Browse our range of reports and publications including performance and financial statement audit reports, assurance review reports, information reports and annual reports.
Managing Mental Health in the Australian Federal Police

Please direct enquiries relating to reports through our contact page.
The objective of this audit was to examine the effectiveness of the Australian Federal Police in managing employee mental health.
Summary and recommendations
Background
1. Managing employee mental health effectively is a challenge faced by policing and first responder organisations around the world. This includes the Australian Federal Police (AFP) as the Australian Government’s primary policing agency responsible for the enforcement of Commonwealth laws and the protection of Australian interests from criminal activity, both domestically and overseas. To fulfil this role the AFP is responsible for a diverse range of functions, the delivery of which place a range of unique demands and stressors on AFP employees.
2. Safe Work Australia’s Work-Related Mental Disorders Profile 2015 concluded that first responders—police, emergency and health services—were the combined occupational group most likely to make a workplace compensation claim based on mental health injury, with incidence rates and costs substantially exceeding other occupational groups.
Audit objective and criteria
3. The objective of this audit was to examine the effectiveness of the Australian Federal Police in managing employee mental health.
4. To form a conclusion against the audit objective, the ANAO adopted the following high level criteria:
- Has the AFP implemented sound governance and risk management practices to manage employee mental health?
- Is the AFP effectively managing employee mental health throughout their career lifecycle?
- Are sound monitoring, reporting and evaluation arrangements in place to assess the effectiveness of the AFP’s management of mental health?
Conclusion
5. The AFP lacks a comprehensive and consolidated organisational health and wellbeing framework to enable effective management and support of employee mental health. While the AFP offers a variety of mental health support services, there is no evidence that these services are effective and they are not supported by sound governance, risk management, evaluation or an articulated business rationale. Any reform of the portfolio of services available should be made in the context of available data on employee access, areas of high stress and risk, gap analysis, organisational culture and employee preferences.
6. The AFP has identified gaps in its management of employee mental health across the organisation and has commenced processes, within existing organisational constraints, to improve the management of employee mental health, which is a complex and sensitive challenge for the AFP and other first responder organisations. Since the end of 2016, eight initiatives have commenced to improve mental health management across the AFP, including a review of AFP’s mental health support services, the establishment of a Mental Health Strategy Board, the launch of an expanded Welfare Officer Network and a wellbeing application (app)—Equipt.
7. While currently developing a mental health framework, the AFP has not established a clear governance structure for decision-making, information sharing and oversight in relation to employee mental health arrangements. Reporting into the governance structure is not comprehensive or risk-based, making it difficult to identify emerging mental health related risks and to utilise this reporting to inform decision making in resource prioritisation to address increasing mental health risks.
8. The AFP formally included mental health as a strategic risk to the organisation in October 2016, however this risk identification has not led to substantive engagement and coordinated identification of mental health risks faced by all of the AFP’s functional areas.
9. The AFP does not currently have in place mechanisms or sufficient data to appropriately align resources with key mental health risks.
10. Screening processes are in place to assess the suitability of employees’ psychological readiness for sworn roles. These are undertaken consistently as part of the recruitment process into the AFP. Required screening processes are not always taking place prior to an existing employee commencing in a high risk / specialist role with the AFP. Therefore the AFP is not provided with the assurance that all employees in these roles have been assessed as suitable for high risk roles.
11. Individual training courses have been developed by the Psychological Services team in response to operational requests in specific areas, however the AFP does not have a specific mental health training framework that identifies the competencies and resilience levels required by employees at different stages in their AFP career to inform delivery and prioritisation of training.
12. Current mechanisms used for identifying employees at risk of psychological injury are limited in effectiveness and do not occur routinely.
13. There are weaknesses with the AFP’s rehabilitation and return to work arrangements for employees suffering from a psychological injury sustained during their employment with the AFP. These relate to the lack of mental-health specific rehabilitation policies, procedures and training.
14. The AFP has a range of mental health support services available for employees to access. Recent employee feedback has indicated that the availability and effectiveness of these services is varied, and that there are no systemic arrangements to evaluate support service effectiveness on an ongoing basis. Feedback also indicated that cultural barriers to accessing support and assistance reduces the potential impact of these services.
15. Information on employee mental health is held across a range of disconnected information systems and multiple hardcopy records which make it difficult for the AFP to monitor and respond to emerging issues.
16. The AFP undertakes a range of internal reporting on mental health metrics and performance for internal oversight committees.
17. The external review currently being conducted of the AFP mental health support services, commenced in 2017, provides the AFP with the opportunity to inform the selection and resourcing of the most effective mix of support services to support the mental health needs of AFP employees.
Supporting findings
Governance and risk management
18. The AFP does not have in place an organisational health and wellbeing strategy which incorporates policies, programs and practices to address mental health risks. The AFP is developing a draft Mental Health Framework and Mental Health Strategic Action Plan, and finalisation of these is dependent upon the outcome of a review of AFP mental health services that was not yet finalised at the time of drafting this report.
19. The AFP has defined the roles and responsibilities of individual employees and managers at different organisational levels for supporting employee mental health. However, the AFP has not established a clear governance structure for decision-making, information sharing and oversight in relation to employee mental health arrangements. This includes both organisational and committee arrangements.
20. The AFP formally recognised mental health as a strategic risk to the organisation and began developing treatment actions in October 2016. This strategic risk identification has not led to substantive engagement by all functional areas. Employee mental health has not been consistently identified as a risk in the AFP’s functional risk assessments and it is not evident that the AFP is co-ordinating the management of mental health as a shared risk (that is, between Organisational Health and functional areas).
21. The AFP does not have arrangements to ensure resources and funding are aligned to key mental health risks.
22. AFP allocates centralised funding to the Organisational Health function to resource mental health support activities. Each functional / geographical area may choose to allocate a portion of its annual operating budget to employee mental health but there is no information or assurance that funding is being spent in line with risk.
Prevention, identification and return to work of psychological injury
23. The AFP has established employment screening processes for mental health but these are not fully effective. The AFP has in place structures for undertaking assessments to ensure that employees possess the physical and psychological competencies required for AFP work. ANAO analysis indicates that required psychological assessments are being undertaken consistently at the pre-employment stage, however are not being undertaken in all instances prior to internal staff movements into specialist roles with higher mental health risk profiles.
24. The AFP has arrangements in place for preventing psychological injury but these are not fully effective as the AFP does not have a specific mental health training framework as a pre-emptive measure to improve employee resilience.
25. The AFP relies on three key mechanisms for identifying employees at risk of psychological injury: employee self-reporting; supervisor observation; and mental health assessments and psychological debriefs following deployment. There are limitations that reduce the effectiveness of these mechanisms, specifically:
- cultural barriers that reduce the likelihood of AFP employees self-reporting psychological injury;
- limited training and support for supervisors in identifying and supporting employees at risk of psychological injury; and
- inconsistent delivery and tracking of mandatory mental health assessments and psychological debriefs.
26. There are weaknesses with the AFP’s rehabilitation and return to work arrangements for employees suffering from a psychological injury sustained during their employment with the AFP. In particular, the draft 2017 AFP Mental Health review identified the lack of mental health-specific rehabilitation policies and the absence of mental health training for rehabilitation case managers to allow them to inform, assess or guide appropriate return to work for staff with psychological injury. Improving return to work arrangements to support better outcomes for injured employees remains a challenge for all organisations.
Mental health support services
27. The services offered by the AFP are not fully effective in supporting employee mental health. The AFP has seven support services available to employees that have mental health support elements, in addition to a range of related initiatives. Feedback from the draft 2017 AFP Mental Health Review and audit interviews with AFP personnel indicates that the availability and effectiveness of these services is varied. There are no systemic arrangements to evaluate the effectiveness of support services on a regular basis.
28. The AFP does not have a framework in place to evaluate the effectiveness of mental health support services and management arrangements. In 2017 the AFP commenced an external review of mental health support services for employees. The review is examining the AFP support services. In 2017, AFP also undertook an internal review of the Confidant Network.
29. In developing the strategy for managing AFP employees’ health and wellbeing, the AFP should incorporate regular reviews of the effectiveness of the mental health support services, as well as evaluating the appropriateness of the overall mix of services in terms of coverage, use by employees and value for money.
30. The AFP’s information on employee mental health is held across a range of disconnected information systems and multiple hardcopy records which make it difficult for the AFP to monitor and respond to emerging issues in employee mental health.
31. The AFP holds data in areas such as workplace health and safety incident reporting, Comcare claims, unscheduled leave, exposure to critical incidents and explicit material and information on deceased personnel which, if linked and analysed appropriately, could assist in identifying known psychological injury risk factors. There is an opportunity for the AFP to conduct such analysis and inform more targeted monitoring and support services.
Recommendations
Recommendation no.1
Paragraph 2.21
The AFP develop a comprehensive organisational health and wellbeing strategy and governance arrangements based on an integrated approach to staff mental health and wellbeing which incorporates policies, programs and practices that address the AFP’s specific risk profile.
Australian Federal Police response: Agreed.
Recommendation no.2
Paragraph 2.34
The AFP analyse, define and report on mental health risks across the organisation in a consistent manner and develop arrangements to align employee mental health and wellbeing resources to areas assessed as highest risk. During this process the AFP should also assess the effectiveness of the existing controls and treatments used to mitigate mental health risks.
Australian Federal Police response: Agreed.
Recommendation no.3
Paragraph 3.22
The AFP implement a mandatory mental health training framework for all AFP employees, tailored to the various capability requirements throughout their career lifecycle that provides information on identifying signs and symptoms of mental health injury (in self and others) as well as guidance on how to conduct meaningful conversations with staff and colleagues about their mental health.
Australian Federal Police response: Agreed.
Recommendation no.4
Paragraph 3.46
The AFP develop formal processes to monitor and provide assurance that:
- employees in specialist roles have their psychological clearance in place before commencing in the role; and
- mandatory mental health assessments and psychological debriefs are undertaken for all those who require them, in a timely manner.
Australian Federal Police response: Agreed.
Recommendation no.5
Paragraph 4.40
The AFP, in reviewing available support service options, uses a risk-based approach to determine the optimal mix of services to target identified organisational mental health risks, including:
- linking the outcomes of that review with the development of an organisational health and wellbeing strategy;
- ensuring the health and wellbeing strategy also addresses the cultural change required to support and encourage employees to access mental health services when required, particularly after involvement in critical incidents or prolonged exposure to high-stress roles; and
- establishing performance measures for the selected support services, and implementing monitoring and evaluation arrangements to ensure those services are systematically assessed.
Australian Federal Police response: Agreed.
Recommendation no.6
Paragraph 4.64
The AFP:
- consolidate disparate systems and hard copy records in order to establish an electronic health records management system that allows a single point of access to high level health information for each AFP employee; and
- establish a strategy for analysing employee health information against data in areas such as workplace incident reporting, Comcare claims, unscheduled leave, exposure to explicit material and information on deceased personnel in order to assist in identifying and addressing known psychological injury risk factors.
Australian Federal Police response: Agreed.
Summary of entity response
32. The proposed audit report was provided to the AFP. An extract of the proposed report was provided to Davidson Trahaire Corpsych.
33. Formal responses to the proposed audit report were received from the AFP and Davidson Trahaire Corpsych. If the entity provided a summary response, these are below, with full responses provided at Appendix 1.
Australian Federal Police
Thank you for the opportunity to consider and provide comment to the proposed report to Parliament on Managing Mental Health in the Australian Federal Police. The high risk nature of the operational work undertaken by AFP employees carries an inherent risk of psychological harm and/or injury. To that end, I [the AFP Commissioner] welcome your report to assist myself and the AFP to continue to improve the support and services we provide to our staff to provide the highest level of safety and wellbeing for them. The AFP has provided a full response to the Australian National Audit Office addressing each recommendation, in addition to this summary response.
As your report highlights, there are unique considerations in the delivery of health and wellbeing services for high-risk organisations such as the AFP. The dynamic and evolving nature of crime means our support areas must be as agile, responsive and adaptable as possible. The AFP recognised the need for enhanced mental health support and in 2016 engaged Phoenix Australia to undertake a review of mental health in the AFP.
