANAO’s analysis indicates that the actuarial projections, provided by insurers to the AGA (via Human Services), had limitations:
- the data only includes claims against the High Cost Claims Scheme rather than for all claims, limiting the AGA’s capacity to monitor claims over time that may potentially become high cost;
- inconsistencies in the data collected, for example, insurers did not use the same list of medical practitioner specialty codes when providing claims data; and
- the AGA’s 10 reports on the Run-off Cover Scheme for medical indemnity insurers covering the period from 2004–05 to 2013–14 indicate that there were discrepancies and inconsistencies in the data provided by medical indemnity insurers.54
2.35 Health was also unable to demonstrate that it had ever used the APRA National Claims and Policies Database for monitoring and reporting purposes. In July 2016, Health advised the ANAO that it had re-engaged with APRA to discuss data sharing and analysis.
2.36 The ANAO identified scope for improving the quality and quantity of data provided by insurers for Health to better inform the minister responsible for reviewing and setting the IIF priorities.
Auditing the Indemnity Insurance Fund schemes
2.37 According to the IIF Guidelines, Human Services is responsible for the payment and audit of funds expended under the IIF schemes.55 Human Services advised the ANAO that the IIF compliance function moved to Health in September 2015, following machinery of government changes. Health advised the ANAO that Human Services maintained responsibility for the payment and quality assurance of medical indemnity payments, while Health is responsible for broader audits of Indemnity Insurance Fund schemes, including the audit of medical indemnity insurers and Medicare providers where required.
2.38 In 2006–07, Human Services audited selected payments against claims made by five medical defence organisations under the IIF schemes. Other audits conducted have included:
- a 2008 internal audit of the Incurred-But-Not-Reported (IBNR) Scheme; and
- an April 2010 external audit that reviewed the key processes and controls in place to administer the IBNR Scheme, on behalf of Health.
2.39 In September 2011, a broader internal audit—Program Integrity Review of Medicare Australia’s Administration of the Medical Indemnity Program, was conducted. Recommendations from the Program Integrity Review included that a comprehensive risk-based compliance audit on the program be considered. The ANAO was advised by Human Services that its Compliance Division did not rank the programme risk high enough to perform an audit at that time.
2.40 Health has not undertaken any internal or externally commissioned audits of the performance or administration of the IIF schemes.
Monitoring the stability of the medical indemnity insurance market
2.41 The IIF Guidelines state that ‘to ensure the ongoing stability of the medical indemnity industry, the department [Health] will continue to monitor the operations and activities of medical indemnity insurers’.56
2.42 Evidence from third party monitoring processes suggest that, following implementation of the government’s reform package, the medical indemnity insurance market stabilised relatively early, and market failure dissipated (see paragraphs 2.24–2.26). The ACCC’s final report in 2009 noted that ’… insurers are in a much stronger capital position compared to when they were established, moving away from an objective of raising capital to maintaining capital’.57
2.43 Moreover, when reporting to its Minister prior to the release of the Medical Indemnity National Collection report Australia’s medical indemnity claims 2010–11 in 2012, Health advised its Minister that ‘the report reinforces the view that the medical indemnity industry had stabilised in the last few years following a period of relative instability’.
2.44 In addition to the ANAO’s analysis of insurers’ market share in 2015 (see Figure 2.2), the ANAO’s additional analysis of relevant insurers’ recent financial positions—including the Medical Insurance Group Australia (MIGA)—as the sole supplier of midwives’ indemnity insurance, is outlined in Table 2.1.
Table 2.1: Key measures of relevant indemnity insurers’ profitability
|
|
|
2013 |
2014 |
2015 |
|
Net Revenues |
$m |
$m |
$m |
|
|
Avant |
195.3 |
212.5 |
230.1 |
|
|
MDA National |
– |
58.3 |
58.8 |
|
|
MIGA |
23.5 |
36.3 |
38.8 |
|
|
Medical Indemnity Protection Society (MIPS) |
97.7 |
85.1 |
94.4 |
|
|
Total |
316.5 |
392.2 |
422.1 |
|
|
Profits |
|
|
|
|
|
Avant |
115.7 |
107.5 |
66.1 |
|
|
MDA National |
– |
11.1 |
14.9 |
|
|
MIGA |
11.9 |
2.2 |
4.6 |
|
|
Medical Indemnity Protection Society (MIPS) |
33.4 |
35.4 |
20.2 |
|
|
Sum |
161.0 |
156.2 |
105.8 |
|
|
Capital multiples |
rate |
rate |
rate |
|
|
Avant |
2.93 |
2.92 |
2.16 |
|
|
MDA National |
– |
– |
– |
|
|
MIGA |
3.11 |
3.17 |
2.83 |
|
|
Medical Indemnity Protection Society (MIPS) |
4.43 |
4.90 |
4.67 |
|
Note a: Blanks denote where data is unavailable. Net revenue for MIPS refers to total income, as data on net earned premium is not provided. MIPS data provided on Total Comprehensive Income for the Year excludes expenses, which is not equivalent to net revenue.
Source: ANAO analysis of the annual reports of insurers.
2.45 While some insurers had posted declining profits in more recent years, capital adequacy multiples for all insurers are in excess of two—well above capital requirement levels set by APRA.58
2.46 Insurers have also considerably strengthened their net asset position over time. The ANAO’s analysis indicates that in 2015, medical indemnity insurers reported net asset holdings of $1935 million across the four active insurers, rising from an estimated $619 million59 across five insurers (including QBE Insurance Group) in 2009.
2.47 While Health reports annually against a number of Key Performance Indicators (see Table 3.1), since its 2012 Medical Indemnity National Collection report to its Minister, Health had not otherwise analysed or reported on the stability of the indemnity insurance market.
Monitoring the availability of professional indemnity insurance for midwives
2.48 Health and Human Services have a contract with MIGA to provide professional indemnity insurance to eligible privately practicing midwives (see paragraph 3.3).60 MIGA was the only provider of professional indemnity insurance to midwives in the Australian market.61 Under this contract, Health established monitoring arrangements with MIGA reporting annually on:
- the number of policy holders and premium information;
- marketing activities of the insurer;
- take-up rates and evaluation of education and risk management activities provided by MIGA; and
- claims notifications and advisory support.
2.49 Human Services advised the ANAO that there were 130 eligible midwives that held policies as at 31 December 2015. There are significantly less midwives participating in the midwife professional indemnity scheme than the 700 midwives originally forecast to be practicing nationally by the end of the third year of the scheme.
2.50 Health does not have any other monitoring arrangements in place for the market or insurance for eligible midwives.
Does Health review and report on the Indemnity Insurance Fund’s performance and risks, including to its Minister?
To date, the Department of Health has not reviewed or evaluated the Indemnity Insurance Fund legislation, supporting regulatory and other legal reforms, or the schemes’ financial assistance packages for their impact on the availability and affordability of indemnity insurance. The Department of Health’s reporting to its Minister on the Indemnity Insurance Fund’s performance and risks are largely ad hoc and driven by external processes, for example, annual Budget requests to bring forward savings. Overall, the Department of Health’s arrangements for review, analysis and advice to its Minister on the Indemnity Insurance Fund schemes, including risks and performance against the Indemnity Insurance Fund’s objectives and priorities, is limited.
2.51 Health provides overall policy and programme support and advice to the Minister and was responsible for the policy development and administrative oversight of the indemnity insurance schemes.62 Under the programme agreements between Health and Human Services, Health was responsible for maintaining and reviewing the legislation supporting the IIF to ensure that legislation supports the policy intent.63
Arrangements established to review indemnity insurance
Reviewing Indemnity Insurance Fund legislation
2.52 In December 2015, Health received its Minister’s agreement to request approval to align sunsetting clauses for 15 of the medical indemnity legislative instruments until 1 October 2019 (five of the 15 legislative instruments were due to sunset between 1 April and 1 October 2016) to allow for a thematic review of the legislation.64 The purpose of the review was ‘to consider the relevant pieces of legislation as a whole, with a view to simplifying and streamlining the legislation, with a particular focus on deregulation.’
2.53 Approval to align the sunset clauses was provided by the Attorney-General’s department on 11 February 2016. Health advised that the thematic review is planned to commence following the Mid-year Economic and Fiscal Outlook 2016–17.
2.54 As no comprehensive review of the IIF-related legislative package had been undertaken to date, the thematic review and its findings, once available, should also be considered in the context of the recommendations in this audit report.
Review of regulatory and other legal reforms
2.55 As discussed in paragraph 1.6, in addition to relevant IIF subsidy schemes, a number of regulatory and legal reforms were implemented to support the stability and availability of medical indemnity insurance in the early 2000s.65
2.56 Broader actuarial sector and ACCC’s reviews indicated that the reforms had a positive impact. In November 2004, United Medical Protection (UMP) indicated that its insurer, Australian Medical Protection Limited ‘…would make significant reductions in premiums for 2005’ on the basis of a number of factors including medical indemnity and extensive tort law reforms. In 2005, the ACCC made a positive assessment of the short term impact of tort law reform, observing that: ‘…the majority of insurers took tort law reform into account in setting their aggregate premium pools for 2005–06’.66
2.57 In December 2006, the Minister for Revenue and Assistant Treasurer reported that the positive impact of regulatory intervention noting that ‘…the changes made to the laws of negligence across Australia have had a positive impact on the availability and affordability of public liability and professional indemnity insurance’.67 This 2006 report also noted that the government’s medical indemnity assistance package, which included regulatory reform, had resulted in a reduction in premiums. It added that the expected flow-on effects from the impact of increased risk management practices, after tort law reforms were introduced, would be seen in the long term.
2.58 Since 2006, Health has not reviewed or reported on the impact of the related regulatory interventions on the market to the government or its Minister.
Commissioned reviews
2.59 In 2011, Health commissioned an internal review of ‘…selected information and data presented publicly in the ACCC reports’, which included an overview of the IIF schemes, analysis on trends in costs and premiums and the commercial justification of premiums. This 2011 review confirmed that ‘…the medical indemnity insurance industry remains in a sound financial condition …’
2.60 Since 2011, there have been no further reviews commissioned. Health advised the ANAO that its focus had centred on the annual Budget process. Health also has not developed an evaluation strategy or undertaken a broader impact evaluation of the IIF-related reforms and financial assistance package.
Reporting on Indemnity Insurance Fund risks and performance
Parliamentary reporting on the Run-off Cover Schemes
2.61 The AGA reports annually to Health on the Run-off Cover Schemes for medical indemnity and midwives.68 Under s. 34ZW of the Medical Indemnity Act 2002 and s. 48 of the Midwife Professional Indemnity (Commonwealth Contribution) Scheme Act 2010, the Minister was required to request the AGA to prepare advice and report on the Run-off Cover Schemes for medical indemnity and midwives within 6 months after the end of the financial year and table the reports in the Parliament within 15 sitting days after receipt of the reports. Generally, Health briefs its Minister ahead of this tabling. Figure 2.4 shows the gap in tabling of the AGA reports from 2004–05 to 2013–14.