We acknowledge that the AFP needs to change in order to meet the growing demand and complexity of the environment in which the AFP operates. Even within current staffing levels, the AFP is working under immense pressure and ongoing activity at current operational tempo will increase health risks for its staff.
We have invested significant resourcing over many years in employee health however know we have some way to go in this journey. I thank the Australian National Audit Office for prioritising the mental health of AFP employees in producing this report. The senior leadership group and I are committed to prioritising and protecting the mental health of all our employees.
Key learnings for all Australian Government entities
Below is a summary of key learnings and areas for improvement identified in this audit report that may be considered by other Commonwealth entities in managing the mental health of employees.
Governance and risk management
Contract management
Records management
1. Background
Introduction
1.1 Managing employee mental health effectively is a challenge faced by policing and first responder organisations around the world. This includes the Australian Federal Police (AFP) as the Australian Government’s primary policing agency responsible for the enforcement of Commonwealth laws and the protection of Australian interests from criminal activity, both domestically and overseas. To fulfil this role the AFP is responsible for a diverse range of functions, the delivery of which place a range of unique demands and stressors on AFP employees.
1.2 Safe Work Australia’s Work-Related Mental Disorders Profile 2015 concluded that first responders—police, emergency and health services—were the combined occupational group most likely to make a workplace compensation claim based on mental health injury, with incidence rates and costs substantially exceeding other occupational groups.
1.3 The AFP employed 6540 staff, both sworn officers and professional staff1, as at 30 June 2017.
Defining mental health
1.4 Good mental health is defined by the World Health Organization as:
a state of well-being in which every individual realizes his or her own potential, can cope with the normal stresses of life, can work productively and fruitfully, and is able to make a contribution to her or his community’.2
1.5 Mental illness refers to a health condition, diagnosed to standardised criteria, that significantly affects how a person feels, thinks, behaves, and interacts with others. Mental health problems interfere with a person’s thinking, feeling and behaviour but to a lesser extent than mental illness. Mental health problems are less severe, but left untreated can develop into mental illness. Mental health problems can be an individual’s temporary responses to external stressors.3
1.6 In this report the term ‘mental health’ is used to reflect a spectrum of conditions, rather than focusing solely on acute presentations of injury. The term ‘psychological injury’ is used consistently with Comcare4 terminology, which defines it as ‘a range of conditions relating to the functioning of people’s minds. While often prompted by workplace stressors, these conditions can be caused by physical injuries, disease, exposure to toxins or underlying psychiatric issues’.5
Mental health in the workplace
1.7 Employee mental health is closely linked to a range of factors that are both individual and organisational. In particular, an entity’s organisational culture, which consists of leadership and management practices as well as organisational structures and processes (such as appraisal and recognition processes, decision-making styles, clarity of roles, and goal alignment), has a strong influence on employee wellbeing and mental health. An individual’s physical health, personal situation and cultural environment all interact with and shape overall wellbeing.6 The term ‘organisational health’ in this report therefore refers to both the organisational and individual factors that contribute to employee wellbeing and organisational performance, as shown in Figure 1.1.
Figure 1.1: Factors influencing employee wellbeing and performance

Source: ANAO analysis based on World Health Organisation and academic research.
1.8 Studies have investigated the relative contributions of organisational culture, employment experiences, personality and coping strategies to levels of wellbeing among police officers. These studies indicated that organisational culture exerted the strongest influence on overall levels of wellbeing for police officers. The interaction between exposure to traumatic incidents and negative organisational experiences has been described in academia as the ‘erosive stress pathway’, which can accelerate mental health injury.7
1.9 The 2016 Victoria Police Mental Health Review identified that mental health risks were associated with operational incident exposure levels, personal stressors and organisational stressors, ‘particularly leadership behaviours, co-worker interactions, tolerance level for bad (counter-productive) behaviours and workload pressures’. In contrast, ‘supportive leadership styles and a positive high quality team climate serve[d] as protective factors’.8 The Queensland Audit Office report, Managing the mental health of Queensland Police employees, noted that the nature of first responders’ work, ‘both the tasks (situational stressors) and conditions (organisational stressors, such as shift work and work culture)—can pose a significant threat to mental health’.9
1.10 These review findings were consistent with concerns raised by current and former AFP employees that organisational stressors were also a contributor to their mental health, or compounded situational stressors.10
Mental health and the AFP
1.11 The AFP operates in a high risk environment for employee mental health given the diverse range of functions it is responsible for delivering—as outlined in Table 1.1. These functions place a varied range of demands and stressors on AFP employees, which are unique compared to the majority of other Australian Government entities.
Table 1.1: Summary of AFP functions
|
AFP functionsa |
|
|
Operations |
|
|
Protection and security |
|
|
Operational/specialist support |
|
|
International operations |
|
|
Other support services |
|
Note a: Table 1.1 lists AFP functions in generalised categories and does not reflect the AFP’s organisational or reporting structure.
Note b: This includes Christmas Island, Cocos (Keeling) Islands, Norfolk Island and Jervis Bay.
Note c: Personal protection in Australia and overseas for Australian high-office holders, Commonwealth public officials and foreign dignitaries in Australia.
Note d: Physical security for Commonwealth facilities such as Australian Parliament House, defence facilities and for diplomatic missions in Australia.
Note e: Planning and provision of security for designated special events, such as the Olympic and Paralympic Games.
Note f: Includes: tactical response; search and rescue disaster response; detection dogs; police negotiation; bomb response; maritime (water and dive) response; communications response; and air security officers.
Note g: AFP maintains a network of liaison officers located across 29 countries.
Source: ANAO analysis of AFP documentation.
1.12 The nature of the AFP’s functions result in staff being exposed to traumatic events such as:
- crime scenes and deceased persons;
- child exploitation material;
- terrorism material;
- victims of crime and their families;
- disaster and accident scenes;
- violence against police;
- extreme violence with limited powers to respond (overseas); and
- remote and isolated work environments in Australia and overseas.11
1.13 Exposure to traumatic events can occur repetitively over an AFP employee’s working life, which can then be associated with an increased vulnerability to the cumulative effects of such incidents both during the employee’s career and post career.12
1.14 The wide geographical distribution of AFP staff across both Australia and overseas, and the differing stressors and traumas to which they may be exposed, present a unique challenge for the AFP in providing appropriate mental health support services to its staff and identifying when and where these support services are required.
Work health and safety framework
1.15 Under the Work Health and Safety Act 2011, the AFP has the primary duty of care to ensure, so far as is reasonably practical, the health and safety of its workers while they are at work, including both physical and psychological health. Comcare and the Safety, Rehabilitation and Compensation Commission are established under the Safety Rehabilitation and Compensation Act 1988 (SRC Act), and jointly administer the statutory framework for rehabilitation and workers’ compensation for all Commonwealth entities, including the AFP.13
1.16 Where an AFP employee has a work-related injury or illness, they may seek support to recover from the injury or illness by making a claim to Comcare. The Comcare benefits and entitlements may include: medical expenses, travel costs, household and attendant care, assistance aids or modifications, incapacity benefits, permanent impairment and death benefits. Comcare makes a determination under the SRC Act as to whether an injury claim is accepted or rejected. In 2016–17 Comcare took an average of 54 days to reach a determination for accepted psychological injury claims made by AFP employees—down from 125 days in 2007–08. If an injury claim is rejected, Comcare has a process for reviewing determinations.
1.17 The AFP has experienced an increase in the number of Comcare claims for psychological injury, and in the costs claimed by employees that are related to psychological injury—as shown in Figure 1.2 and Figure 1.3. In 2007–08 there were 11 AFP claims related to psychological injury that were approved by Comcare at a cost of $2.8 million. By 2016–17 this had increased to 35 claims approved with an associated cost of $16.7 million.14 Figure 1.3 illustrates the variability in claim costs between years.
Figure 1.2: AFP injury claims accepted by Comcare by injury type, 2007–17

Source: ANAO analysis of AFP Comcare data.
Figure 1.3: Total cost of AFP Comcare claims, 2007–17
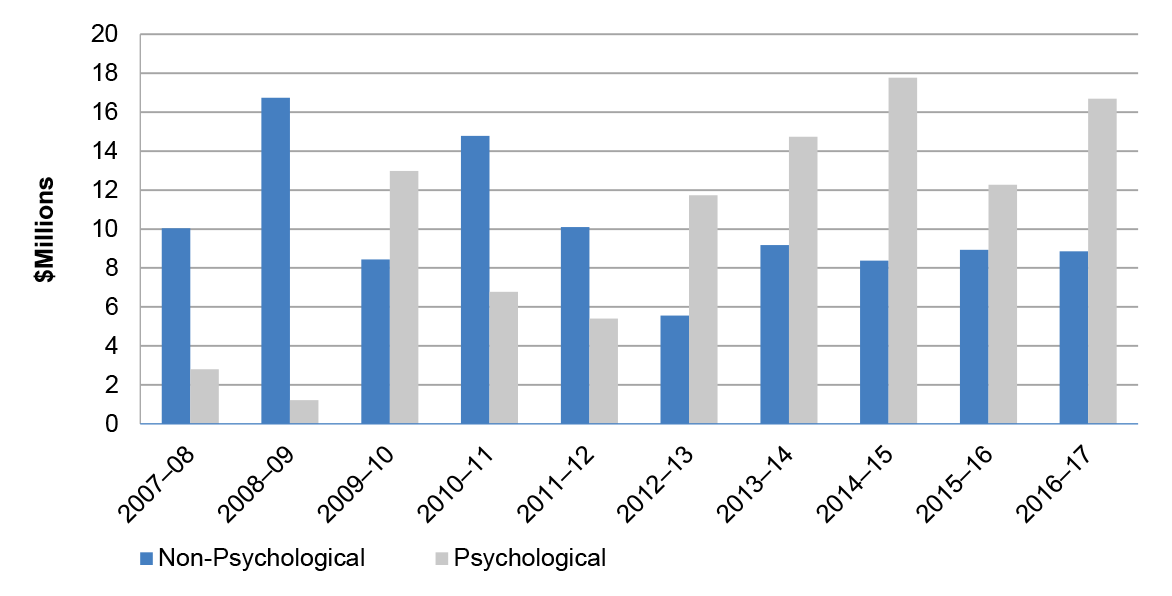
Source: ANAO analysis of AFP Comcare data.
1.18 As the above Comcare data only includes accepted claims from AFP employees, it may not reflect the actual number of AFP employees experiencing psychological injury, or the associated costs to those employees. AFP employees not reporting psychological injury to Comcare may be a result of barriers to employees seeking help, as discussed in paragraph 3.25. The number of AFP employees that have or are seeking support externally to the AFP, or not seeking assistance at all, is unknown.
AFP reviews
Cultural change review
1.19 In August 2016 the AFP undertook a review, Cultural Change: Gender Diversity and Inclusion in the Australian Federal Police, which examined AFP culture and diversity. The scope of the review did not examine employee mental health, although some of the findings relate to employee mental health. The review findings included:
- a ‘trust deficit’ between members and leaders, particularly with senior leaders;
- the need for change to the AFP’s recruitment, promotion and training process to emphasise the importance of people management and leadership skills;
- noting that the majority of female employees interviewed feel they are not able to thrive equally with male colleagues;
- high level of female employees—46 per cent of female survey respondents—reporting experiencing sexual harassment in the workplace in the last five years—a result which is higher than the broader Australian workforce;
- a culture that makes reporting incidents, including sexual harassment, unsafe. In addition, internal integrity investigations can be protracted, which can be a disincentive for members to report incidents;
- poor performers not being appropriately managed;
- structural and cultural obstacles, including a strong stigma, that limit employees’ (all genders) ability to access flexible work arrangements; and
- three in five staff having experienced bullying in the workplace.
1.20 The AFP Commissioner has accepted all 24 recommendations in the report and committed to ensuring that each is implemented. The AFP has set out an implementation plan, and is regularly reporting on progress. As at July 2017, 8 recommendations had been implemented, with the remainder pending or in progress.
AFP activities to improve employee mental health
1.21 In February 2017, AFP Commissioner Colvin noted that it is ‘widely acknowledged that police are at a higher risk of trauma-caused mental injury than almost any other profession’ and that the health and wellbeing of AFP staff is of the highest priority.15 In recognising that it faces a significant challenge in managing the mental health of its employees, the AFP has commenced a range of activities intended to improve how it supports employee health and wellbeing. In September 2016, the AFP began developing a draft Mental Health Framework and associated Mental Health Strategic Action Plan based on Beyond Blue’s Good practice framework for mental health and wellbeing in first responder organisations.
1.22 To inform the design of the Framework and Strategic Action Plan, in March 2017 the AFP engaged a contractor to review the quality and employee perceptions of its mental health support services.16 The review included an examination of the literature associated with mental health in policing; review of AFP documentation; face to face consultations with senior AFP leaders; focus groups with AFP employees and an online survey seeking AFP employees’ views of support services, with the report not yet completed at the time of drafting this audit.17 Finalisation of the framework and associated action plan is pending the outcome of this review; as such the AFP executive has not been in a position to consider its approval and implementation.
1.23 In February 2017, the AFP established a Mental Health Strategy Board intended to ‘direct all aspects of the AFP Mental Health Strategy including an independent review’ and to ‘oversight the implementation of the review recommendations’.18
1.24 In June 2017, the AFP commenced an informal pilot project to track employee exposure to critical or potentially traumatic incidents. The project involved AFP’s Organisational Performance and Organisational Health areas. The project was prompted by academic research indicating that cumulative exposure to traumatic events increases the risk of psychological injury, with rates of Post-Traumatic Stress Disorder and depression increasing with each additional traumatic exposure. AFP employees conducted an exercise to combine data from its policing case management system with time charging records to see how many hours AFP members are charging to particular types of cases, and attendance at critical incidents. The purpose was to use this information to improve the targeting and timeliness of intervention support to members who may be at risk from cumulative exposure to traumatic events and/or material.
1.25 Recognising the need for better identification of physical and mental health risks across the AFP, in mid-2017, the AFP’s Organisational Health area:
- seconded a staff member from the Strategic Risk section to develop Organisational Health’s capacity to assess needs for services; and
- commenced development of an informal pilot program to assess work stresses in a given operational area, in order to target future interventions. The pilot is taking place in the Forensics area, Telephone Intercept and ACT Policing areas, as these have been identified by AFP psychologists as potential high risk areas.
1.26 In July 2017, the AFP officially launched an expanded Welfare Officer Network (the network previously comprised two officers supporting ACT Policing employees). The network now comprises 22 Welfare Officers across the ACT, NSW, Victoria, Western Australia, South Australia, Cairns and Brisbane. Services from Welfare Officers extend to Darwin, Geraldton, Exmouth and international posts.
1.27 In October 2017, the AFP made available a free wellbeing app, Equipt, for current and former AFP employees and their families. The app is a self-help tool to assist individuals with tracking their physical, emotional and social wellbeing.19 The AFP in partnership with the Australian Federal Police Association, have licenced the app from Victoria Police and The Police Association of Victoria, tailoring aspects to meet AFP needs.
Audit approach
1.28 The objective of the audit was to examine the effectiveness of the AFP in managing the mental health of its employees. To form a conclusion against the audit objective, the ANAO adopted the following high-level audit criteria:
- Has the AFP implemented sound governance and risk management practices to manage employee mental health?
- Is the AFP effectively managing employee mental health throughout their career lifecycle?
- Are sound monitoring, reporting and evaluation arrangements in place to assess the effectiveness of the AFP’s management of mental health?
1.29 The scope of this audit is the management of employee mental health by the AFP. It addresses high-level management and coordination of programs explicitly supporting mental health. The ANAO did not evaluate or form conclusions against organisational stressors within the AFP. The ANAO did not review Comcare services or claims processes, as these are not directly within the control of the AFP.
1.30 The ANAO conducted this audit to contribute to work being undertaken in other audit jurisdictions relating to the mental health of first responders, including the Queensland Audit Office, and the Audit Office of New South Wales.20 The Office of the Auditor-General of Canada was also conducting work in this area. The selection of this audit also reflects the significant risks and costs faced by the AFP in managing employee mental health, as evidenced by increasing rates of Comcare psychological injury claims in recent years.
1.31 In conducting this audit, the ANAO reviewed AFP documentation, interviewed key AFP personnel and relevant stakeholders at AFP national headquarters in Canberra and regional AFP sites in Adelaide, Alice Springs, Darwin, Melbourne, and Sydney. The audit team conducted 102 interviews with AFP personnel and received 66 public submissions to the audit.
1.32 The audit was conducted in accordance with the ANAO Auditing Standards, at a cost to the ANAO of approximately $705,268.00.
1.33 The team members for this audit were Anna Peterson, Jess Scully, Lachlan Fraser, Jerry Liao and Paul Bryant.
2. Governance and risk management
Areas examined
The ANAO assessed the AFP’s governance arrangements for managing employee mental health, and its management of mental health risks.
Conclusion
While currently developing a mental health framework, the AFP has not established a clear governance structure for decision-making, information sharing and oversight in relation to employee mental health arrangements. Reporting into the governance structure is not comprehensive or risk-based, making it difficult to identify emerging mental health related risks and to utilise this reporting to inform decision making in resource prioritisation to address increasing mental health risks.
The AFP formally included mental health as a strategic risk to the organisation in October 2016, however this risk identification has not led to substantive engagement and coordinated identification of mental health risks faced by all of the AFP’s functional areas.
The AFP does not currently have in place mechanisms or sufficient data to appropriately align resources with key mental health risks.
Areas for improvement
The ANAO made two recommendations aimed at improving AFP’s strategic and governance arrangements for managing employee mental health, as well as for enhancing its management of mental health risks.
Does the AFP have an organisational health and wellbeing strategy in place that incorporates mental health?
The AFP does not have in place an organisational health and wellbeing strategy which incorporates policies, programs and practices to address mental health risks. The AFP is developing a draft Mental Health Framework and Mental Health Strategic Action Plan, and finalisation of these is dependent upon the outcome of a review of AFP mental health services that was not yet finalised at the time of drafting this report.
Draft Mental Health Framework and Strategic Action Plan
2.1 In September 2016 the AFP developed a draft Mental Health Framework and associated Mental Health Strategic Action Plan based on Beyond Blue’s Good practice framework for mental health and wellbeing in first responder organisations. The purpose of the draft framework was to ‘reset the direction in the AFP for mental health’, and the action plan outlined initiatives intended to strengthen the AFP’s commitment to mental health.
2.2 The draft framework and action plan were presented to the AFP’s Executive Leadership Committee on 13 September 2016. The documents were discussed but not approved, with the rationale for this decision not clear from the meeting minutes.
2.3 In March 2017 the AFP commenced a review of the quality and perceptions of its mental health support services. The review included an examination of the literature associated with mental health in policing; review of AFP documentation; face-to-face consultations with senior AFP leaders; focus groups with AFP employees and an online survey seeking AFP employees’ views of support services.21 Once finalised, the review will inform the design of the draft framework and action plan. In revising the framework and action plan, the AFP should consider how these documents could fit within an overarching organisational health and wellbeing strategy (as discussed below).
2.4 In September 2017, the AFP provided a status update to the ANAO regarding progress against each of the activities listed in the draft plan. However, as the framework and plan have not yet been finalised or approved—pending the outcome of the review, this progress reporting is not currently being monitored or reviewed through any formal mechanisms.
Organisational health and wellbeing strategy
2.5 The AFP does not have in place a formal organisational health and wellbeing strategy, which incorporates policies, programs and practices to address the AFP’s mental health risks.
2.6 In early 2017, the AFP developed a draft concept paper called ‘Road2Ready – Physical Health Concept Paper 2017 – 2020’. This concept paper proposes an ‘AFP physical health model’ and acknowledges the interaction of physical, psychological and community health. However, the paper is primarily focused on physical health and has limited information on psychological health or broader elements of organisational health. Although the paper does reference the mental health framework, it is unclear how the draft mental health framework and the ‘Road2Ready’ concept paper are linked.
2.7 The AFP would benefit from developing a strategy which recognises that mental health is a component of overall employee wellbeing, and that mental health is impacted by a range of factors including organisational climate, physical health and personal circumstances. The strategy should capture the reforms and activities already underway to ensure that desired improvements to employee wellbeing are achieved over the long term.
Are clear governance arrangements in place to manage responsibilities in relation to mental health?
The AFP has defined the roles and responsibilities of individual employees and managers at different organisational levels for supporting employee mental health. However, the AFP has not established a clear governance structure for decision-making, information sharing and oversight in relation to employee mental health arrangements. This includes both organisational and committee arrangements.
Responsibilities
2.8 The AFP is required to protect workers and other persons against harm to their health, safety and welfare through the elimination or minimisation of risks arising in the course of their employment under the Workplace Health and Safety Act 2011 (WHS Act).
2.9 The AFP has guidelines in place that articulate the roles and responsibilities of workers, managers, team leaders and coordinators in relation to supporting the physical and psychological health of employees. Examples include the National Guideline on AFP Health and Safety Management Arrangements.
Governance arrangements
Organisational level
2.10 There are a number of distinct teams that contribute to the AFP’s management of employee wellbeing and mental health. As discussed in Chapter 4 and outlined in Figure 2.1, these include Psychological Services, the Welfare Officer Network, Employee Assistance Program, Chaplaincy, Safe Place, the Confidant Network and the recently established (in August 2017) Organisational Health Triage team.
Figure 2.1: Organisational structure for the management of employee wellbeing and mental health

Source: ANAO analysis of AFP documentation.
2.11 As outlined in Figure 2.1, many of the health and wellbeing components are managed by Organisational Health and the Chief Medical Officer, under the National Manager People Safety and Security, while Safe Place and the Confidant Network are managed by the National Manager Reform, Culture and Standards who reports directly to the Commissioner. There is no formalised governance mechanism in place to support co-ordination, information sharing and reporting between the two interrelated business areas. Having two separate business areas that focus on employee wellbeing and mental health may reduce the ability to co-ordinate the AFP’s activities to address employee wellbeing, including mental health, but also to identify employees at risk. There would be benefit in the AFP reviewing the organisational structure and co-ordination of these business areas.
Committee level
2.12 The AFP’s governance structure is characterised by a range of committees at the national and regional level. The committees with functions relevant to organisational and mental health are outlined in Appendix 2. The ANAO’s analysis of these committees’ Terms of Reference, meeting minutes and agenda papers between August 2016 and September 2017 found that their decision-making responsibilities and reporting arrangements in relation to employee mental health and wellbeing have not been clearly documented.
2.13 The ANAO’s analysis found that it is not clear which committee has the primary responsibility for the governance of employee mental health and wellbeing. The AFP advised that the National Safety Committee (NSC) has oversight of all employee health matters under WHS legislation. The committee Terms of Reference do not mention employee mental health or wellbeing.22 The committee focuses on reviewing reported work health and safety incident statistics, compensation claim statistics and physical injury risks presented by operational equipment. While there is some discussion of mental health matters, these are not undertaken in line with a long-term perspective and established priorities for action.
2.14 The AFP also advised that Regional Safety Committees (RSCs) report to the NSC. There was no evidence from the agenda papers or minutes that the NSC considered matters raised at RSCs.
2.15 Review of committee agenda papers and minutes further identified that there is no committee which receives a complete reporting picture on employee mental health matters, and that reporting on the performance of support services is not consistently shared between the committees.
2.16 The Functional and Efficiency Review of the AFP, finalised in November 2016, identified similar concerns in relation to the AFP’s governance and committee arrangements, in particular with the clarity of committee accountabilities, responsibilities and discipline. The AFP is currently preparing a fully costed response to the review for government consideration by the end of 2017.
2.17 An internal review of the AFP’s committee structure is currently underway but has not yet been finalised. As part of the broader review, the AFP should incorporate opportunities to improve its governance arrangements for organisational health including employee mental health and wellbeing.
Functional and Geographic level
2.18 AFP functional areas and regional offices hold responsibilities for the physical and psychological health of AFP employees.
2.19 AFP functional areas, such as Counter Terrorism or Protection Operations, are led by a National Manager (SES Band 2) who, along with the AFP Commissioner and Deputy Commissioners, are considered to be Officers (Senior Executive) under the WHS Act 2011. Officers are required to take reasonable steps to gain an understanding of the hazards and risks associated with the business and ensure that the business has and uses appropriate resources and processes to eliminate or minimise risks to health and safety (that is both risks to physical and psychological health).