Figure 2.4: Tabling of Australian Government Actuary reports in Parliament: time between reporting period (end of financial year) and actual tabling (months)
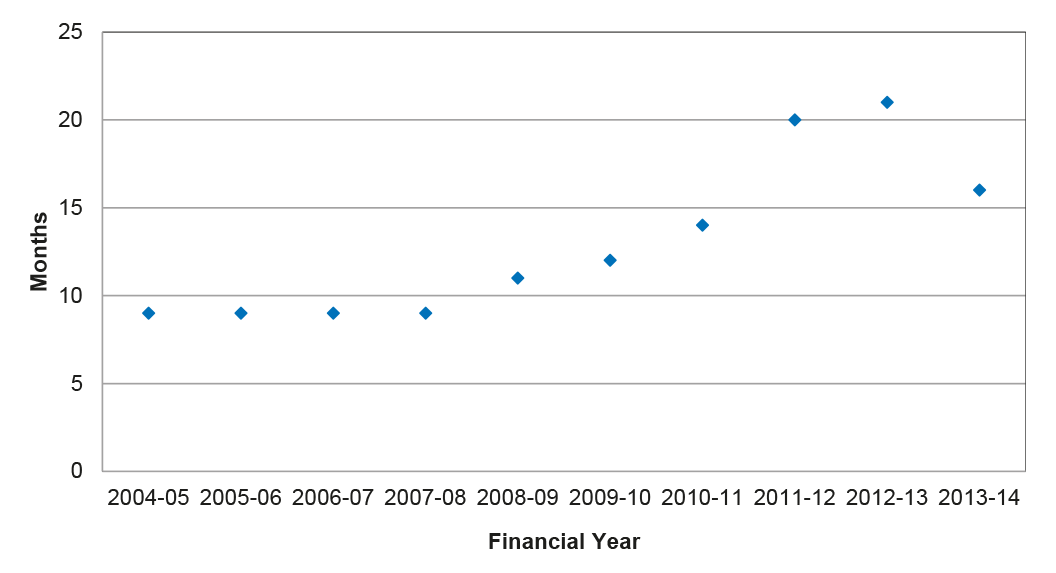
Source: ANAO analysis.
2.62 As illustrated in Figure 2.4, the time between actual tabling of the AGA reports and the relevant periods they cover has increased progressively since the 2007–08 report, with Report Number 9 tabled in March 2015, some 21 months from the end of the 2012–13 data period.
2.63 The cost of the Run-off Cover Schemes (ROCS) was met over time by a ROCS support payment paid by insurers to the government; in this way, the Run-off Cover Schemes are designed to be cost neutral to the government. The AGA’s 2013–14 report noted that the total ROCS revenue for medical indemnity insurers (from the insurers’ support payments) to date was greater than the government’s liabilities in ROCS.69 However, AGA further notes that claims are ‘…lumpy in nature’ and ‘volatile’ and there was uncertainty related to liabilities the government faces.70 In addition to its legislative requirements, this ongoing uncertainty of ROCS liabilities heightens the need for Health to provide timely advice to its Minister.
The Department of Health’s reporting to its Minister
2.64 Since 2010, apart from briefing its Minister on the AGA’s Run-off Cover Schemes reports and the now ceased Australian Institute of Health and Welfare’s Medical Indemnity National Collection reports (see paragraph 2.7), Health’s advice to the government and its Minister over time was focussed on:
- administrative matters, including: the renewal of the Premium Support Scheme contracts and the midwives scheme contract; and advising the Minister when insurers notify Health that they are exiting the market or potentially entering the medical indemnity/professional indemnity (midwives) market; and
- related Budget proposals over time, including:
- the consolidation of the schemes into the IIF as part of the 2011–12 Budget;71
- the phased reduction in the PSS subsidy rate from 80 to 70 cents in the dollar as part of the 2012–13 Budget;
- similar PSS subsidy reductions in the 2013–14 Budget, which reduced the subsidy to 60 cents in the dollar;
- a proposal to further reduce the PSS subsidy rate to 55 cents in the dollar, to be considered following negotiations with the medical profession. Following Health’s advice, the government agreed no further changes to support for medical indemnity would occur before the 2015–16 Budget;
- the government’s consideration of a scale back of its medical indemnity subsidies as part of the 2015–16 Budget. Again, following Health’s advice, the government agreed to delay further changes until the 2016–17 Budget; and
- as part of the 2016–17 Budget, Health advising the government to defer options to reduce the level of government involvement in the medical indemnity insurance industry, noting the uncertainty with the proposed medical injury stream of the no fault National Injury Insurance Scheme (NIIS).72
2.65 Health advised the ANAO that any proposed review or change to the IIF schemes is dependent on the NIIS. The Department of the Treasury (Treasury) had policy responsibility for the NIIS. Health met with Treasury on medical indemnity insurance and the NIIS issues on 17 February 2016, at a meeting with insurance providers. At this meeting, Treasury noted that it is working with the states and territories on developing the medical treatment injury stream of the NIIS and will be reporting back to the Council of Australian Governments at the end of 2016.
2.66 In February 2014, the National Commission of Audit recommended that the Commonwealth scale back its subsidies for medical indemnity insurance and reported that there was evidence that the market was normalising—average premiums had declined since 2003 to become more affordable and net assets and reported profits in the industry had increased. The government’s response to the National Commission of Audit report was that ‘Reforms to Medical Indemnity will be considered following the 2014–15 Budget’.73
2.67 Health did not provide any written advice to its Minister on the 2014 National Commission of Audit findings, although Health advised the ANAO that it did brief its Minister orally on 5 December 2014 as part of Budget processes and also on 19 January 2015, as part of incoming Minister discussions. Health did not though advise its Minister more broadly on the IIF schemes, including on risk and performance against the IIF’s objectives and priorities.
Reporting on medical indemnity insurance premium affordability
2.68 One of the priorities of the IIF was to ensure that medical indemnity insurance premiums are affordable for medical practitioners.74 Two schemes had an effect on premium affordability: the Premium Support Scheme (PSS) and the High Cost Claims Scheme (HCCS).
Premium Support Scheme
2.69 As noted in paragraph 1.11, Health administers the PSS contracts with each insurer. These contracts define the parameters of the PSS and identify the specific payments to insurers for costs associated with their roles in administering the PSS. There were 1597 participants75 in the PSS in 2013–14; 1496 in 2014–15; and 1177 in 2015–16. In general, the PSS provides a subsidy for medical practitioners where their insurance premium was calculated to be more than 7.5 per cent of their income.76
2.70 As noted in paragraph 2.26, the ANAO’s analysis indicates that average premiums had generally fallen over time for a range of medical practitioner specialities. Table 2.2 sets out further ANAO analysis on premium affordability, including details of medical practitioners receiving the PSS subsidy, average incomes, and the average premium before and after the subsidy.
Table 2.2: Participation levels and impact of the Premium Support Scheme, 2013–14(a)
|
Specialty |
Doctors in PSS |
PSS cost per doctor |
Private income |
Premium set by insurers, prior to PSS subsidy |
Premium, including PSS subsidy |
||
|
|
|
$ 000 |
$ 000 |
$ 000 |
Per cent of income (b) |
$ 000 |
Per cent of income |
|
GP with obstetrics |
177 |
8 |
383 |
15 |
4 |
7 |
2 |
|
GP procedural |
531 |
3 |
309 |
8 |
3 |
5 |
2 |
|
Obstetrician(c) |
293 |
15 |
695 |
56 |
8 |
41 |
6 |
|
Neurosurgeons |
45 |
11 |
878 |
47 |
5 |
36 |
4 |
|
Other specialities(d) |
551 |
2 |
85 |
10 |
12 |
7 |
9 |
Note a: Data for 2013–14 used, as income data for 2014–15 was incomplete.
Note b: Significant proportions of these speciality groups continue to receive PSS subsidies due to MISS grandfathering arrangements.
Note c: Includes gynaecology.
Note d: Weighted average across all other specialities.
Source: ANAO analysis on Human Services’ PSS data.
2.71 For 2013–14, on average, initial premiums set by insurers were generally less than 10 per cent of income. While there was no agreed benchmark for the proportion of a medical practitioner’s income that should be allocated to insurance, rates of 10 per cent have been noted internationally.77 After the PSS subsidy, the majority of average 2013–14 premiums fell below 7.5 per cent. Other observations include:
- the average premium for procedural General Practitioners, before the PSS, was low, between two and four per cent of income;
- the average premium for neurosurgeons, before the PSS is applied, had dipped to below 7.5 per cent of average income. Despite this, 22 per cent of the number of doctors who were receiving a subsidy under the PSS in 2013–14 (1597 doctors) continue to receive PSS subsidies, largely due to a greater proportion of neurosurgeons (compared to all other specialists) still qualifying for a subsidy through the Medical Indemnity Subsidy Scheme;78
- the average premium for General Practitioners with obstetrics had been persistently below the 7.5 per cent cut-off; and
- currently medical practitioners operating in rural areas are eligible for the subsidy regardless of whether their premium exceeds the 7.5 per cent income threshold. However, ANAO analysis shows that most medical practitioners in rural areas are General Practitioner proceduralists who generally face the lowest average premiums.79
2.72 Separately, the ANAO identified that, for PSS eligibility purposes, rural areas are those defined in accordance with the Rural, Remote and Metropolitan Areas 3-7 (RRMAs) which was based on 1991 data. The ANAO’s analysis indicated that some health programs define rural areas using the more current Modified Monash Model, for example, the General Practice Rural Incentive Program.80 Under the Modified Monash Model, some PSS participants may no longer be classified as rural.
2.73 Under the memorandum of understanding between Health and the AGA, the AGA will, if requested, provide actuarial advice on the PSS. While the AGA received data from Human Services on premiums, Health had not asked the AGA to provide any advice on the affordability of premiums.
2.74 Health does not regularly analyse the PSS data, or review premium affordability and whether the scheme was appropriately targeted in line with the original policy intent. Health had used the PSS data to review select policy parameters, on an ad hoc basis, for example, the assessment of rural areas—although this analysis was not conveyed to its Minister.
2.75 In contrast to Health’s role in the private health insurance market, there were no oversight arrangements in place in the medical indemnity insurance market to review and assess premiums and the impact of the PSS on Commonwealth outlays over time.81
High Cost Claims Scheme
2.76 Premium affordability was also affected by the HCCS. The HCCS reduced insurers’ costs by reducing the payout normally borne by insurers for high cost claims. In a relatively competitive market, the HCCS subsidy would generally be factored into the premium rates set by insurers, and would therefore have the effect of reducing premiums. In 2009, the ACCC noted that ‘…all insurers appropriately considered HCCS and ROCS in their premium determinations’.82
2.77 Health has not undertaken any analysis or provided advice to its Minister on the impact of the HCCS on premium affordability since the reduction to the HCCS threshold amounts in 2004.
2.78 Using 2013–14 data on neurosurgeons as an example83, the ANAO’s analysis indicates that premiums for neurosurgeons would have been around one per cent higher, as a proportion of their income, without the HCCS, shown in Figure 2.5.