2.20 Regional offices are run by State Managers (SES Band 1). Under the WHS Act 2011, Managers are considered to be Workplace Supervisors and are similarly required to eliminate health and safety risks from the workplace, and where this is not reasonably practicable, take all reasonably practicable steps to effectively minimise the risks.
Recommendation no.1
2.21 The AFP develop a comprehensive organisational health and wellbeing strategy and governance arrangements based on an integrated approach to staff mental health and wellbeing which incorporates policies, programs and practices that address the AFP’s specific risk profile.
Entity response: Agreed.
2.22 I [AFP Commissioner] wish to highlight the progress AFP had made prior to the commencement of the 2017 audit. In 2016, we developed a Mental Health Strategy and engaged Phoenix Australia to undertake a review of mental health in AFP. Concurrently, KPMG was engaged to conduct a review of the AFP governance framework. The formal engagement of Phoenix Australia predates this audit and demonstrates my commitment to mental health reform.
2.23 The AFP will finalise the mental health strategy and associated policies, programs and practices incorporating the relevant recommendations of the Phoenix Australia review, lessons drawn from other policing and first responder agencies both nationally and internationally and this audit.
2.24 We acknowledge that the current governance arrangements are complex and do not clearly identify lines of accountabilities in the area of mental wellness. KPMG was engaged in 2017 to conduct a review of the AFP governance framework and this review will inform the mental health strategy to ensure clear lines of accountability.
Does the AFP identify, assess and prioritise key risks relating to mental health?
The AFP formally recognised mental health as a strategic risk to the organisation and began developing treatment actions in October 2016. This strategic risk identification has not led to substantive engagement by all functional areas. Employee mental health has not been consistently identified as a risk in the AFP’s functional risk assessments and it is not evident that the AFP is co-ordinating the management of mental health as a shared risk (that is, between Organisational Health and functional areas).
Risk management framework
2.25 The AFP’s risk management framework comprises four levels of assessment: entity; functional; program; and specific operations. The Enterprise Risk Profile outlines the AFP’s risk exposure at an entity level, with four categories of strategic risk identified.23 Each functional and program area is to undertake a risk assessment and develop a risk assessment and treatment plan (risk register), based on the template provided as part of the guidance material. In line with the Commonwealth Risk Management Policy the AFP has defined its risk appetite and tolerance, with risks rated above ‘medium’ expected to have a specific treatment plan in accordance with the AFP’s Risk Assessment Tool. The AFP targeted an ‘integrated’ level of risk management maturity in the Comcover Risk Management Benchmarking Survey 2017, and was assessed as meeting this standard based on its survey responses.
Identifying and monitoring mental health risks
Entity level
2.26 Risks to employee mental health were formally identified at an entity level in October 2016 following the increasing number and cost of accepted Comcare psychological injury claims and a growing Comcare premium.
2.27 As at August 2017, the AFP’s Enterprise Risk Profile identifies mental health injury as one of 22 entity level risks.24 Risk controls have been documented, and further treatments are proposed. The identified treatments primarily involve changes to the delivery of training and support networks, and the integration of organisational and mental health considerations in policies and processes. Despite the risk of mental health injury being considered ‘High’, only two of the planned risk treatments are expected to be implemented in 2017–18. Five of the nine identified treatments are not due until 2022.
Functional level
2.28 The entity level recognition of mental health is not consistently reflected in functional risk assessment and treatment plans. Comcare mental health injury claims data shows that of the 20 functional areas within the AFP, ACT Policing, Protection Operations, Specialist Operations, and International Operations were among the functional areas with the highest number and cost of compensation claims for mental health injuries. Despite this, these four functional areas did not specifically identify mental health as an area of risk in their risk assessment and treatment plans. Crime Operations, also identified as an area with a high number and cost of compensation claims for mental health injury, did identify staff mental health as a specific area of risk and had identified specific controls and treatments for this risk.
2.29 Where employee mental health has been identified as a concern within functional risk assessments, there remains scope to improve the specificity of controls and treatments.25 Examples were identified where the listed treatment control referenced existing procedures or policies, and did not clearly illustrate how the control mitigated the identified risk. For example, existing controls identified in the risk assessment for Organised Crime and Cyber include ‘adhere to AFP Reform – Safe Place Initiative … Adhere to policy and procedures’.26 On the positive side, many new treatments identified were more specific and listed actions or interventions with clear correlations to the mitigation of the identified risk. For example, Crime Operations identified the risk that exposure to certain work types could have negative mental health impacts, and proposed assessments for exposed staff and the introduction of software and systems to limit staff exposure. The AFP is not assessing whether the functional risk plans are being implemented, and whether identified mitigations are effective.
2.30 Further, there is a lack of clarity as to which aspects of risk treatments the functional areas are responsible for. For example, ACT Policing’s risk treatment plan for risks to employee physical and mental health states that ‘Risk Treatment initiatives being undertaken through enterprise wide Organisational Health projects […] will contribute to covering this risk for ACTP’, but does not specify how the initiatives that will specifically reduce ACT Policing’s risks.27
Organisational Health’s management of mental health risk
2.31 The ANAO’s review of AFP functional risk assessments identified that engagement with the Organisational Health team does not appear to have been formally prioritised in the functional areas of greatest risk within the AFP. Organisational Health has recognised the need for better identification of physical and mental health risks across the AFP. To achieve this, the Organisational Health area:
- has seconded a staff member from the AFP’s Strategic Risk section to develop the section’s capacity to assess needs for services; and
- is developing an informal pilot program to assess work stresses in a given operational area, in order to target future interventions. The pilot is taking place in the Forensics, Telephone Intercept and ACT Policing areas, as these has been identified by AFP psychologists as a potential high risk areas.
Does the AFP have an effective framework to align resources with key mental health risks?
The AFP does not have arrangements to ensure resources and funding are aligned to key mental health risks.
AFP allocates centralised funding to the Organisational Health function to resource mental health support activities. Each functional / geographical area may choose to allocate a portion of its annual operating budget to employee mental health but there is no information or assurance that funding is being spent in line with risk.
2.32 AFP provides centralised funding through a reccurring allocation to the Organisational Health function in order to resource core activities related to employee mental health across the AFP.
2.33 Separately, each functional or geographical area is allocated an annual operating budget, and each area is then responsible for determining what proportion of this funding to allocate to employee mental health at the operational level. No specific funding amounts are allocated for functional or geographical areas to spend on employee mental health. There is no available information on the extent to which each functional / geographical area allocates any of its annual operating budget to employee mental health. There is no assurance that appropriate funding is spent on employee mental health in functional / geographical areas and prioritised in alignment with the areas’ different mental health related risk profiles.
Recommendation no.2
2.34 The AFP analyse, define and report on mental health risks across the organisation in a consistent manner and develop arrangements to align employee mental health and wellbeing resources to areas assessed as highest risk. During this process the AFP should also assess the effectiveness of the existing controls and treatments used to mitigate mental health risks.
Entity response: Agreed.
2.35 The AFP continues to strengthen its governance and risk framework following the KPMG review of governance. I [AFP Commissioner] am committed to better management of mental health as a strategic risk and will adopt a risk-based approach to the delivery of services.
2.36 We continue to refine the mental health services, support and policies for our employees and I am committed to enhancing that support further to counter new and emerging mental health challenges. The development of the Mental Health Strategy and the engagement of Phoenix Australia to undertake a review of mental health in AFP assist me to realise my commitment to my workforce and to their safety and wellbeing.
3. Prevention, identification and return to work of psychological injury
Areas examined
This chapter assesses the effectiveness of the AFP’s arrangements for preventing and identifying psychological injury among employees through an examination of employment screening processes, mental health prevention and identification activities, and return to work processes for employees who have experienced a psychological injury.
Conclusion
Screening processes are in place to assess the suitability of employees’ psychological readiness for sworn roles. These are undertaken consistently as part of the recruitment process into the AFP. Required screening processes are not always taking place prior to an existing employee commencing in a high risk / specialist role with the AFP. Therefore the AFP is not provided with the assurance that all employees in these roles have been assessed as suitable for high risk roles.
Individual training courses have been developed by the Psychological Services team in response to operational requests in specific areas, however the AFP does not have a specific mental health training framework that identifies the competencies and resilience levels required by employees at different stages in their AFP career to inform delivery and prioritisation of training.
Current mechanisms used for identifying employees at risk of psychological injury are limited in effectiveness and do not occur routinely.
There are weaknesses with the AFP’s rehabilitation and return to work arrangements for employees suffering from a psychological injury sustained during their employment with the AFP. These relate to the lack of mental-health specific rehabilitation policies, procedures and training.
Areas for improvement
The ANAO has made two recommendations aimed at improving mental health training for AFP employees and developing processes for providing assurance that mandatory psychological clearances, mental health assessments and psychological debriefs are undertaken in a timely manner.
The ANAO also suggests that the AFP monitor the long-term exposure of its employees and implement workforce planning for specialist roles. Additionally, the ANAO suggests that the AFP work closely with other policing jurisdictions to identify mechanisms for ongoing monitoring of the psychological health of general duties officers.
Does the AFP have effective and integrated employment screening for mental health?
The AFP has established employment screening processes for mental health but these are not fully effective. The AFP has in place structures for undertaking assessments to ensure that employees possess the physical and psychological competencies required for AFP work. ANAO analysis indicates that required psychological assessments are being undertaken consistently at the pre-employment stage, however are not being undertaken in all instances prior to internal staff movements into specialist roles with higher mental health risk profiles.
3.1 All AFP employees are required to possess and maintain a standard of health, wellbeing and physical fitness that enables them to fulfil their job requirements competently and safely. The Australian Federal Police Act 1979 (Cth)28 enables the AFP to establish various conditions and competency requirements for employment, including: a medical assessment, a physical competency assessment and a psychological assessment.
3.2 The ANAO’s examination focused on the psychological assessment element of the employment screening process, which aims to assess an employees’ psychological readiness for policing roles.
Psychological assessments / clearances
3.3 The AFP National Guideline on medical, psychological and physical competency assessments requires that psychological assessments (also known as psychological clearances) must be conducted:
- prior to an applicant joining the AFP (pre-employment); and
- prior to an AFP employee being assigned to designated specialist operational roles, and designated non-operational support roles (an internal clearance).29
3.4 The nature of the psychological assessment varies depending on whether it is for pre-employment or as part of an internal clearance to a specialist role:
- For all recruitment in relation to sworn positions—candidates who are found suitable at the AFP Assessment Centre proceed to a psychological assessment. This assessment consists of two, short psychometric tests and a face-to-face interview with a psychologist from an external Health Provider. All candidates must undertake this psychological assessment and be assessed as suitable prior to being offered a new recruit role. This arrangement has been in place since 2009.
- For recruitment in relation to non-sworn / professional positions—there is no psychological assessment process for external applicants for non-sworn / professional positions. Once a non-sworn employee has joined the AFP, if they wish to transfer to certain specialist roles, they go through the process for an internal psychological clearance (see below).
3.5 For an internal clearance to transfer to certain specialist roles (see Box 1 below)—AFP Recruitment or the AFP Business Area advises the Psychological Services team that a psychological clearance is required. An initial check is undertaken by Psychological Services of the employee’s psychological data stored in the Clearance database, the PLANES database, Comcare’s Customer Information System (CIS) and on hard copy files.30 The employee is then required to complete a Psychological Services Assessment Form31 which is reviewed by Psychological Services and an assessment interview32 may be undertaken.
3.6 For certain specialist roles such as child protection there is an additional online test33, a face-to-face assessment interview by an AFP registered psychologist (which is mandatory) and graduated exposure to explicit materials. There is a Standard Operating Procedure (SOP) on Graduated Exposure to Child Exploitation Material.