Figure 2.5: Impact of the High Cost Claims and Premium Support Schemes on premiums paid by neurosurgeons for medical indemnity insurance as a percentage of income
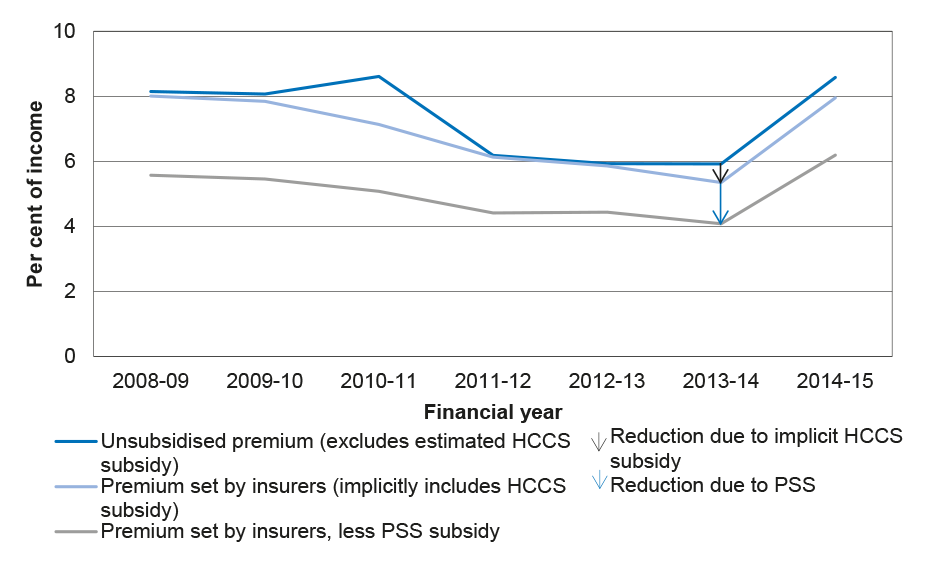
Note: Assumes the average impact of the HCCS on premiums is the HCCS payout in a year proportionate to the number of medical practitioners.
Source: ANAO analysis of Human Services’ data.
2.79 In 2006, the AGA advised the Medical Indemnity Policy Review Panel (the Review Panel) that an increase in the High Cost Claims threshold would result in savings for the government. In 2007, the Review Panel reported that the HCCS was still in its infancy, and it was difficult to estimate the impact of any change in the threshold. The Review Panel further advised the government that at that time, the HCCS should continue to operate for several years without change, and be monitored by the ACCC over the period.
2.80 The $300 000 minimum threshold for a high cost claim had not been reviewed since 2004. Over time, the policy intent of the HCCS had potentially been eroded because the threshold had not been subject to indexation. In this context, and all other things being equal, a number of claims would not have been considered to be high cost had inflation been considered through an appropriation indexation rate. For example, if the $300 000 threshold had increased in line with average weekly earnings (AWE), then $300 000 in 2005 would be valued at $439 000 in 2015. In this scenario, the government now bears the cost of those claims between $300 000 and $439 000 in 2015, due to inflation alone.
2.81 The ANAO’s analysis indicates that had the HCCS minimum threshold for the HCCS been subject to annual increases in line with AWE, 27 per cent of the HCCS claims paid by the government in 2015 would not have been eligible. The ANAO’s further high level analysis of HCCS data on expected payments made to insurers from 1 July 2004 suggests that approximately $33 million of the anticipated $190 million cost of the HCCS would have been saved by indexing the threshold based in line with AWE.84
Reporting on increasing High Cost Claim Scheme liabilities and risks to government
2.82 The overall financial exposure and risk to government is increasing over time, as the number of large claims ($550 000 and above) under the HCCS grows over time. The ANAO’s analysis of the government’s increasing financial and risk exposure is set out in Figure 2.6.
Figure 2.6: Growth in High Cost Claims Scheme large claims over time

Source: ANAO analysis of Human Services’ HCCS data.
2.83 The government’s growing liability associated with the HCCS is further illustrated in Table 2.3, which sets out for the period from 2004 to 2015:
- HCCS payments to insurers;
- estimates of remaining claim payments, known as the reported incurred cost (RIC);
- estimates of the expected final claims settlement costs; and
- estimates of the increases over time, associated with large claims. In this regard, the gap between the RIC (the third column) and estimated settlement costs (fourth column) is known as the Incurred But Not Enough Reported (IBNER). For HCCS purposes, the IBNER relates to any claim that will ultimately settle above the $300 000 threshold.
Table 2.3: High Cost Claims Scheme payments to insurers
|
Notification Year |
HCCS Paid to Date as at 30 June |
Reported Incurred Cost |
Estimated Settlement |
IBNER |
|
|
$million |
$million |
$million |
(%) |
|
2004 |
13.928 |
15.688 |
18.089 |
15.3 |
|
2005 |
21.854 |
35.983 |
37.362 |
3.83 |
|
2006 |
19.346 |
21.915 |
21.590 |
-1.48 |
|
2007 |
16.223 |
20.818 |
25.397 |
22.00 |
|
2008 |
25.289 |
34.576 |
40.321 |
16.62 |
|
2009 |
25.784 |
37.196 |
44.974 |
20.91 |
|
2010 |
16.169 |
28.329 |
29.209 |
3.11 |
|
2011 |
17.988 |
32.793 |
41.072 |
25.25 |
|
2012 |
13.951 |
26.851 |
46.065 |
71.56 |
|
2013 |
13.653 |
38.440 |
49.856 |
29.70 |
|
2014 |
5.146 |
38.826 |
66.509 |
71.30 |
|
2015 |
4.184 |
30.008 |
54.683 |
82.23 |
|
Total |
193.516 |
361.424 |
475.128 |
N/A |
Source: ANAO analysis of Human Services’ data on claims and liabilities.
2.84 Some of the claims presently below the $300 000 threshold will become large over time. These potential HCCS claims are not presently included in the data provided to Human Services under the Scheme’s contracts with insurers. Where there was a significant gap between the RIC and the actuarial estimate, there was greater uncertainty surrounding the numbers of large claims. To be able to reasonably forecast the number of large claims, additional data85 would be required.
2.85 Unlike the self-funding model for the ROCS, insurers make no contribution to offset the cost of the HCCS. In addition, the government bears 50 per cent of the liability for large claims up to $20 million, rising to 100 per cent for those claims above this, through the Exceptional Claims Scheme (ECS). Given the volume of large claims from 2011 onwards where the estimated settlement was at least 25 per cent or greater than the RIC, it would be expected that the number of large claims would continue to increase from the number known today. In this regard, the government would face increasing exposure to risk (and financial cost) over time.
2.86 Consistent with its policy and Fund oversight responsibilities, Health should undertake further analysis to fully assess the government’s risk exposure with respect to the HCCS and the ECS, and report on risk mitigation options to its Minister, including options for containing this increasing financial risk.
Reporting on the availability and affordability of Midwife Professional Indemnity Scheme
2.87 The availability of professional indemnity insurance (PII) for eligible midwives was one of the IIF’s priorities. Although affordability of PII premiums for midwives was not an identified priority for the IIF, the IIF Guidelines note that the Minister would review the priorities ‘…to address emerging issues that will support more effective indemnity insurance schemes’.86
2.88 ANAO analysis of premium information in the MIGA reports shows that the method of calculating premiums changed from 2011–12 to 2012–13. Premiums had always been capped at $7500 for midwives. However, in 2010–11 and 2011–12, the level of premiums was determined on the basis of the number of women (and their babies) receiving midwifery services. From 2012−13, the determination of premiums was on the basis of gross income, bringing it more into line with the PSS.
2.89 The ANAO analysed premiums paid by midwives for indemnity insurance from 2013–14, as outlined in Table 2.4.
Table 2.4: Midwives premiums as a proportion of income
|
Gross income band of midwife |
Option A annual premium (providing intrapartum care) |
Option B annual premium (no intrapartum care) |
Premium as a proportion of gross income -Option A (%)(a) |
Premium as a proportion of gross income -Option B (%)(a) |
|
$90,000 or higher |
7500 |
3400 |
8.3 |
3.8 |
|
$70,000– $89,999 |
6500 |
3000 |
9.3 |
3.3 |
|
$50,000– $69,999 |
5000 |
2250 |
10.0 |
2.5 |
|
$25,000– $49,999 |
3375 |
1530 |
13.5 |
1.7 |
|
Less than $25,000 |
2400 |
1350 |
9.6 |
1.5 |
Note a: The proportion is calculated on the minimum amount of gross income the premium level applies to.
Source: ANAO analysis from MIGA 2013–14 and 2014–15 annual reports to Health.
2.90 For those privately practicing midwives who do not provide intrapartum care (while the woman is in labour), premiums are 3.8 per cent or below as a proportion of their gross income. For midwives who do provide intrapartum care, premiums are much higher. For instance, midwives earning $25 000 per annum pay 13.5 per cent of their gross income on PII, whereas midwives earning between $25 000 and below $33 750 pay over 10 per cent of their income on PII.
2.91 To be able to advise its Minister on this and related matters, Health would need to obtain additional data from insurers, and then undertake further analysis to assess the affordability of PII. This analysis may include an assessment of the impacts of the Midwives Professional Indemnity Scheme.
Summary
2.92 Since 2003, the IIF and related financial support schemes (including the relevant midwives’ schemes) were established to address market failure in the indemnity insurance sector and rising premiums for medical professionals and midwives (from 2010). The IIF and its schemes had not been fully evaluated since that time, nor have the IIF’s overall priorities been assessed or reviewed. There had also been no assessment of the impacts of current regulatory arrangements and the need for, or extent of, any on-going government intervention. This needs to be addressed in light of the ANAO’s findings which highlight that:
- the existence and extent of market failure in the contemporary medical indemnity insurance market has dissipated over time;
- the financial position, including solvency, of medical indemnity insurers was stable with 2015 annual reporting showing net assets of approximately $1935 million across the four active insurers;
- premiums for medical indemnity insurance, both in absolute terms and as a share of income, had been falling or had been generally flat since the early 2000s; and are now generally affordable for most medical practitioners;
- premiums for some midwives are high;
- HCCS payment thresholds had not been reviewed since 2004, and any analysis would benefit from access to more complete and quality assured data; and
- Health’s monitoring, analysis and reporting arrangements on the government’s financial and risk exposures, especially with respect to the HCCS and ECS, is limited.
Recommendation No.1
2.93 The Department of Health should conduct a ‘first principles review’ of the Indemnity Insurance Fund and related schemes prior to the 2017–18 Budget.
Health’s response: Agreed with qualification.
2.94 The department agrees there is benefit in conducting a ‘first principles review’. However, the scope, timing and resourcing of such a review, will be a decision for the Australian Government.
Recommendation No.2
2.95 Subject to the outcome of this ‘first principles review’, the Department of Health should develop and implement a fit-for-purpose monitoring and reporting arrangement for the Indemnity Insurance Fund, legislation, and related schemes that provides its Minister with timely, robust analysis of the Indemnity Insurance Fund’s performance and risks to government.
Health’s response: Agreed
3. Governance and administrative arrangements
Areas examined
This chapter examines the governance arrangements in place to support oversight and probity of the Indemnity Insurance Fund and its schemes and the effectiveness and efficiency of administrative arrangements between the departments of Health and Human Services. This chapter also considers whether suitable controls are in place to support the administration of payments, security of data, and management of key records.
Conclusion
The departments of Health and Human Services developed and documented bilateral management and administrative arrangements to support the delivery of the Indemnity Insurance Fund’s support measures. While these arrangements clearly set out each entity’s roles and responsibilities, the documented mechanisms for cross-entity risk management are not in place. Both entities’ internal and external guidance materials also need to be reviewed and updated.
There is scope for the entities to review and put measures in place to ensure that the information and data collected from insurers against the schemes is accurate and relevant to better inform actuarial assessments, risk analysis and the measurement and reporting of the performance of the schemes against the Indemnity Insurance Fund’s objectives. There is also a need for the entities to improve the relevancy and completeness of public and internal performance indicators, including implementing measures to monitor and report the actual cost to the government to administer the Indemnity Insurance Fund.
Areas for improvement
The ANAO has made two recommendations aimed at the Department of Health establishing suitable governance and stakeholder engagement arrangements, including risk management plans, and both the departments of Health and Human Services developing more suitable key performance indicators and ensuring adequate controls to support data integrity.
Are the Indemnity Insurance Fund’s governance arrangements fit-for-purpose?
The roles of the Australian Government entities, including contracted insurers, for delivery of Indemnity Insurance Fund-related regulation and administrative responsibilities, are generally clear.
As the entity with overall responsibility for medical indemnity policy, the Department of Health had not established any regular intra-government or stakeholder engagement arrangements to coordinate or communicate Indemnity Insurance Fund-related policy and regulatory developments.
Coordination arrangements within the Australian Government
3.1 Increasingly, the outcomes sought by government for the community depend on the contribution of multiple parties, including public sector entities, other governments and entities, key non-government organisations and citizens.
3.2 As set out in Appendix 3, administrative responsibilities to support relevant legislation on the package of regulatory and financial measures are shared across Health and Human Services, and the Treasury portfolio (AGA, APRA and ASIC).
3.3 In addition to legislative responsibilities, the roles of Health and Human Services are clearly articulated in:
- the IIF Guidelines;
- the 2015–2018 Bilateral Head Agreement87, supported by two IIF-related programme agreements covering the medical indemnity and midwife professional indemnity schemes, respectively;88 and
- tripartite contracts established between Health, Human Services and medical indemnity insurers on the Premium Support and Midwives Professional Indemnity Schemes.
3.4 Within the Treasury portfolio, the AGA’s role was clearly articulated in a memorandum of understanding with Health to provide actuarial advice on the medical indemnity and professional indemnity for midwives schemes.
3.5 Other than established arrangements with Human Services (see paragraphs 3.18–3.22), Health did not have in place any regular coordination and engagement mechanisms with other government entities or the contracted insurers. Engagement with these parties was largely undertaken on an ad hoc basis.
Engagement with external stakeholders
3.6 Within Health, the Medical Benefits Division is responsible for the management and administration of the IIF. Health’s 2014–15 Business Plan outlined the key roles, objectives and responsibilities of the Division including, as a priority:
…ensuring that the medical indemnity insurance industry is affordable, stable and secure, and that medical indemnity products are affordable for doctors/midwives by monitoring the Australian Government programs and engaging with stakeholders to ensure the programs are meeting policy objectives.
3.7 Health has not developed an overarching communication or engagement strategy to support the administration and monitoring of the IIF schemes. Post the initial consultation supporting the development of the government’s support measures, engagement with external stakeholders had largely been intermittent—driven by specific developments or policy changes.
- In 2011, following the government’s decision to reduce the PSS rate, Health set out a stakeholder management approach, as part of its implementation strategy for this 2011–12 Budget measure. In this regard, Health attended a stakeholder meeting hosted by the Australian Medical Association (AMA) and requested submissions on potential impacts of the measure from the AMA and relevant insurance providers in early 2012.
3.8 Health advised the ANAO that it did not regularly consult with key medical or midwifery professional bodies on the IIF Schemes.
3.9 Dissatisfaction with the level of engagement was expressed by the stakeholder bodies consulted by the ANAO as part of this audit. Of particular concern was a lack of communication with these bodies post the government’s response to the National Commission of Audit’s 2014 recommendations, and in particular consultation on potential changes to any of the schemes.
3.10 In February 2016, Health hosted a meeting with insurers—with officials from Human Services and Treasury also attending. Discussions centred on the proposal for a National Injury Insurance Scheme89 and administration of the current measures.
Are suitable risk management arrangements in place?
There is no coordinated cross-entity risk management arrangements in place for medical indemnity matters, including the Indemnity Insurance Fund and related schemes.
Bilateral management arrangements for the medical indemnity programs between the departments of Health and Human Services are governed by joint agreements. However, no overarching bilateral risk management plans or formal arrangements have been established for the Indemnity Insurance Fund schemes.
The Department of Health did not have any risk management plans, including regular assessment, monitoring and mitigation arrangements in place for the Indemnity Insurance Fund schemes to support its Indemnity Insurance Fund related policy responsibilities.
The Department of Human Services have established suitable risk management plans and review arrangements to support its IIF-related administrative responsibilities.
3.11 As noted in paragraph 2.5, the design of certain IIF schemes, particularly the High Cost Claims and Exceptional Claims Schemes represented a significant financial risk transfer to the Commonwealth. In this context, there could be expected to be ongoing and active monitoring of risks associated with the Commonwealth’s continuing intervention in the insurance market. In addition, implementation of initiatives that involve other entities, state and territory bodies and non-government entities face increased risk management complexities.
3.12 Under the Commonwealth Risk Management Policy, entities are required to establish and maintain an appropriate system of risk management, oversight and internal control. In addition, this policy sets out that shared risks, that is those risks that extend beyond a single entity, require shared oversight and management. In this regard, accountability and responsibility for the management of shared risks may involve other sectors, community, industry or other jurisdictions. Under this policy, each entity is required to implement arrangements to understand and contribute to the management of shared risks.90
3.13 There was no coordinated cross-entity or shared risk management plan setting out oversight, and management and accountability responsibilities for medical indemnity and IIF-related matters. Health as the policy entity for medical indemnity should lead this development.
3.14 Under the 2015–18 Bilateral Head Agreement,91 the Joint Management Committee (at the Deputy Secretary level) is to agree and review the Risk Management Plan(s) and their operation. At the programme agreement level, the departments are to collaborate on compliance activities to effectively monitor and mitigate risks to the medical indemnity scheme. To date, there is no evidence of cross-entity or shared risk management plans or review activity relating to the medical indemnity schemes being developed or undertaken.
3.15 To support its own responsibilities, Human Services maintains a comprehensive IIF programme-specific risk management plan that is internally reviewed every 3–6 months. In contrast, Health does not have an equivalent.
3.16 Health advised the ANAO that it operates under its broader departmental Risk Management Policy. Health’s 2014–15 Business Plan identified high-level risks for the Medical Benefits Division (which administers the Fund within Health) and a standard set of mitigation measures. While not specifically addressing risks associated with the IIF, the Business Plan identified a need to ‘rebuild [corporate] knowledge about medical indemnity’. The allocation of risk between the various parties has not been considered or documented.
Recommendation No.3
3.17 That the Department of Health establish suitable governance and stakeholder engagement arrangements, including risk management plans, to support its and other shared responsibilities for the administration of the Indemnity Insurance Fund and related schemes.
Health’s response: Agreed
Are the administrative arrangements between the departments of Health and Human Services well-designed and operating effectively?
The bilateral agreements between the departments of Health and Human Services set out key administrative arrangements intended to support the operation and delivery of the Indemnity Insurance Fund schemes.
There is scope to improve the relevancy and completeness of the departments of Health and Human Services’ public and internal performance indicators.
3.18 Prior to 2009, there were no formal agreements between Health and Human Services—including its predecessors92, specifically covering the administration of the medical indemnity schemes.
3.19 Since 2009, a number of joint agreements underpinning the administration of the IIF’s schemes have been in place between Health and Human Services prior to the current Bilateral Head Agreement and programme agreements being established.93
3.20 The IIF-related programme agreements outlined the programme objectives for each IIF scheme as well as relevant legislative instruments. They also detailed:
- each department’s requirements and obligations, including deliverables;
- reporting requirements;
- key performance indicators;
- funding and financial management arrangements; and
- dispute/issues management procedures.
3.21 The programme-level agreements did not require Health and Human Services to formally meet at defined intervals. Nonetheless, in August 2015, both departments established more formal, regular meetings with the objective ‘to ensure the continual alignment of the policy and service delivery of the IIF schemes’. These quarterly governance meetings had covered agenda items such as:
- programme review;
- Premium Support Scheme contracts;
- legislation; and
- reporting.
3.22 Agreed actions were documented, including relevant responsibilities and relevant dates.
3.23 Representatives from both departments advised the ANAO that separate informal fortnightly teleconferences had generally taken place, with Health indicating that these informal arrangements had been in place since July 2015. The bilateral teleconferences were used to discuss and act on operational matters pertaining to the schemes.
3.24 In general, these arrangements provided a solid foundation for bilateral cooperation on the administration of the IIF schemes.
Measuring Performance
3.25 Key performance indicators (KPIs) should be relevant, reliable and complete, and provide a balanced assessment of overall performance, using both qualitative and quantitative measures.94 Human Services advised the ANAO that a cross-departmental key performance indicator review occurred when the 2012–15 Bilateral Head Agreement was renegotiated. Table 3.1 outlines the ANAO’s assessment of Health’s and Human Services’ relevant public and bilateral agreement KPIs against these characteristics.
Table 3.1: Assessment of the Health and Human Services Key Performance Indicators for the Indemnity Insurance Fund
|
Characteristic(a) |
Assessment |
|
KPIs |
Health (public)(b):
Human Services (programme agreements)(c)
|
|
Relevant |
Partially:
|
|
Reliable |
Yes:
|
|
Complete |
No:
|
Note a: These characteristics are based on the criteria developed to evaluate the appropriateness of an entity’s key performance indicators contained in ANAO Audit Report No. 21 2013–14, Pilot Project to Audit Key Performance Indicators, p. 41.
Note b: Department of Health, Portfolio Budget Statements 2016–17, Health, 2016, Canberra, p. 104–105.
Note c: Department of Health and the Department of Human Services, Programme Agreement-Medical Indemnity Scheme, 2015, p. 8; and Programme Agreement-Midwife Professional Indemnity Scheme, 2015, p. 7.
Source: ANAO analysis.
3.26 According to reporting in Health’s 2016–17 Portfolio Budget Statements, all KPI targets were met in 2015–16, including the KPI on uptake of the Premium Support Scheme (PSS). Respective targets for the 2013–14 and 2014–15 financial years were also publicly reported to be met.