3.7 The clearance process for Child Protection Operation (CPO) members, including the Joint Anti-Child Exploitation Taskforce (JACET), has three steps. The employee may choose to withdraw from the process at any point:
- Step 1: Organisational Health clears the employee to commence the graduated exposure exercise. A determination to proceed is made based on the results of the online tests, such as those outlined in paragraph 3.6, and a face-to-face interview with an AFP psychologist;
- Step 2: The business area commences part one of the graduated exposure program with the employee. This should be conducted by a senior or experienced member of the CPO team in the relevant office. The employee is debriefed by an AFP psychologist; and
- Step 3: The business area commences part two of the graduated exposure program with the employee. The employee is debriefed by an AFP psychologist and, if appropriate, has their clearance signed off. The AFP’s SOP states ‘everyone undergoes the graduated exposure exercise before they commence in child protection operations work. The member is not to be exposed to explicit material before they have been psychologically cleared or completed the graduated exposure exercise. Furthermore, the clearance has to have been received by the CPO member conducting the process in writing’.
|
Box 1: AFP business areas requiring a psychological assessment and clearance |
|
|
|
3.8 The ANAO’s analysis of the AFP’s PLANES database, which holds information on the use of psychological services and related consultations for AFP employees, showed that in 2016–17, Psychological Services undertook 530 psychological clearances. The majority were for employees working in International Operations (381), followed by ACT Policing (43), Specialist Operations (36) and Crime Operations (32).
3.9 Psychological assessment occurs consistently as part of the pre-employment recruitment process for sworn positions. However, psychological assessments are not occurring consistently for internal staff movements into specialist roles. ANAO analysis showed that 34 per cent (13 of 38) of current JACET employees34 did not have a recorded psychological clearance registered against their name in the PLANES database. The AFP reviewed the relevant files for those 13 employees and advised the current status of the clearances as follows:
- four employees had been cleared but due to practitioner oversight or system error, the clearance had not been recorded in PLANES;
- four employees had been cleared prior to establishment of PLANES and so there was no record in the database;
- one employee was not cleared to work in JACET but the business area did not accept the AFP psychologist’s recommendation;
- three employees had completed one or two of the clearance steps but had not had final sign off on their clearance from an AFP psychologist; and
- one employee withdrew from the clearance process after step 2 but it was not clear whether that individual was still working in JACET.
3.10 As recently as October 2017, the AFP Mental Health report made to the National Safety Committee, states that:
On several occasions Psychological Services have been requested to clear members after they have commenced in Child Protection Operations roles. This potentially places members at risk of exposure associated with this type. Psychological Services have reminded Coordinators of the importance of clearance prior to exposure.35
3.11 Further, in 2015 the AFP noted36 that there were identified instances where business areas, in trying to meet their outcomes, decided to progress with an individual for a task who had not cleared employment gateways. The minute paper states that the non-compliance arises for one of two primary reasons:
- insufficient lead time to clear selected staff prior to the requirement; and
- during the clearance process, delays occur because of follow-up Organisational Health activities.
3.12 The minute also notes that where deployment or internal recruitment has been made without appropriate clearance:
Getting the decision wrong can be very costly and impact on the AFP in many dimensions: reputation, costs to recover and remedy, Comcare premium, and negative employee confidence.37
3.13 The minute recommended that the governance arrangements for clearances be reinforced across AFP business areas, and that the mandatory requirement for medical and psychological clearances be met before postings, deployments, recruitments, training and secondments.
3.14 Non-compliance with the psychological clearance process reduces AFP business areas’ assurance that their employees can meet the psychological demands of certain specialist roles. Additionally, without conducting psychological assessments and undertaking adequate role preparation, the AFP may be exposing its employees to mental health risks38, impacting on the future health of its employees and may expose AFP to additional future Comcare claims.
Does the AFP have effective arrangements for preventing psychological injury, including through appropriate training?
The AFP has arrangements in place for preventing psychological injury but these are not fully effective as the AFP does not have a specific mental health training framework as a pre-emptive measure to improve employee resilience.
3.15 Psychological injury prevention involves understanding and minimising factors which heighten risk39, and enhancing factors40 which improve resistance.41 Psychological injury prevention can be undertaken through initiatives that target whole populations, such as all AFP employees, with the aim of promoting resilience in individuals or positively impacting on some aspect of the social environment. Alternatively, prevention can be undertaken through selective interventions that target people who have not yet acquired a psychological injury but who exhibit or are exposed to risk factors that may predispose them to injury in the future, such as AFP staff in specialist roles.42
3.16 The main universal prevention initiatives implemented by the AFP are the use of employment screening and psychological assessments discussed above. Such controls function to increase the likelihood that mentally fit employees are engaged by the organisation and perform specialist roles.
Mental health training
3.17 In addition to the employment screening arrangements outlined earlier, another key universal prevention activity is to undertake training to improve employee awareness and resilience. The 2016 NSW Government report Mental Health and Wellbeing Strategy for First Responder Organisations in NSW notes that:
Mental health and resilience training should begin from the first stages of emergency work training and should initially provide mental health awareness training, help-seeking advice and evidence-based resilience training. Mental health training and promotion strategies should then progress as first responders move into different stages of their career, including strategies on transitioning into retirement.43
3.18 The 2016 Victorian Police Mental Health Review made the following recommendation:
Mental health literacy content should also be embedded and examinable as a mandatory component in all leadership development programs, especially sergeant and senior sergeant levels, as well as training in undertaking supportive conversations. Attendance at a minimum number of such programs (e.g., at least one per year) could be included in Professional and Development Assessments for accountability purposes.44
3.19 The purpose of mental health literacy programs are to, among other things, increase recognition of early warning signs; provide accurate information about mental health issues including risk and recovery prospects; detail the benefits of and encourage early help seeking behaviour; provide information about evidence-based treatment options; and clarify appropriate ways to engage with and support a person in the workplace who may be experiencing mental health-related difficulties.45
3.20 Currently, the extent of mental health training focussed on enhancing the mental health of AFP employees is limited to:
- the Psychological Services team delivering a Wellbeing Services course to the AFP College as part of recruit training. This training involves informing cadets of the AFP support services available; and
- if requested by a business area, Psychological Services can provide training to support specific operational requirements or as part of preparation for overseas deployment. The training delivered by Psychological Services is operationally focused and delivered as skills training, however, AFP advises that the purpose of the training is to minimise the risk of psychological harm to AFP employees. A series of 31 courses were developed and delivered between 2010 and 2017 on an ad-hoc basis. The AFP was unable to advise how many individuals attended these courses. Examples of training provided under this heading include mindfulness, stress management, self-care, vicarious trauma, interacting with people who are suicidal, exposure to explicit material and respectful workplaces.
3.21 The AFP does not have a specific mental health training framework aimed as a pre-emptive measure to improve employee resilience. Further, there is no mandated mental health literacy content in AFP leadership programs. Whilst the draft AFP Mental Health Strategic Action Plan 2016–2022 indicates that mental health training is to be prioritised into learning and development activities covering induction to exiting the organisation, this document has yet to be formally approved, and there is no evidence that the articulated measures have been put into practice.
Recommendation no.3
3.22 The AFP implement a mandatory mental health training framework for all AFP employees, tailored to the various capability requirements throughout their career lifecycle that provides information on identifying signs and symptoms of mental health injury (in self and others) as well as guidance on how to conduct meaningful conversations with staff and colleagues about their mental health.
Australian Federal Police response: Agreed.
3.23 In late 2017, the AFP endorsed the delivery of a suite of mental health first aid training across the whole of the AFP. The delivery of this training, across the organisation, will be a tailored package to ensure the right training is delivered at the right time. The AFP agrees that a mental health training framework must be developed to afford access to diverse and relevant training for all areas.
3.24 We have also delivered an Early Access program where all members of the AFP can seek financial assistance for work related injuries both physical and psychological. This early intervention program is designed to link with the early recognition of mental health injury in self and others.
Does the AFP have effective arrangements in place for identifying psychological injury?
The AFP relies on three key mechanisms for identifying employees at risk of psychological injury: employee self-reporting; supervisor observation; and mental health assessments and psychological debriefs following deployment. There are limitations that reduce the effectiveness of these mechanisms, specifically:
- cultural barriers that reduce the likelihood of AFP employees self-reporting psychological injury;
- limited training and support for supervisors in identifying and supporting employees at risk of psychological injury; and
- inconsistent delivery and tracking of mandatory mental health assessments and psychological debriefs.
3.25 Whilst all AFP employees have a responsibility under the Work Health and Safety Act 2011 (WHS Act 2011) to report any negative psychological experiences to their Supervisor or Psychological Services, and to engage in actions to limit further harm, self-reporting is a mechanism of limited effectiveness. Interviews with AFP personnel noted that there are a number of barriers to self-reporting, such as the perception that firearms will be removed (resulting in reduced remunerative allowances and financial distress), or the perception of risk to career prospects. Results from the draft 2017 AFP Mental Health Review noted that the top three barriers to seeking support for mental health concerns were:
- putting one’s career at risk (32 per cent rated as a definite concern);
- fears that confidentiality will not be respected (31 per cent rated as a definite concern); and
- concerns that people will have less confidence in me (24 per cent rated as a definite concern).
3.26 In the AFP Strategic Leadership Group’s October 2016 meeting it was reported that stigma associated with mental illness, and a culture where employees with psychological injury have been referred to as ‘broken biscuits’, reduces the likelihood of employees seeking treatment.
3.27 The AFP’s other two mechanisms for identifying psychological injury are through:
- Supervisors—who may request a psychological assessment of an employee who they consider to be at risk. Supervisors are expected to continue to support the employee, however, as previously noted, supervisors do not receive any training on how to recognise or support employees at risk of psychological injury. In addition, as discussed in Figure 4.3, 76 per cent of AFP employees stated they were unlikely to seek support from their supervisor or manager; and
- Psychological Services—mental health professionals identify psychological injury through mandatory mental health assessments undertaken of employees in specialist roles (or who are exposed to explicit materials) and/or in the debriefing process following overseas deployments (discussed below).
Exposure to explicit material and mandatory mental health assessments
3.28 The AFP recognises that exposure to explicit material is a psychological health and safety workplace hazard. As such, under the WHS Act 2011, the AFP has an obligation to manage the potential psychological health impacts of exposure to such material. The 2017 AFP Handbook: Managing the Psychological Health Impact on Staff from Explicit Material46 (the Handbook) sets out the AFP policy and protocol for business areas to identify the risks and mitigation strategies for managing the potential psychological and health impacts from staff dealing with explicit material. The Handbook recognises however that the risks associated with exposure to explicit material cannot be fully mitigated.
3.29 The Handbook requires that employees working with explicit material should be cleared through a psychological assessment, including graduated exposure to materials, before undertaking their role. The key mechanism to manage an employee’s risk of psychological injury once they are in the role is to undertake mandatory mental health assessments. As per AFP policy, mental health assessments are to be conducted annually (at a minimum). For those staff who have been in the role for less than two years, mental health assessments are supposed to occur annually, and a mental health assessment screening test takes place at the six month point between annual mental health assessments. If there is a need for early intervention from these screening tests, the policy is for a follow-up discussion with an AFP psychologist. Mental health assessments are also mandatory on exit or re-entry into the role. Unlike psychological clearances and debriefs (discussed below), Psychological Services has a role in instigating and monitoring the occurrence of mandatory mental health assessments.
3.30 The purpose of the mental health assessment is to assess an employee’s psychological status. An AFP registered psychologist compares the employee’s incoming psychological testing results with previous results. The mental health assessment focuses on promoting employee self-awareness and includes a discussion on early intervention for signs of vulnerability and coping strategies.
3.31 When an employee leaves a role that involves working with explicit material, a mental health exit assessment must be conducted and involves:
- assisting ‘closure’ of any identified outstanding issues;
- providing information on potential transition experiences;
- assisting in linking the person to any ongoing support services, if required; and
- consulting on the next career role and any psychological considerations which have emerged as a result of working in the current area.
3.32 Where there are early indicators of potential delayed impact, employees are expected to undergo further assessment or intervention as recommended by Psychological Services.
3.33 The Handbook provides comprehensive protocols for managing the psychological risks of exposure to explicit materials, however the processes in the Handbook are not yet embedded into AFP practices.
3.34 ANAO analysis of PLANES database information for AFP employees currently working in Joint Anti-Child Exploitation Teams (JACET) showed that 26 of the 38 team members were in breach of the requirements47:
- 28 per cent (11 of 38) of the team’s employees had no mental health assessments recorded;
- of the 27 employees with a mental health assessment recorded, there was an average of 391 days since their most recent mental health assessment, and 55 per cent (15) were recorded as having had their most recent assessment over a year ago, with three employees not having had an assessment for over 600 days; and
- one employee had no record of a clearance48 or a mental health assessment against their name.