3.27 Human Services’ internal reporting indicated that the KPI targets in the programme agreements—100 per cent of the agreed reports to Health within the agreed timeframes, have been met since the KPI was implemented in July 2014.
3.28 While the established public and programme agreement KPIs offered some useful insights into the performance of the IIF, they did not provide a complete basis for assessing outcomes against the IIF’s objectives. There are opportunities to develop KPIs that more directly assist in assessing the policy intent of the measure, for example, the change in the cost of average premiums over time, as well as other aspects of market stability. Human Services’ only KPI was also insufficient to make a useful assessment of its administrative performance for IIF, particularly around payment quality standards.
Are suitable administrative and other controls in place to support accurate payments, the security of personal information, and management of key records?
The Department of Health published the Indemnity Insurance Fund guidelines which outline key aspects of the Indemnity Insurance Fund’s administrative arrangements. The Department of Human Services established a range of internal guidance materials to assist its administration of the Indemnity Insurance Fund’s schemes. However, some of the guidance materials contain inaccuracies and need to be reviewed and updated.
The Department of Human Services’ claims assessment process, a series of manual and paper-based processes, is supported by a reasonable quality assurance process. Human Services has delayed the development of a medical indemnity online claiming system, which is intended to realise efficiencies for both insurers and the department; the department’s new electronic claiming system was expected to be delivered by October 2016. However, the department advised the ANAO that the project has been further delayed and a new implementation date has not yet been identified.
During 2014–15, due to problems with the functionality of its Health Professional Online System, the Department of Human Services implemented data transfer arrangements, albeit temporarily, and did not document its consideration of the risk of any compromise of the confidentiality of midwives’ personal information.
There is also scope for improving the Department of Human Services’ Indemnity Insurance Fund data integrity controls. In particular, the relevance, accuracy, and consistency of data provided by insurers, including to the Australian Government Actuary.
Indemnity Insurance Fund Flexible Fund Guidelines
3.29 The IIF’s establishment followed a 2010 strategic review of the administrative arrangements in the Health portfolio.95 Following the creation of the IIF in 2011, Health consolidated the administration of the schemes as described in the IIF Guidelines.96
3.30 The IIF Guidelines set out background to the IIF, including: the IIF’s objectives and priorities; the relevant roles and responsibilities of the Minister for Health, the departments of Health and Human Services; funding and the data that would be used to monitor the IIF. However, aspects of the IIF Guidelines were incomplete or inaccurate. For example the IIF Guidelines refer to:
- eligibility being prescribed in relevant legislation, but the applicable legislation was not referenced;
- Medicare Australia which is no longer an entity since it was merged within the Department of Human Services in 2011;
- grants when the IIF payments are not grants;
- medical indemnity insurers making electronic applications for funding through Human Services, whereas the claims application process is manual (see discussion of the claims process at paragraphs 3.34–3.37);
- Health continuing ‘to monitor the effectiveness of IIF activities and providing evidence-based policy advice to the government using data published in reports by the Australian Institute of Health and Welfare’ (AIHW). However, the AIHW medical indemnity series was discontinued following release of its 2012–13 report.97 To date, Health has not developed nor implemented an alternate data collection or monitoring strategy; and
- the glossary appears incomplete (it only defines one term).
3.31 Health’s IIF Guidelines, which were last updated in January 2014, need to be reviewed.
Human Services’ internal guidance material
3.32 Human Services maintains a range of internal guidance material in relation to policy, procedures and processes. Although the procedural material is comprehensive, there is scope for improvement in relation to document administration. For example, version control referencing was inconsistent between documents and revision history was not clear.98
3.33 In addition, the ANAO noted an inaccuracy in the policy guidance: AGA IBNR; ROCS and HCC, in relation to ROCS reporting. The policy guidance stated that the Minister for Health would table a report detailing the liabilities and funding of the Medical Indemnity Run-off Cover Scheme within six months of the end of the financial year. Whereas, the relevant legislation requires Health to make a request within six months of the end of the financial year for the production of the report, and that the report subsequently be tabled within 15 sitting days after it is supplied to the Minister for Health.99
Insurance claims processing and data integrity
Claims processing
3.34 Human Services is responsible for assessing and processing claims made under the IIF schemes in accordance with the governing legislation for each scheme.100
3.35 Under the IIF’s medical indemnity schemes (excluding the Midwife Professional Indemnity Scheme), insurers are required to submit paper-based claims, by mail or via insecure email to the department. Once received, claims are manually registered and assessed by a departmental officer.101
3.36 Human Services’ quality assurance process for IIF claims are embedded in its internal procedural guidance. The procedures require that each claim is expected to be reviewed by three different departmental officers and validated by a more senior officer before any payment is made. The ANAO’s observation of Human Services’ claims processing noted that the established quality assurance processes were being applied.
3.37 While it was originally scheduled that the electronic claiming system would be operational by mid–2016, the ANAO’s review of available project documentation found that the project had not progressed as planned. At the time of this audit fieldwork, in May 2016, consultation with industry stakeholders had only recently commenced. Human Services advised the ANAO that the project had been re-scheduled for delivery by October 2016. However, in August 2016, the department advised that the project had been further delayed and a new implementation date has not yet been identified.
Data security and integrity
3.38 Under the IIF bilateral and programme agreements with Health, Human Services was responsible for collecting, maintaining and reporting a range of key datasets in respect of the IIF schemes. The data collected by Human Services includes information on medical indemnity payments and claims, and premium information and data provided by insurers’ actuaries. With the exception of premium information data that was only provided to Health, the remaining data was provided directly to the AGA for analysis.
3.39 Under the Midwife Professional Indemnity Scheme Programme Agreement, with Health, Human Services is responsible for ‘maintaining an online solution for the purpose of all claims’. This system is known as Health Professional Online Solution or HPOS. The insurer is required to upload details of midwives’ contributions under the Midwife Professional Indemnity Run-off Cover Scheme into HPOS. While this data does not contain individuals’ names, it does include personal details such as: individuals’ insurance policy numbers, contributions, dates of birth, gender, state and postcodes.
3.40 Entities are required to take reasonable steps to protect the personal information they hold from misuse, interference and loss, and from unauthorised access, modification or disclosure.102 Human Services advised the ANAO that between December 2014 and June 2015, the relevant insurer experienced ‘intermittent’ issues with the HPOS system—such as slow response times and timeouts, when attempting to upload the data. The department further advised the ANAO that from June 2015 to May 2016, as a ‘work around’, the insurer was advised by Human Services to email the relevant data files to the department for manual upload—a less secure channel. The department’s programme specific risk management plan did not establish any controls or mitigations to reduce the risk of any potential compromise of personal information in an event such as this.
3.41 Human Services advised the ANAO that the HPOS issue had been rectified in May 2016 and the secure transfer of data had resumed. Health advised the ANAO that it was not notified of the above HPOS ‘work around’ until April 2016.
3.42 The ANAO’s analysis of IIF data also identified that a number of improvements to integrity controls would be prudent:
- ensuring that all insurers use the medical practitioner specialty codes specified in the IIF application forms when submitting data to provide consistency and reduce administrative risks associated with the AGA’s analysis and reporting; and
- consider review of insurers data, as provided to the AGA, to improve relevancy and accuracy. 103
3.43 In addition, ANAO analysis identified further opportunity to improve IIF data collection (see paragraphs 2.84 and 2.91).
Recommendation No.4
3.44 That the departments of Health and Human Services review their Indemnity Insurance Fund administrative arrangements to:
- establish a suitable set of public and internal key performance indicators that allow for relevant, reliable and complete reporting of the Indemnity Insurance Fund schemes’ performance;
- ensure that public guidance materials are accurate, consistent and current;
- establish suitable controls to improve data integrity, including monitoring and reporting of any relevant matters under the bilateral programme agreement; and
- consult with relevant insurers and the Australian Government Actuary to improve the relevancy, consistency and accuracy of data used to inform projections of the Commonwealth’s risks.
Health’s response: Agreed
Human Services’ response: Agreed
3.45 The department agrees with sub point (a) regarding establishing a suitable set of public and internal key performance indicators that allow for relevant, reliable and complete reporting of the Indemnity Insurance Fund schemes’ performance.
3.46 The department agrees with sub point (b) about the importance of ensuring that public guidance materials are accurate, consistent and current. The department will have its public guidance information updated by 31 October 2016.
3.47 The department agrees with sub point (c) regarding the requirement for suitable controls around data integrity to be established.
3.48 The department agrees with sub point (d) and will work with the Department of Health.
Do Health and Human Services analyse and report on the costs of administering the Indemnity Insurance Fund schemes?
The departments of Health and Human Services do not report on the costs of administering the Indemnity Insurance Fund and related schemes in a consistent and transparent manner.
While the department of Health publicly reports its Indemnity Insurance Fund departmental costs, Human Services does not report on its own Indemnity Insurance Fund-related costs.
The department of Health has not recently reviewed the basis on which the administration fees paid to insurers are calculated to ensure ongoing value for money to the government.
To improve transparency, there would be particular benefit in the departments of Health and Human Services analysing and reporting on the costs of Indemnity Insurance Fund administration over time.
Further, the reasonableness of the current administration costs needs to be considered by the department of Health in undertaking a ‘first principles review’ of the Indemnity Insurance Fund and related schemes.
3.49 The costs of administering the IIF and its related schemes can be categorised into:
- the costs of Health’s and Human Services’ overall administration of the IIF; and
- the costs for insurers to administer relevant schemes.
The cost of Health’s and Human Services’ administration of the Indemnity Insurance Fund
3.50 Health regularly reports on its departmental cost of IIF administration in its Portfolio Budget Statements. In 2016–17, Health received $1.528 million for its IIF administration costs; internally, $0.814 million of these monies was identified as staffing costs.
3.51 As shown in Figure 3.1, Health’s IIF administration costs have varied over time, declining sharply (86 per cent) from 2007–08 to 2008–09. Further reductions in Health’s departmental costs are seen over time, especially following the consolidation of the schemes within the IIF in 2011–12. Some modest increases are also apparent from 2015–16.
Figure 3.1: Health’s Departmental Expenses for the Indemnity Insurance Fund

Note: Expenses for 2015–16 and 2016–17 are an estimate only and figures for financial year 2007–08 to 2009–10 are for ordinary annual services.
Source: ANAO analysis of Health’s Portfolio Budget Statements.
3.52 Funding for Human Services’ costs is sourced from within its overall departmental appropriation. Human Services’ costs of administering the IIF schemes are not publicly reported. The department advised the ANAO that while it was not able to provide the actual cost of administering the Indemnity Insurance Fund, the department estimated its 2015–16 IIF expenditure (based on 9 full-time equivalent staff) was approximately $1.265 million. Health has no visibility of Human Services’ IIF administration costs.
Cost for the administration of relevant schemes
3.53 Under tripartite contracts with the Commonwealth (as represented by Health and Human Services), relevant medical indemnity insurers receive fees to cover their costs of administering defined elements of the Premium Support Scheme (PSS) and Midwife Professional Indemnity Schemes. These administration fees cover obligations imposed on the insurers, such as:
- gathering of the information required to assess a medical practitioner’s (participant) eligibility;
- calculating participants’ subsidy amounts; and
- lodging claims on behalf of participants.
Administration fees—Premium Support Scheme
3.54 The PSS administration fee agreed between the Commonwealth, as represented by Health and Human Services, and the relevant insurers was to be determined by an authorised officer under the Premium Support Scheme Act 2004 and was originally outlined in the initial 2003–06 contracts with each insurer.
3.55 Under the Premium Support Scheme Amendment 2007 the administration fee payable to insurers was based on a proportion of a PSS Administration Fee Pool.104 From 2007, the PSS Administration Fee Pool for a financial year was based on the previous financial year’s amount plus indexation.105 Administration fee arrangements for the 2013–16 PSS contracts are still operating under this arrangement.
3.56 Figure 3.2 compares the total fees paid to insurers to administer the PSS against the number of eligible PSS participants.
Figure 3.2: Premium Support Scheme administration fees compared to eligible participants 2004–05 to 2014–15

Source: ANAO analysis of Human Services’ annual reports.
3.57 Figure 3.2 shows that in 2007–08, there was a peak of 7210 eligible PSS participants, which then declined 81 per cent to 1400 eligible participants in 2014–15. Similarly, the PSS administration fees paid to relevant insurers declined 48 per cent from a peak of $2.5 million in 2010–11 and 2011–12 to $1.3 million in 2014–15. Although the decline in PSS administration fees occurred several years after the drop in eligible participants, overall there was a broad correlation between the reduction in eligible participants and the reduction in insurers’ administration costs to the government.
3.58 In 2012–13, as the affordability of indemnity insurance improved, Health advised its Minister of the correlation between the decline in the PSS administration fees and declining participation in the PSS. Health further advised its Minister that a reduction in the PSS administration fees had been negotiated by identifying opportunities to improve the efficiency of the administration of the scheme—specifically reducing the administrative burden for insurers via reduced risk reporting requirements.106
Administration fees—Midwife Professional Indemnity Scheme
3.59 The contract with the MIGA—the sole insurance provider for the Midwives Professional Indemnity Scheme (MPIS)—defines the administration fees in respect of the obligations imposed for administering MPIS.
3.60 Health advised the ANAO that the MPIS administration fee was determined in 2010, following the original tender process when the MPIS was developed, and that ongoing administration fees were renegotiated alongside contract renewal negotiations. The contract had been extended twice with the insurer seeking additional funds on the basis that indexation had not been automatically applied to the 2010 fee—unlike the PSS fee arrangements.
3.61 Figure 3.3 outlines the MPIS administration fees since the scheme’s inception.
Figure 3.3: Midwife Professional Indemnity Scheme administration fees 2010–11 to 2014–15

Source: ANAO analysis of Human Services’ annual reports.
3.62 These administration costs are intended to offset the administration of professional indemnity insurance cover for 106 privately practicing midwives (as at 30 June 2015). For 2014–15, this fee equates to just over $1500 to administer the scheme for each eligible midwife.
3.63 Apart from 2010–11, the ANAO’s analysis indicates that the department’s approach to reporting MPIS administration fees in its annual reports was not consistent. For example, the administration fee for 2013–14 ($125 000), as reported in Human Services’ 2013–14 Annual Report, was significantly below the amount set out in the contract with the insurer ($165 000).107 There were also smaller differences for 2011–12, 2012–13 and 2014–15.108 While Human Services reports publicly on the cost of insurers administering the Indemnity Insurance Fund schemes, neither Health nor Human Services report publicly or internally on the costs of departmental administration in a transparent manner.
3.64 There has not been a recent review in relation to the basis on which the administration fees paid to insurers are calculated to ensure on-going value for money to the government.
3.65 To improve transparency, there would be particular benefit in Health and Human Services reporting on and analysing the administrative costs of the Indemnity Insurance Fund over time. Further, the reasonableness of administration costs needs to be considered by Health in undertaking a ‘first principles review’ of the Indemnity Insurance Fund and related schemes.109
Appendices
Appendix 1 Entity responses


Appendix 2 Financial arrangements
- Funding (administered expenses) for the IIF schemes was made through special appropriations for medical indemnity and midwives professional indemnity with a separate appropriation for Health’s departmental expenses. Reported actual expenditure under the IIF schemes (including liabilities) for special appropriations for the period 2004–05 to 2014–15 was approximately $957 million110 with departmental expenses of $7.1 million over this same period.111 Human Services’ departmental expenses are separately appropriated for the IIF schemes. Human Services advised the ANAO that it is unable to provide this information.
- Each year, the Australian Government Actuary (AGA) provides Health with estimates of annual expenses and liabilities for each scheme. Due to the ‘long tail’ of potential indemnity insurance claims, unexpended funds from each year are carried over into that scheme’s estimates of ongoing liabilities. Table A.1 outlines the number of claims, payments—including benefits paid and fees to contracted insurers, liabilities and revenue collected112—under each of the Fund’s schemes since 2004–05.
Table A.1: Indemnity Insurance Fund claims payments, liabilities and receipts for the period 2004 to 2014
|
Scheme |
No. of claims 2004–15 |
Benefits paid 2004–15 ($’m) |
Fees paid to insurers ($’m)(b) |
Liabilities as at 30 June 2015 ($’m) |
Revenue collected ($’m)(c) |
|
IBNR |
1868 |
$91.9 |
– |
$34 |
– |
|
PSS |
3357(a) |
$199.2 |
$24.1 |
– |
– |
|
HCCS |
1349 |
$208.9 |
– |
$300 |
– |
|
ECS |
– |
– |
– |
– |
– |
|
ROCS |
393 |
$16.0 |
$1.2 |
$79 |
($112.9) |
|
MPIS |
– |
– |
$1.5 |
– |
– |
|
MPIROC |
– |
– |
$0.8 |
– |
($.049) |
|
Totals |
3610 |
$516 |
$27.6 |
$413 |
($113) |
|
Total reported benefits and fees paid plus liabilities |
$956.6 |
||||
Note a: Shows the average number of eligible practitioners per year from 2004–05 to 2014–15 and is not included in the Claims Totals.
Note b: Fees paid to insurers includes: payments (to insurers) in respect of compliance costs and internal claims handling costs under the ROC Claims and Administration Protocol (Medical Indemnity Act 2004–05, s.34ZN) for the period 2004–2013; midwives’ ROC support payments indemnity payments under the Midwife Professional Indemnity (Commonwealth Contribution) Scheme Act 2010 for the period 2010–2013; administration fees under the PSS for the period 2004–2015 and contract payments for the provision of Midwife Professional Indemnity Insurance by MIGA (01 July 2010 to 30 June 2015).
Note c: ROCS support payments are collected by Human Services, on behalf of the government, in the form of an annual tax (or levy) on each insurer from 1 July 2004. The midwives’ ROC support payments are collected by Human Services, on behalf of the government, as an annual tax (or levy) on MIGA from 1 July 2010. Public reporting of the revenue collected from ROCS support payments is outlined in the AGA reports and Health’s Annual Reports.
Source: ANAO analysis, based on: data from Human Services’ annual reports 2004–05 to 2014–15; AGA Run-off Cover Schemes annual reporting (ROCS 2004–05 to 2013–14, ROCS midwife professional indemnity scheme 2010–11 to 2014–14); AGA expense and liability estimates prepared for Health, as at 30 June 2015 and contract payments for the provision of Midwife Professional Indemnity Insurance to MIGA (01 July 2010 to 30 June 2015). Note numbers may not add due to rounding.
Appendix 3 Legislation impacting on medical indemnity insurance and regulation
|
No. |
Legislation |
Description |
Administered by |
|
1 |
Insurance Act 1973 |
The main object of this Act is to protect the interests of policyholders and prospective policyholders under insurance policies (issued by general insurers and Lloyd’s underwriters) in ways that are consistent with the continued development of a viable, competitive and innovative insurance industry. |
APRA ASIC |
|
2 |
Insurance Contracts Act 1984 |
An Act to reform and modernise the law relating to certain contracts of insurance so that a fair balance is struck between the interests of insurers, insureds and other members of the public and so that the provisions included in such contracts, and the practices of insurers in relation to such contracts, operate fairly, and for related purposes. |
ASIC |
|
3 |
Medical Indemnity Act 2002 |
An object of this Act is to contribute towards the availability of medical services in Australia by providing Commonwealth assistance to support access by medical practitioners to arrangements that indemnify them for claims arising in relation to their practice of their medical professions. |
Health Human Services (payments) |
|
4 |
Medical Indemnity Agreement (Financial Assistance—Binding Commonwealth Obligations) Act 2002 |
An Act about binding Commonwealth obligations to provide financial assistance under indemnity agreements relating to Australasian Medical Insurance Limited and United Medical Protection Limited, and for related purposes. |
Health Human Services (payments)
|
|
5 |
Medical Indemnity (Consequential Amendments) Act 2002 |
An Act to make amendments consequential on the enactment of the medical indemnity legislation, and for related purposes. |
Health Human Services (payments) |
|
6 |
Medical Indemnity (UMP Support Payment) Act 2002 |
An Act to impose a tax on certain members and former members of certain medical defence organisations, and for related purposes. |
Health |
|
7 |
Medical Indemnity (Prudential Supervision and Product Standards) Act 2003, except to the extent administered by the Minister for Health |
The objects of this Act are to:
|
ASIC APRA, Part 3: Division 2 Health, Part 3: Division 2.A |
|
8 |
Medical Indemnity (Run-off Cover Support Payment) Act 2004 |
For each contribution year, a Run-off cover support payment is imposed as a tax on each medical indemnity insurer. Medical Indemnity (Run-off Cover Claims and Administration) Amendment Protocol 2013. |
Health Human Services (payments) |
|
9 |
Medical Indemnity (Competitive Advantage Payment) Act 2005 |
An Act to impose a tax on certain medical indemnity insurers, and for related purposes. |
Health Human Services (payments) |
|
10 |
Midwife Professional Indemnity (Commonwealth Contribution) Scheme Act 2010 |
An object of this Act is to contribute towards the availability of professional midwife services in Australia by providing Commonwealth assistance to support access by eligible midwives to arrangements that indemnify them for claims arising in relation to their practice of the profession of midwifery. |
Health Human Services (payments) |
|
11 |
Midwife Professional Indemnity (Run-off Cover Support Payment) Act 2010 |
An Act to make provision in relation to professional indemnity cover for certain midwives, and for related purposes. |
Health Human Services (payments) |
|
12 |
Health Legislation Amendment (Midwives and Nurse Practitioners) Act 2010 (Cth) |
An Act to amend the law relating to health and to make amendments consequential on the enactment of the Midwife Professional Indemnity (Commonwealth Contribution) Scheme Act 2010, and for related purposes |
Health Human Services (payments) |
Source: Department of Human Services, listings of Medical Indemnity Legislation, Medical Indemnity Scheme and Midwives Professional Indemnity Scheme programme agreements, September 2015.