3.35 AFP reviewed hard copy files for the JACET employees’ mental health assessment records and advised that of the 11 employees with no mental health assessments recorded in the PLANES database, eight had had mental health assessments and three had mental health assessments scheduled.
3.36 Feedback from public submissions and interviews conducted with AFP personnel as part of this audit indicated that mental health assessments do not occur routinely, particularly in relation to exit assessments. Additionally, in March 2017 the AFP National Manager Forum Papers noted that:
AFP Digital Forensics specialists are often exposed to explicit material through their routine involvement in Child Protection Operations and Counter Terrorism operations. However, unlike investigators, as highly specialised technical specialists, employees do not have the same mobility across the organisation. As such, many long term Digital Forensics members have been exposed to explicit material for periods extending beyond 10 years. The removal of regionally based psychologists combined with the 30 per cent increase in operations over the past 12 months has reduced the resilience of members to deal with this exposure.49
3.37 The Handbook notes that while there is no evidence to support a fixed tenure of roles or the need to implement rotation policies, such policies may be more sustainable. The Handbook also recognises potential health risks associated with long-term exposure to explicit material. The ANAO suggests that the AFP monitor long-term exposure of its employees and implement workforce planning for specialist roles.
3.38 The draft 2017 AFP Mental Health Review results show that AFP employees working in ACT Policing have a higher rate of exposure to potentially traumatic events in their career than any other business area. ACT Policing has dedicated processes for dealing with critical incidents which involve the ACT Welfare Officers and team debriefs, however it does not have broader processes for monitoring the mental health of ACT Policing staff. The need for improved arrangements to support general duties police officers was also identified in the Queensland Audit Office’s audit of the Queensland Police Service (QPS):
… critical incident response processes are more likely to capture acute psychological health issues. They are less likely to identify more chronic issues that develop over time with exposure to multiple incidents and/or stressors. … Unlike for those officers in roles defined as specialist (high risk), the QPS has no established process for the ongoing psychological health monitoring of general duties and traffic officers. These officers are not offered or required to undertake periodic psychological health monitoring. The QPS is not proactively monitoring the biggest (and arguably highest-risk) component of its workforce. To our knowledge no Australian police jurisdiction has ongoing psychological health monitoring of general duties officers.50
3.39 The AFP faces similar challenges in regard to ACT Policing general duties officers, and should work closely with other policing jurisdictions to identify mechanisms for ongoing monitoring of the psychological health of general duties officers. In 2017, the AFP commenced an informal pilot process for identifying exposure of AFP employees to potentially traumatic events and has advised that work is being undertaken to review the Safe-T-Net system utilised by the Victorian Police Force.
Psychological debriefs
3.40 Following an individual’s completion of a long-term deployment or overseas mission Psychological Services is required to conduct a psychological debrief. It is the responsibility of the AFP business area or employee to request a debrief. The process requires completion of a Psychological Assessment Form51 and a face-to-face interview with an AFP registered psychologist. Debriefs are mandatory after a long-term deployment, but may also be requested as a result of a critical incident.
3.41 ANAO analysis of the PLANES database showed that in 2016–17 Psychological Services undertook 96 debriefs, a decrease on 2015–16, when 156 debriefs were undertaken. The AFP advised that this decrease is primarily due to the AFP’s changing international footprint and also relates to the surge of psychological clearances as part of Operation AREW, supporting the MH17 investigation in 2014.
3.42 The ANAO was unable to assess whether mandatory debriefings following a long-term deployment occurred in all cases, as it was not evident how the AFP monitors whether deployed staff attend a debrief. As debriefs can be instigated by the AFP business area or by the individual, and recorded by Psychological Services, there is need for role clarification on whose responsibility it is to ensure that mandatory debriefs occur and are recorded centrally.
3.43 Overseas deployments often involve personnel operating in volatile environments, and in response to a disaster or terrorist event. The AFP’s analysis of leave from Sept 2016 shows that employees in international operations have higher levels of unscheduled leave compared to other functions across the regions (ACT, NSW, QLD, Vic). The international operations risk assessment does not recognise mental health as a potential risk.
3.44 AFP personnel interviewed as part of this audit stated that mandatory debriefs did not occur routinely, particularly in relation to mission postings pre-2010 (such as for Sudan, Papua New Guinea, and the Bali bombings). Additionally there was feedback that debriefs were absent after more recent deployments, such as to the Netherlands for the MH17 investigation.
3.45 The purpose of the debrief processes is to assess whether AFP employees are at risk in their role as well as providing a baseline measurement for the ongoing monitoring of their psychological wellbeing. Data on debriefs, psychological clearances and other psychological related data needs to be more effectively collated and analysed by the AFP in order to monitor the psychological wellbeing of personnel involved in deployments.
Recommendation no.4
3.46 The AFP develop formal processes to monitor and provide assurance that:
- employees in specialist roles have their psychological clearance in place before commencing in the role; and
- mandatory mental health assessments and psychological debriefs are undertaken for all those who require them, in a timely manner.
Australian Federal Police response: Agreed.
3.47 The AFP recognises the under investment in systems and automation, and has committed to enhance and consolidate this through our transformation program. This program will implement a long-term workforce planning model including improved workforce health and wellbeing through implemented programs and processes.
3.48 The AFP is currently reviewing all employees who hold positions in high risk areas to ensure that appropriate screening and assessment has been undertaken. Work has also commenced to ensure that all associated employee records are up to date to reflect any screening, assessment and/or debriefing.
Does the AFP effectively support employees returning to work after a psychological injury?
There are weaknesses with the AFP’s rehabilitation and return to work arrangements for employees suffering from a psychological injury sustained during their employment with the AFP. In particular, the draft 2017 AFP Mental Health review identified the lack of mental health-specific rehabilitation policies and the absence of mental health training for rehabilitation case managers to allow them to inform, assess or guide appropriate return to work for staff with psychological injury. Improving return to work arrangements to support better outcomes for injured employees remains a challenge for all organisations.
Lodging a Comcare claim
3.49 Section 5A of the Safety, Rehabilitation and Compensation Act 1988 (SRC Act) defines a Compensable Injury as one that arose out of or in the course of an individual’s employment. When an AFP employee is injured or becomes ill in circumstances that appear to fall within that definition, they may choose to lodge a claim for compensation with Comcare. The Comcare claim process requires the employee to make a statement to Comcare, and the AFP is asked to respond to that statement.
3.50 ANAO analysis of the AFP’s Comcare data from Comcare’s Customer Information System (CIS) for the period 1989 to 2017 shows that psychological claims were three times more likely to be withdrawn during the assessment process than non-psychological claims made by AFP staff over the period, see Figure 3.1 for withdrawal rates for psychological injury claims.52 The higher withdrawal rates for psychological claims may reflect the anecdotal evidence from AFP personnel interviews and public submissions, as well as the draft 2017 AFP Mental Health review that indicate making a Comcare claim, when struggling with psychological injury, can exacerbate the injury and delay recovery. To address the higher withdrawal rates the AFP should investigate opportunities to better support employees during the Comcare claim assessment process.
Figure 3.1: Liability Status of Psychological Injury Claims

Source: ANAO analysis of AFP Comcare information.
Management of rehabilitation
3.51 The AFP has rehabilitation case managers who co-ordinate the activities necessary to assist the AFP in meeting its duties to manage the rehabilitation and safe and early return to work for any injured employee. When an employee is injured, AFP case managers initially contact the employee to explain workers’ compensation benefits and the return to work process, and provide them with the online claim forms and Comcare process guidelines. Throughout the process, case managers negotiate with senior managers, line managers, employees, rehabilitation providers, medical practitioners and Comcare claims managers in relation to assisting injured employees’ return to work.
3.52 Best practice53 considers that employers should arrange a rehabilitation assessment as soon as possible following the submission of a workers’ compensation claim. The information obtained from this assessment is then used to develop a rehabilitation program, which is a series of structured activities and services to assist the injured employee to achieve an appropriate rehabilitation goal. In most cases, the preferred rehabilitation outcome is to return an injured employee to their pre-injury duties as quickly and safely as possible. This can be put in place prior to Comcare determining the liability of the injury.
3.53 The AFP is proposing to establish an AFP Early Access (EA) program that will reimburse employees for the cost of any medical treatments associated with work related injuries both physical and psychological.54 The previous Early Intervention Program, in place since 2012, only covered physical injuries. The new EA program aims to reduce the impact of work-related injuries for members and the indirect costs for the AFP, such as loss of productivity. At the time of the audit, $100,000 had been allocated to the EA program for 2017–18.
AFP return to work outcomes
3.54 ANAO analysis of the AFP’s Comcare data for the period 1989 to 2017 is presented in Figure 3.2 and Figure 3.3. Figure 3.2 shows that in 15 per cent of cases, a psychological injury resulted in the employee returning to work with another employer rather than returning to the AFP. This differs significantly from the return patterns for physical injuries.
Figure 3.2: Total return to work outcomes of completed rehabilitation programs, 1989 to 2017

Source: ANAO analysis of AFP Comcare information.
3.55 Figure 3.3 shows that, of those employees with a psychological injury that return to work at the AFP, less than 40 per cent will return to the same duties they had pre injury/claim. This compares to other (physical) claims where the employee will return to the same duties in over 60 per cent of cases.
Figure 3.3: AFP return to work rehabilitation outcomes, 1989 to 2017

Source: ANAO analysis of AFP Comcare information.
3.56 More broadly, evidence from other policing organisations has found that employees have a proportionally lower rate of return to work for psychological injuries than for physical injuries. For example, the Queensland Audit Office Report Managing the Mental Health of Queensland Police Employees found that since 2009–10, the reported return to work rate for all injury types has averaged 90 per cent, while the rate for employees with psychological injury has averaged 70 per cent.55 Similarly, the independent report of the Royal Canadian Mounted Police – Mental Health Support for Members found that 20 per cent of members who sought support for a mental health condition did not return to work.56
3.57 The AFP Organisational Health Performance Report for the period 1 January to 30 June 2017 notes that mental stress claims represented:
- 24 per cent of claims over the period;
- 44 per cent of claim costs over the period; and
- 26 per cent of total weeks lost by mechanism of injury (body stressing injury is the only other claim type that represents a significant proportion of weeks lost at 37 per cent).
3.58 The draft 2017 AFP Mental Health Review identified weaknesses in the AFP’s rehabilitation and return to work arrangements. Specifically the review identified:
- the lack of mental health-specific rehabilitation policies and absence of mental health training for rehabilitation case managers to allow them to inform, assess or guide appropriate return to work for staff with a psychological injury;
- the absence of a system of preferred providers with known skills for treating mental health concerns arising from police work;
- unclear processes for ensuring access to rehabilitation services for injured workers deployed internationally, or those in regional and remote areas; and
- insufficient information about AFP operational requirements and risk assessment procedures given to external providers.
3.59 The draft 2017 AFP Mental Health review made a range of recommendations to improve the AFP’s rehabilitation and return to work processes for employees experiencing psychological injury.
3.60 With mental health claims costing on average two to three times more than other injury and physical disease claims, the AFP needs to actively monitor and support its members in achieving realistic return to work outcomes.
4. Mental health support services
Areas examined
This chapter examines the delivery of the AFP’s mental health support services for employees, along with the AFP’s arrangements to evaluate, monitor and report on employee mental health.
Conclusion
The AFP has a range of mental health support services available for employees to access. Recent employee feedback has indicated that the availability and effectiveness of these services is varied, and that there are no systemic arrangements to evaluate support service effectiveness on an ongoing basis. Feedback also indicated that cultural barriers to accessing support and assistance reduces the potential impact of these services.
Information on employee mental health is held across a range of disconnected information systems and multiple hardcopy records which make it difficult for the AFP to monitor and respond to emerging issues.
The AFP undertakes a range of internal reporting on mental health metrics and performance for internal oversight committees.
The external review currently being conducted of the AFP mental health support services, commenced in 2017, provides the AFP with the opportunity to inform the selection and resourcing of the most effective mix of support services to support the mental health needs of AFP employees.