Footnotes
1 Hon J.B. Hockey, Treasurer, Senator the Hon. Mathias Cormann, Minister for Finance, Joint Media Release, Our response to the National Commission of Audit Report, 13 May 2014. Available from: <http://www.financeminister.gov.au/media-release/2014/05/13/our-response-national-commission-audit-report>.
2 Department of Health and Ageing, Portfolio Budget Statements, 2010–11, p. 348.
3 Before 1 July 2003, medical indemnity protection was traditionally offered by medical defence organisations (MDOs)—not-for-profit mutual organisations created by and owned by medical practitioners to provide a range of services to members, including indemnity. Cover provided by MDOs was discretionary—that is, the medical practitioner had no contractual right to be indemnified by the MDO.
4 Australian Competition and Consumer Commission, Medical indemnity insurance report: sixth monitoring report, ACCC, Canberra, April 2009.
5 Average medical indemnity premiums increased by 221 per cent between 1995 and 2005 (at an average rate of 13 per cent per annum). The largest annual increase was in 2002, when the average premium rose nearly 50 per cent. Medical Indemnity Industry Association of Australia. Medical indemnity report: an analysis of premium and claim trends in Australia from 1995 to 2005, 21 August 2006. Prepared by Insurance Statistics Australia Limited.
6 The Prime Minister, the Hon. John Howard MP, Transcript: Medical Indemnity Insurance, 19 December 2001. Available from: <http://pmtranscripts.dpmc.gov.au/release/transcript-12181>.
7 A tort is a legal wrong which one person or entity (the tortfeasor) commits against another person or entity and for which the usual remedy is an award of damages. Australian Law Reform Commission, Traditional Rights and Freedoms—Encroachments by Commonwealth Laws (IP46), ALRC Issues Paper 46, 2014, p. 107.
8 Department of Health, Indemnity Insurance Fund website. Available from: <http://www.health.gov.au/internet/main/publishing.nsf/Content/budget2011-flexfund-indemnity19.htm>
9 These were the: Premium Support; High Cost Claims; Exceptional Claim; Run-off Cover; Incurred-But-Not-Reported; Midwife Professional Indemnity Commonwealth Contribution; and Midwife Professional Indemnity Run-off Cover Schemes.
10 Department of Health, Indemnity Insurance Fund website. Available from: <http://www.health.gov.au/internet/main/publishing.nsf/Content/flexible-fund-guide2011.htm>
11 Department of Health and Ageing, Portfolio Budget Statements, 2010–11, p. 350.
12 APRA are responsible for regulating medical indemnity insurers, including as part of its broader responsibilities for the general regulation of insurance companies. ASIC are responsible for the regulation of products, standards and disclosure requirements which apply to medical indemnity insurance policies.
13 Department of Health, Portfolio Budget Statements, 2004–05 to 2014–15.
14 Payments for actuarial services provided by the AGA under the memorandum of understanding were made from the Department of Health’s departmental appropriations.
15 The Department of Human Services advised the ANAO that while it was not able to provide the actual cost of administering the Indemnity Insurance Fund, it was able to provide an estimate for 2015–16.
16 The ANAO survey covered the themes of: interactions with the departments of Health and Human Services; roles and responsibilities; consultation; information and data transfer; and views on the National Commission of Audit recommendations. Insurance providers, peak medical bodies, and other government stakeholders were invited to comment. Fifteen of the 24 (63 per cent) entities and bodies approached provided responses.
17 The Prime Minister, the Hon. John Howard MP, Transcript: Medical Indemnity Insurance, 19 December 2001. Available from: < http://pmtranscripts.dpmc.gov.au/release/transcript-12181>.
18 Some of these forums included: the Secretaries’ Taskforce on Medical Indemnity Insurance (including the secretaries of the departments of the Prime Minister and Cabinet, the Treasury—which includes the Australian Government Actuary—Finance and Administration, Attorney-General’s and Health and Ageing); and, through the Council of Australian Governments (COAG), the Australian Health Ministers’ Advisory Council (AHMAC); the Standing Committee of Attorneys-General; and the Heads of Treasury Accounting and Reporting Advisory Committee.
19 The IBNR Scheme was funded through an IBNR levy on medical/general practitioners who were members of UMP as at 30 June 2002. Medical indemnity cover is ‘long-tailed’, which means that claims can be brought against doctors a long time after the alleged negligence occurred. This means that providers of medical indemnity cover need to consider IBNR claims, which are claims that will potentially be made (reported) in the future from negligence occurring today.
20 Medical Indemnity Policy Review Panel, Affordable, Secure and Fair, Report to the Prime Minister 10 December 2003, pp. 0–21.
21 The Australian Health Ministers Advisory Council, an advisory and support body (now the COAG Health Council), commissioned the AIHW to develop the Medical Indemnity National Collection (MINC), with the Commonwealth and states and territories cost-sharing the project. There were 14 reports released as part of the MINC. Eight reports presented annual data on public sector medical indemnity claims and six reports presented annual data on both public and private sector medical indemnity claims.
22 Australian Institute of Health and Welfare. Australia’s medical indemnity claims 2012–13, Canberra, 2014, AIHW, p. vii.
23 All APRA-regulated insurers that provide public and products liability and professional indemnity insurance policies are required to contribute claims and policies data to the National Claims and Policies Database. Other organisations, such as state and territory insurers also submit data to the National Claims and Policies Database. The first data was collected in early 2005 for the period from 1 January 2003 to 31 December 2004.
24 The Prime Minister asked the ACCC, initially for 3 years, to monitor and report on the affordability of medical indemnity premiums to assess whether they were actuarially and commercially justified across jurisdictions. As part of the 2006–07 Budget, the ACCC’s monitoring role was extended to 2008–09. The ACCC were then asked to expand the scope of their analysis to also assess whether premiums were actuarially and commercially justified across and within jurisdictions.
25 State and territory jurisdictions introduced reforms progressively from 2002 to 2006, with each jurisdiction taking into account its own circumstances. The reforms were broadly consistent with the recommendations of the Review of the Law of Negligence (the Ipp review), Minter Ellison Special report: Tort law reform throughout Australia: a brief review of recent amendments (Sixth edition, December 2005).
26 Medical Indemnity Act 2002 s. 34ZW and the Midwife Professional Indemnity (Commonwealth Contribution) Scheme Act 2010 s. 48.
27 Medical Indemnity Policy Review Panel, Affordable, Secure and Fair, Report to the Prime Minister 10 December 2003 pp. 20–21 and Medical Indemnity Policy Review Panel, Achieving Stability and Premium Affordability in the Australian Medical Indemnity market Place, February 2007, p 2.
28 Parliament of Australia, Medical Indemnity Legislation Amendment (Competitive Neutrality) Bill 2005, Bills Digest No. 16, 2005–06. Available from: <http://www.aph.gov.au/Parliamentary_Business /Bills_Legislation/bd/bd0506/06bd016>.
29 ACCC, Medical indemnity insurance: fourth monitoring report, April 2007, p 23.
30 Medical Indemnity Policy Review Panel, Achieving stability and premium affordability in the Australian medical indemnity marketplace, February 2007, p 21.
31 The findings of the review were presented in Improving maternity services in Australia: the Report of the Maternity Services Review in 2009. Available from: <http://www.health.gov.au/internet/ main/publishing.nsf/Content/8AF951CE492C799FCA257BF0001C1A4E/$File/maternityplan.pdf>.
32 Australian Health Ministers’ Conference, National Maternity Services Plan, 2010, p. 58.
33 Department of Health, Flexible Fund Guidelines, Indemnity Insurance Fund, Attachment A, January 2014.
34 Medical Indemnity Policy Review Panel, Achieving stability and premium affordability in the Australian medical indemnity marketplace, February 2007, pp 13 and 9.
35 ACCC, Medical indemnity insurance report: sixth monitoring report, April 2009, p. 11.
36 Medical Indemnity Policy Review Panel, Achieving stability and premium affordability in the Australian medical indemnity marketplace, February 2007, p. 23.
37 ACCC, Medical indemnity insurance report: sixth monitoring report, April 2009, p. 36.
38 Medical Indemnity Policy Review Panel, Achieving stability and premium affordability in the Australian medical indemnity marketplace, p. 2.
39 Rogers, G. 2005. Review of competitive neutrality in the medical indemnity insurance industry. Report to the Australian Government, p. 6.
40 APRA’s transitional arrangements enabled medical indemnity providers to build capital up to APRA’s targeted capital level by 30 June 2008. Effective 1 July 2008, APRA advised in practice note GPG 100 that medical indemnity insures are expected to maintain a capital ‘buffer’ of at least 150 per cent. ACCC, Medical indemnity insurance report: sixth monitoring report, April 2009, p. 46.
41 Rogers, G. 2005. Review of competitive neutrality in the medical indemnity insurance industry. Report to the Australian Government, p. 7.
42 ACCC. Medical Indemnity Insurance report: sixth monitoring report, 2009, p. 35.
43 The five medical indemnity insurers as at 30 June 2008 were: MDA National Insurance, Medical Insurance Group Australia, Medical Indemnity Protection Society, Avant Insurance, and QBE Insurance, ibid., p. xii.
44 ibid., p. 44.
45 ACCC, Medical Indemnity Insurance: first Monitoring Report, 2003, p. 20.
46 National Commission of Audit website. Available from: <http://www.ncoa.gov.au/report/appendix-vol-2/10-16-medical-indemnity.html>.
47 The Department of Health, Flexible Fund Guidelines, Indemnity Insurance Fund, January 2014, p. 3.
48 ibid., p. 2.
49 ibid., p. 5.
50 Medical Indemnity Policy Review Panel, Achieving stability and premium affordability in the Australian medical indemnity marketplace, February 2007, pp.9 and 21.
51 Medical Indemnity Insurance Association of Australia Newsletter, Issue 18 – August 2010 stated that the MIIAA, on behalf of the Stakeholder Forum, provides half-yearly reports to the Department of Health and Ageing on issues raised during the Stakeholder Forum.
52 The ANAO has previously commented on the effectiveness of Health’s record keeping. See ANAO Audit Report No. 10, 2015–16 Records Management in Health, p. 8.
53 Data provided to AGA from insurers for these purposes comprise the insurers’ own actuarial projections of claims, rather than individual claim data.
54 The AGA reports provide information on the Commonwealth’s Run-off Cover Scheme for medical indemnity insurers medical indemnity. Available from: <http://www.aga.gov.au/publications/>.
55 Department of Health, Flexible Fund Guidelines: Indemnity Insurance Fund, January 2014, Clause 1.1, p. 3.
56 ibid,. Appendix, Section - Promote stability of the medical indemnity insurance industry, paragraph 1.
57 ACCC, Medical indemnity insurance report: sixth monitoring report, April 2009, p. xvi.
58 General insurers are required to hold a minimum level of capital, referred to as the Minimum Capital Requirement (MCR). The MCR is calculated according to a complex formula that takes into account a range of risk factors that may threaten an insurer’s capital base. Insurers are required to hold at least 1.2 times their MCR, referred to as their capital adequacy multiple (CAM).
59 ACCC, Medical indemnity insurance report: sixth monitoring report, April 2009, p. 44.
60 Health reported 6 separate contract notices on AusTender for the MIGA contracts for the period December 2009 to June 2017 with a total value of approximately $3.4 million. The department has in fact had the same contract in place since 2009 which has been amended or varied over the years. The total expenditure under the contract for the provision of midwives indemnity insurances for 2009–17 (as identified at the time of audit) will be approximately $3.8 million.
61 The insurance policy for midwives only covers antenatal and postnatal care in any setting including unplanned homebirths. The policy does not cover intra-partum care as part of a planned homebirth.
62 Department of Health, Flexible Fund Guidelines: Indemnity Insurance Fund, January 2014, p. 3.
63 As outlined in the relevant programme agreements—the keys pieces of legislation that underpin the IIF measures is the Medical Indemnity Act 2002 and the Midwife Professional Indemnity (Commonwealth Contribution) Scheme Act 2010.
64 Sunsetting provisions in legislation provide that the law ceases to have effect after a specific date unless further legislative action is taken to extend that law. Agencies must plan for sunsetting well in advance of an instrument’s sunset date, as the process to review and action review recommendations for each instrument can be lengthy. A thematic review is a review of two or more instruments which share a common theme, such as a particular treaty or the regulation of a particular industry. Thematic reviews are not limited to instruments made under a single Act or administered by a single agency. Australian Government, Attorney-General’s Department, Guide to Managing Sunsetting of legislative Instruments, April 2014, pp. 4 and 11.
65 Reforms included medical indemnity insurers becoming subject to minimal capital requirements/supervision by the Australian Prudential Regulatory Authority (APRA); tort law reform in state jurisdictions and the development of a national ‘Open Disclosure’ standard which allows for ‘…open communication in public and private hospitals, following an adverse event in health care’.
66 ACCC, Medical indemnity insurance: third monitoring report, February 2006, p. 39.
67 Australian Government. Available and affordable Improvements in liability insurance following tort law reform in Australia. Attorney-General’s Department, 2006, p 15.
68 These AGA reports provide information on the Commonwealth’s future liabilities of the medical indemnity and the midwives schemes and the general financial position of the schemes in relation to support payments and claims.
69 Australian Government Actuary, Tenth report on the costs of the Australian Government’s Run-off Cover Scheme for medical indemnity insurers. AGA Canberra, 2015, p. 22.
70 ibid., p. 19.
71 The Department of Health, Flexible Funds, October 2015. Available from: <http://www.health.gov.au/internet/main/publishing.nsf/Content/budget2011-flexfunds.htm>.
72 The Treasury is consulting with states and territories regarding the medical injury stream of the no fault National Injury Insurance Scheme (NIIS), proposed by the Productivity Commission in August 2011. Implementation of the proposed medical injury stream of the NIIS would result in no fault care and support arrangements for catastrophic injuries arising from medical treatment. The medical injury stream of the NIIS has the potential to reduce claims subsidised through the HCCS and ROCS.
73 Our response to the National Commission of Audit report, Hockey & Corman, Joint Media Release, 13 May 2014. Available from: <http://www.financeminister.gov.au/media-release/2014/05/13/our-response-national-commission-audit-report>.
74 The Department of Health, Flexible Fund Guidelines - Indemnity Insurance Fund, January 2014.
75 Human Services defines participants as the number of practitioners participating in the PSS in a financial year.
76 The subsidy is more generous for procedural general practitioners in rural areas.
77 For instance, see <http://work.chron.com/much-doctors-pay-insurance-7304.html>.
78 From 1st January 2003, the Medical Indemnity Subsidy Scheme (MISS) applied. MISS subsidised premiums for doctors working only in high risk fields, where premiums were higher. These specialties were: obstetricians; procedural GPs (rural and non-rural); GP registrars undertaking procedural training; and neurosurgeons. The MISS subsidies were grandfathered when the PSS was introduced. Doctors who received a subsidy for the MISS still qualify for a MISS subsidy (under the MISS’s original terms) and continue to receive their MISS subsidy. The subsidy was a percentage of the difference between the premium in the high risk speciality and the premium in a corresponding, lower risk specialty. The rate of subsidy varies across high risk specialties.
79 Seventy-seven per cent of GP Proceduralists are categorised as rural/regional.
80 The Modified Monash Model uses the Australian Bureau of Statistics’ Australian Statistical Geography Standard - Remoteness Areas as a base, and further differentiates areas in Inner and Outer Regional Australia based on local town size.
81 Under s. 66–10 of the Private Health Insurance Act 2007, private health insurers must apply to the Minister for Health for approval of premium changes. The Minister must approve the proposed changes unless satisfied that a change would be contrary to the public interest. Each application was closely scrutinised to ensure the increases are fully justified.
82 ACCC, Medical indemnity insurance report: sixth monitoring report, April 2009, p. xiv.
83 At the time of the audit fieldwork, 2013–14 payment data was the most current available from Human Services as, under its PSS contracts with relevant insurers, insurers have up to 13 months from the end of the relevant premium period to provide information on medical practitioners’ actual income to Human Services.
84 Australian Bureau of Statistics, Average Weekly Earnings, Australia, 2016. Available from: <http://www.abs.gov.au/ausstats/abs@.nsf/mf/6302.0>.
85 In particular, a time series of the reported incurred cost for all medical indemnity insurance claims (that is, those that are below the HCCS $300 000 threshold) is needed to understand how the reported incurred cost on open claims might develop in the future.
86 The Department of Health, Flexible Fund Guidelines - Indemnity Insurance Fund, January 2014.
87 The 2015–2018 Bilateral Head Agreement between Health and Human Services was signed on 30 October 2015. The bilateral head agreement outlines the agreement of the departments to work cooperatively to fulfil their respective roles and responsibilities on policy and the administration of health programs.
88 The bilateral head agreement and the relevant medical indemnity scheme programme agreements established between Health and Human Services, set out their shared commitment to work in partnership for the effective coordination and delivery of a range of Australian Government health policy priorities, objectives and services, including the IIF schemes.
89 In August 2011, the Productivity Commission recommended the establishment of two schemes: the National Disability Insurance Scheme and the National Injury Insurance Scheme (NIIS). The Australian Government is continuing to work with states and territories on a NIIS for individuals who are catastrophically injured in workplace accidents, medical treatment accidents or general accidents (occurring in the home or community). The Department of the Treasury, National Injury Insurance Scheme. Available from: <http://www.treasury.gov.au/Policy-Topics/PeopleAndSociety/National-Injury-Insurance-Scheme>.
90 Department of Finance, Commonwealth Risk Management Policy, 2014, p. 16. Available from: <http://www.finance.gov.au/sites/default/files/commonwealth-risk-management-policy.pdf>.
91 From 2009, the relevant entities (Health and Medicare Australia) operated under a memorandum of understanding; from 2010, business practice agreements between Health and Medicare Australia outlined respective programme-level requirements; and for the period 2012–2015, a high level bilateral head agreement was established between Health and Human Services, supported by an Indemnity Insurance Fund Business Agreement and schedules.
92 Before 2005, the Health Insurance Commission was responsible for administering relevant IIF schemes in place at that time. Between 2006 and 2011, Medicare Australia was the responsible administering entity. From 2011, Medicare Australia (along with Centrelink and the Child Support Agency) was merged within the Department of Human Services.
93 From 2009, the relevant entities (Health and Medicare Australia) operated under a memorandum of understanding; from 2010, business practice agreements between Health and Medicare Australia outlined respective programme-level requirements; and for the period 2012–2015, a high level bilateral head agreement was established between Health and Human Services, supported by an Indemnity Insurance Fund Business Agreement and schedules.
94 ANAO Audit Report No. 21 2013–14, Pilot Project to Audit Key Performance Indicators, p. 41.
95 The strategic review identified an opportunity to improve the management of (acute care) programs by consolidating them into larger ‘flexible funds’ in order to cut red tape, increase flexibility, and more efficiently provide evidence based funding for the delivery of health outcomes to the community.
96 The Department of Health, Flexible Fund Guidelines - Indemnity Insurance Fund, January 2014.
97 Australian Institute of Health and Welfare, Medical indemnity publications, AIHW, 2013. Available from: <http://www.aihw.gov.au/publications/medical-indemnity/>.
98 The department’s process maps had capacity to document version details, yet this capacity was not used.
99 Medical Indemnity Act 2002, s. 34ZW(1).
100 The accuracy of Human Services’ claims assessments and payments were not within the scope of this audit.
101 Although the claims process is paper based, the department maintains scanned electronic copies of the hard copy claims for back-up purposes.
102 Office of the Australian Information Commissioner, Australian Privacy Principles (APP 11). Available from: <https://www.oaic.gov.au/agencies-and-organisations/app-guidelines/chapter-11-app-11-security-of-personal-information>.
103 The bilateral agreements between the departments do not establish a requirement for Human Services to reconcile its own payment data with the claims data provided by insurers.
104 The proportion was calculated based on each insurers’ market-share of ROCS members.
105 Health advised the ANAO that the base amount is indexed in line with Wage Cost Index 3. See Australian Bureau of Statistics, Wage Price Index, Australia, ABS, 2016. Available from: <http://www.abs.gov.au/Ausstats/abs@.nsf/0/21A522D06599E6F8CA2573F500152ECC?OpenDocument>.
106 Prior to the renewal of PSS contracts in 2013–14, insurers were required to provide Health with a risk management report in relation to medical practitioners eligible for PSS undertaking risk management training and activities. The Health Practitioner Regulation National Law (which came into force while the 2010–2013 PSS contracts were in operation) required health practitioners to undertake continuing professional development. Therefore, the clauses in the contracts relating to risk management training and activities were removed when the 2013–2016 contracts were renewed.
107 Human Services advised the ANAO that in 2010–11 the reported figure was inclusive of GST, and since 2011−12 all financial information has been consistently reported as exclusive of GST. Human Services further advised that the substantial discrepancy in 2013–14 was due to certain administration fee payments that accrued in 2013–14 were reported as 2014–15 payments.
108 The MPIS administration fee publicly reported by Human Services in 2011–12 was $162 468 whereas the contract stated $178 715; in 2012–13 the reported fee was $173 916 whereas the contract stated $191 308; in 2013–14 the reported fee was $125 000 whereas the contract stated $165 000; and in 2014–15 the reported fee was $175 000 whereas the contract stated $165 000.
109 See Recommendation No.4, p. 57.
110 Department of Health, Portfolio Budget Statements, 2004–05 to 2014–15.
111 Payments for actuarial services paid to the AGA under the MOU were made from the Department of Health’s departmental appropriations.
112 Run-off Cover Scheme notional accounts are maintained. The Notional Accounts are not official Government accounts. Rather, they are a device established for the sole purpose of facilitating equity between practitioners and other taxpayers. AGA: Tenth report on the costs of the Australian Government’s ROCS for medical indemnity insurers p. 19; and Fourth report on the costs of the Australian Government’s Run-off Cover Scheme for midwife professional indemnity insurers p. 12.