Areas for improvement
The ANAO made two recommendations aimed at applying a risk-based approach to determine the optimal mix of services to target the identified organisational mental health risks, and developing an information system to track and monitor employees’ mental health over their career to support early intervention and support services.
Do the AFP’s services effectively support employee’s mental health?
The services offered by the AFP are not fully effective in supporting employee mental health. The AFP has seven support services available to employees that have mental health support elements, in addition to a range of related initiatives. Feedback from the draft 2017 AFP Mental Health Review and audit interviews with AFP personnel indicates that the availability and effectiveness of these services is varied. There are no systemic arrangements to evaluate the effectiveness of support services on a regular basis.
4.1 The AFP has a range of internal support services available for employees. Supporting staff mental health is a core function of AFP Psychological Services, the Employee Assistance Program, the Welfare Officer Network and the AFP Chaplaincy. AFP Safe Place and the Confidant Network are support services not specifically targeted at employee mental health but that may engage with staff on issues affecting mental health. Support services are outlined in Figure 4.1.
Figure 4.1: AFP’s internal support services
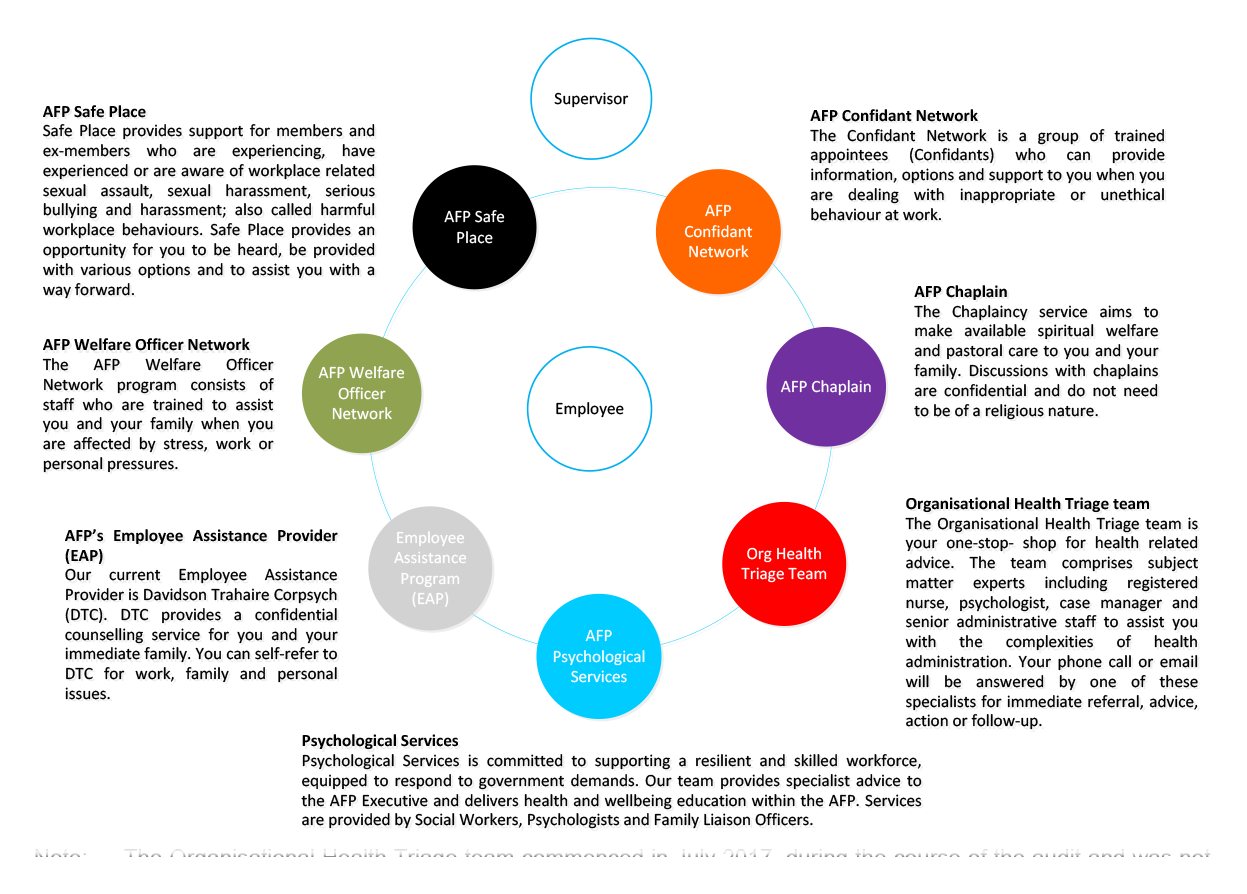
Note: The Organisational Health Triage team commenced in July 2017, during the course of the audit and was not examined.
Source: Reproduced based on AFP material ‘Our culture, Our AFP’. Professional Standards (PRS), AFP’s internal misconduct and corruption area, was included in AFP’s original material but is not included here. While noting that PRS has a responsibility to provide employees subject to an investigation with information on where to seek support in order to cope with the stress of the investigation, their role is not to provide mental health support.
4.2 The ANAO reviewed the AFP’s support services through an examination of documentation and data, information from 102 interviews with AFP personnel, 66 public submissions made to the audit and the results of the draft 2017 AFP Mental Health Review. A summary of the availability and access, reporting and usage and resourcing for each support service (based on 2016–17 data) is provided at Appendix 3.
Supervisors
4.3 AFP supervisors provide the day-to-day management interface for all AFP employees, and as such are the key first point for providing support to staff.
4.4 As noted previously in this report, AFP supervisors do not receive specific training in identifying or supporting employees that may be experiencing mental health concerns. The draft 2017 AFP Mental Health Review indicates that there is limited awareness by AFP supervisors of the AFP’s mental health support services, particularly in the regions (locations outside of the ACT), and limited awareness on how to appropriately support employees experiencing mental health challenges.
4.5 Currently, the AFP does not identify core supervisor competencies and training relevant to managing employee mental health, or incorporate this into supervisor training and selection/promotion frameworks. The 2017 expansion of the AFP Welfare Officer Network—discussed later in this Chapter—will better support supervisors across the AFP in managing employee mental health.
Organisational Health support services
Psychological Services
4.6 Psychological Services undertake a range of psychological functions in the AFP, including assessments and clearances of AFP employees, deployment debriefs, mandatory mental health assessments, and employee wellbeing training—these are outlined further in Chapter 3. In addition to those services, Psychological Services also provide:
- Services to management—development of policy and procedure and provision of advice;
- Services to individuals—through provision of education, short-term counselling, other interventions, and referrals to other services; and
- Services to families—through the Family Liaison Officer and management of the EAP counselling service.57
4.7 The ANAO’s analysis of the PLANES database shows that the total number of sessions delivered by psychological services (psychologists, social workers and the family liaison officer) to clients has decreased by 19 per cent over three financial years—from 4156 sessions in 2014–15 to 3370 in 2016–17. The AFP advised that factors affecting this decrease include a change in AFP’s international footprint, and a surge in clearance requirements relating to international incidents in 2014.
4.8 As at October 2017, there were six registered AFP psychologists and two social workers in the Psychological Services team, all of whom are based in the ACT. These staff undertake or oversight all mandatory health assessments, mandatory psychological clearances for specialist roles (pre-employment psychological clearances are outsourced), mandatory debriefs, and training for AFP staff nationally and internationally.
4.9 The ANAO also examined delivery of psychological services by AFP portfolio and geographic location. Analysis showed that the highest users of Psychological Services in the period June 2014 to June 2017 were employees working in International Operations, followed by non-AFP members (such as family members), and those in ACT Policing, Specialist Operations and Crime Operations. Geographically, ACT-based employees have been the highest consumers of Psychological Services, with 7098 services (55 per cent of all services) between 2014 and 2017.
Employee assistance program (EAP)
4.10 The EAP service is a mechanism for the AFP to provide support to staff and their families. The AFP EAP contract has been held by Davidson Trahaire Corpsych since 2000, and, along with the recently established Welfare Officer Network, is the only support service that produces regular reporting. EAP reporting is de-identified to protect employees, but provides the AFP with a summary of the key areas of concern for staff using the services. The ANAO reviewed the EAP service contract and the EAP monthly, quarterly and annual reporting covering January 2012 to March 2017 and identified the following:
- over five years there has been limited use of the EAP service in relation to critical incidents.58 Over this period the AFP engaged the EAP provider for 12 individuals (cases) in relation to critical incidents—three cases did not have any associated reporting and eight cases related to one incident. AFP employees used the EAP service in relation to work related trauma 40 times over the five years. Given the draft 2017 AFP Mental Health Review shows that 76 per cent of police officer staff, 43 per cent of protective service officers and 44 per cent of professional staff have indicated an exposure to critical incidents, it is apparent that AFP employees are either seeking support for critical incidents through other internal or external services, or are not seeking any support;
- 28 per cent of people using the EAP service are AFP family members. While the number of family members utilising the service is reported for billing purposes, the matters they discuss are not reported to the AFP;
- on average, employees are only using two out of the six sessions available per employee under the contract;
- psychological issues covering anger, anxiety, depression, grief and loss, personal stress, personal trauma, psychotic disorder and self-esteem issues represent 26 per cent of matters raised, with anxiety and personal stress representing the largest proportion of those issues;
- six AFP remote locations are serviced by telephone counselling, despite a contractual obligation for the service provider to provide face-to-face counselling for all AFP locations nationally. The EAP provider has advised that fly-in fly-out or drive-in drive-out services could be provided on request, however ANAO has not received evidence of these services being provided or offered;
- the service provider is unable to provide counselling within the contract timeframes. AFP personnel interviewed noted long delays in obtaining counselling appointments, particularly in the ACT where the majority of AFP employees are based. The EAP provider acknowledges they have not met the KPI turnaround times for the first two quarters of 2017, and advised that they are addressing the issue through recruitment; and
- limited evidence of contract management and quality assurance by the AFP in relation to the performance of the service provider. The contract requires that quarterly governance meetings occur between the parties, and that quarterly quality assurance reports are prepared by the EAP provider. There was limited evidence that these meetings occurred, or that the AFP monitors the quarterly assurance reports. The EAP provider advised that they undertake internal assurance processes over the quality of their service, however this information is not shared with AFP.
4.11 Additionally, submissions made through the ANAO’s citizen contribution function noted that there were significant concerns with the EAP service, including:
- qualified psychologists not always available through this service (social worker available instead);
- not being able to see the same counsellor on subsequent visits and having to explain the background each time; and
- inconsistent quality of counselling services.
4.12 The AFP is not effectively managing the EAP provider from a quality or contractual compliance perspective. The AFP advises that since June 2017, it has engaged regularly with its EAP provider to improve service delivery in areas such as: ensuring contract obligations are met; contract variations are discussed and agreed; an action plan is developed to address areas of concern; and new performance indicators agreed and implemented.
AFP Welfare Officer Network
4.13 ACT Policing has historically had two Welfare Officers supporting ACT Policing employees. From July 2017, the Welfare Officer Network was expanded nationwide. There are now eight welfare officers in Canberra plus three in ACT Policing, three in NSW, two in Victoria, one in WA, two in SA, one in Cairns, and two in Brisbane. Welfare Officers also have coverage of Darwin, Geraldton, Exmouth and all international posts. One Canberra-based Welfare Officer focuses on providing support to AFP family members.
4.14 A Welfare Officer’s primary role is to be a conduit to professional support, advice and counselling on an as required basis to AFP employees experiencing personal and/or work related issues. A further focus of the role is the provision of welfare support to employee’s families. Welfare Officer work may include:
- supporting AFP members as a result of a critical incident;
- supporting AFP personnel and their families who may be experiencing either personal or work related issues (including personnel with long term illnesses);
- preparing routine reports for management following incidents, and on workplace or workforce issues;
- engaging with and referring AFP members to professional clinicians, including elements of the Organisational Health portfolio or external service providers; and/or
- working in challenging conditions such as prolonged crime scenes, protracted siege situations and/or major events.
4.15 The Welfare Officer Network reports to the Organisational Health team based in ACT. The draft 2017 AFP Mental Health Review notes that the ACT Welfare Officers are considered to be a helpful and accessible support service in relation to other AFP support services. The National Welfare Officer Network was unable to be assessed as part of the audit since it was only recently established in July 2017.
AFP Chaplaincy
4.16 The AFP Chaplaincy is to provide multi-faith spiritual, pastoral care and welfare support to all AFP employees, retired members, and their immediate families.59 The AFP first appointed a full-time Chaplain in 1999. The AFP Chaplain is based in the ACT, with the majority of their time spent assisting ACT Policing staff. In October 2017, the AFP commenced using contractor Chaplains (on a fee-for-service basis) and Honorary AFP Chaplains in NSW, NT, QLD, VIC, WA and the ACT.
4.17 Policy on the operation of the AFP Chaplaincy was developed in July 2015, and revised in June 2017 (during the course of the audit). The 2017 policy notes that:
Spiritual wellbeing is an essential component to sustaining the health of AFP members, and crucial in assisting the AFP to work as a successful and safe workplace. The AFP values the commitment that appointees make to the field of policing, and is aware of the impact that this can have on appointees’ work and personal lives. Consequently, the AFP has a responsibility to support and protect the wellbeing of its appointees.60
4.18 The Chaplaincy does not maintain performance information. It is not clear how frequently AFP members access the Chaplaincy service, reporting is ad hoc, and no evaluation of the Chaplaincy service has been undertaken. The lack of reporting and performance information on the Chaplaincy program provides no assurance that the program met, or was compliant, with the 2015 policy. AFP advised that reporting mechanisms have been in the process of being tested since October 2017.
4.19 AFP employees interviewed expressed mixed views regarding the benefit of having a dedicated AFP Chaplaincy service. Outside of the ACT, AFP employees reported not having had access to a Chaplain, and therefore gained limited benefit from the service. In the ACT, many staff expressed positive views of the Chaplaincy, although noting the limited support available other than a ‘friendly conversation’.
Other Organisational Health initiatives
Equipt app
4.20 In October 2017, the AFP made available a free wellbeing app Equipt for current and former AFP employees and their families. The AFP, in partnership with the Australian Federal Police Association, have licenced the app from Victoria Police and The Police Association of Victoria and tailored aspects to meet AFP needs. The app is a self-help tool to assist individuals with tracking their physical, emotional and social wellbeing.61
Early access program
4.21 As outlined in 3.53, the AFP established an Early Intervention Program in July 2012 that provided reimbursement of medical treatment to employees for work-related physical injuries separate to a Comcare claim. This allows support and rehabilitation to be commenced as soon as possible. In September 2017, the AFP allocated funding to expand this program to also include psychological support to employees, renamed Early Access (EA). The EA program aims to reduce the impact of work-related injuries for all employees and the associated indirect costs for the AFP, such as loss of productivity.
Other support services
AFP Safe Place
4.22 A key recommendation from the 2016 AFP Cultural Change: Gender Diversity and Inclusion in the Australian Federal Police review, was the establishment of an independent unit to support complainants and to investigate sexual harassment and abuse. While not specifically targeted at mental health, AFP Safe Place was established to fulfil a culture change and gender equity function by supporting current and former AFP employees who have experienced harmful workplace behaviour such as sexual harassment, assault and bullying. These issues can affect mental health. Since its establishment in August 2016, Safe Place has received approximately 318 referrals.
AFP Confidant Network
4.23 The Confidant Network has been in place since 1996 and was setup to provide AFP employees with an informal network of Confidants—experienced AFP employees—who could provide advice and support when personnel are experiencing difficulties in the workplace, or have workplace integrity concerns. As at 30 August 2017, the AFP had 109 Confidants across 15 locations in Australia and overseas.
4.24 Historically, any AFP employees can volunteer to be a Confidant, in addition to their normal roles, with the criteria for selection of Confidants appearing ad-hoc.
4.25 The Confidant Network sits under the Reform, Culture and Standards Area and an annual report is produced on the data generated by the Confidants. For the Confidant Network to operate successfully, information relating to individuals must be kept confidential, and therefore reporting only encompasses the referrals made to Confidants by incident type.
4.26 The AFP reviewed the Confidant Network in 2016 and made 23 recommendations aimed at improving the operation of the Network, including developing a communications strategy, updating governance documentation, improved consultation and collaboration with relevant areas of the AFP, improving the selection process and regular monitoring of program performance. AFP reporting indicates that of the 23 recommendations, 13 are complete and nine are in progress or ongoing, as at November 2017.
4.27 The review found that a major indicator of the effectiveness of the Confidant Network is the level of trust AFP employees have in the personnel comprising the Network. AFP personnel interviewed as part of the audit indicated concerns with the current operation of the Confidant Network, particularly in relation to confidentiality. This particular concern could act as a barrier to AFP employees seeking support from the network.
4.28 The Confidant Network’s efforts could be more effectively aligned with the other support networks and services offered by the AFP. For example, whilst Confidant Network reporting is limited, there may be benefit in matching Confidant Network information with Safe Place data, EAP reporting and Welfare Officer Network reporting to identify trends in mental health concerns across the AFP.
Support for former AFP employees
4.29 Under the Safety Rehabilitation and Compensation Act 1988, the AFP remains liable for any existing Comcare claims and new claims that may be lodged by an individual after cessation with the AFP in relation to injuries which occurred during employment.
4.30 The Heads Up and Beyond Blue Good Practice Framework notes that:
First responders leaving the service – either for a career change or for retirement – face specific challenges. The loss of self-identity tied to their first responder life can be very difficult. Depending on their reason for leaving there may also be a host of other stressors impacting on their mental health. Unfortunately, there is often little support available to first responders at this point of their career.62
4.31 The only AFP support services available to former AFP employees are Safe Place and the Chaplain—as discussed above. The AFP advised that former employees are also supported by the Organisational Health Triage Team established in July 2017.
4.32 The ANAO analysed the AFP’s Comcare data for the number of claims lodged by former AFP employees (whether through resignation or dismissal). As Figure 4.2 shows, psychological claims are more likely to be lodged by former employees than physical or other claims. While the volume of claims from 2000 to 2015 remained consistent, there has been a significant increase since 2015, with post-employment psychological claims accounting for around eight per cent of all claims in 2016–17.
Figure 4.2: AFP Comcare claims by former AFP employees (as a percentage of total)

Note: The figure represents psychological Comcare claims lodged after the employee has left AFP as a percentage of total psychological claims made in the relevant year. Similarly, it shows physical claims lodged after the employee has left AFP as a percent of total physical claims made in that year.
Source: ANAO analysis of AFP Comcare information.
4.33 The data in Figure 4.2 indicates that the AFP could investigate opportunities to improve employee exit/departure processes, such as providing advice and information on available services that can be accessed, including a mental health assessment or checklist into employee exit/departure processes, or developing transition plans for employees accessing AFP support services prior to departure.63
Are mental health services regularly evaluated to assess effectiveness?
The AFP does not have a framework in place to evaluate the effectiveness of mental health support services and management arrangements. In 2017 the AFP commenced an external review of mental health support services for employees. The review is examining the AFP support services. In 2017, AFP also undertook an internal review of the Confidant Network.
In developing the strategy for managing AFP employees’ health and wellbeing, the AFP should incorporate regular reviews of the effectiveness of the mental health support services, as well as evaluating the appropriateness of the overall mix of services in terms of coverage, use by employees and value for money.
Evaluation of mental health support services
4.34 The AFP does not have systematic evaluation arrangements in place to assess the effectiveness of mental health support services, and to evaluate whether the AFP has in place the optimal services to target areas of highest risk.
4.35 In 2017, the AFP commissioned a review of its mental health support services, which was conducted by external mental health specialists and included focus groups and a survey seeking employee views of internal and external support services. The results in relation to AFP employee preferences on seeking support from each of the AFP support services are shown in Figure 4.3 and Figure 4.4.
Figure 4.3: AFP services/support: Employee support seeking preferences of respondents with high stress indicator

Note: The survey did not include a high level question on the Welfare Officer Network.
Source: Draft 2017 AFP Mental Health Review.
4.36 The survey found that for the subset of AFP employees who were experiencing high distress at the time of the survey, only 12 per cent were likely, and 76 per cent were unlikely, to seek support from AFP support services on average across the six64 listed services. Similarly, for employees experiencing high distress at the time of the survey, 56 per cent indicated they were likely, compared to 28 per cent unlikely, to seek support from external supports such as family or friends, a private GP or a private psychologist — as shown in Figure 4.4. The survey also shows that employees were more likely to seek support from Google or online tools before any of the AFP support services, as shown in Figures 4.3 and 4.4.
Figure 4.4: External services/support: Employee support seeking preferences of respondents with high stress indicator
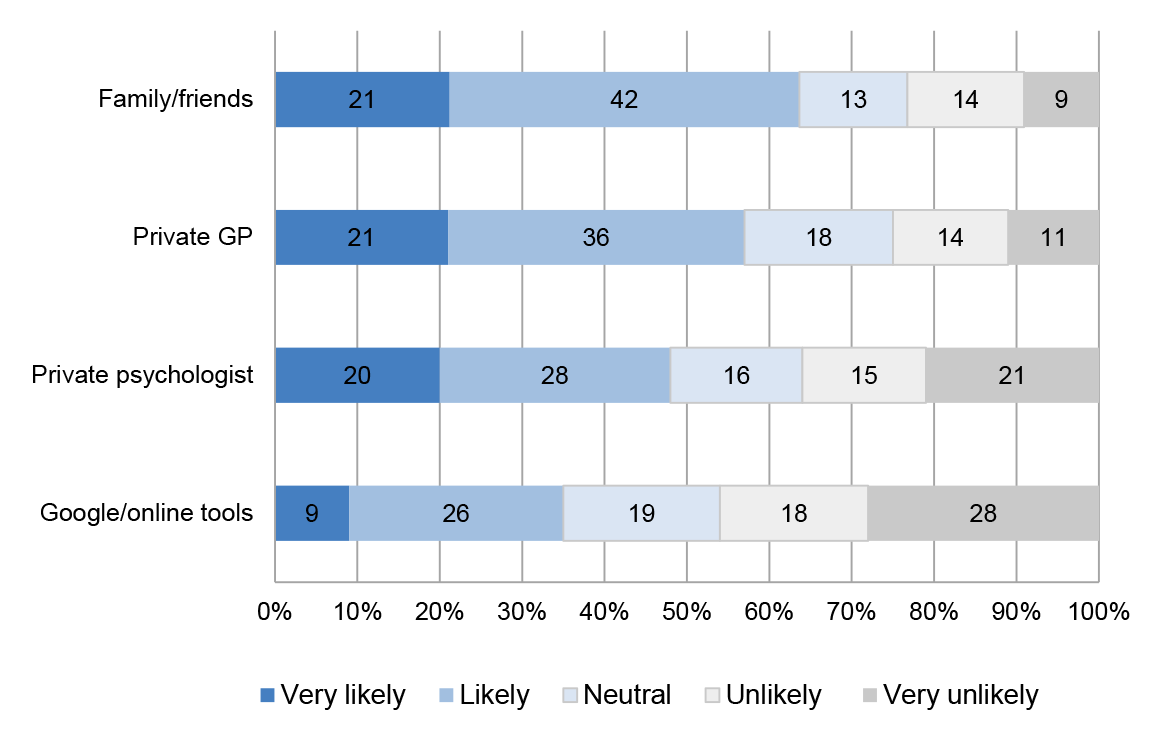
Source: Draft 2017 AFP Mental Health Review.
4.37 While the draft 2017 AFP Mental Health Review indicated that AFP employees were more likely to seek support from external services than internal AFP services, the ANAO found that external sources were not clearly and consistently promoted by the AFP as options for employees. AFP personnel interviewed for this audit also indicated that they sought support through external information and advice (such as family and friends, online research or their GP).
4.38 The draft 2017 AFP Mental Health Review identified that there are a range of barriers that limit AFP employee willingness to seek support within the AFP, including organisational culture, the stigma associated with mental illness, perceived impact on career, confidentiality and the extensive Comcare claim process.
4.39 More regular, systemic evaluations such as the survey can assist the AFP to better determine the optimal mix of mental health support services to provide to employees, and inform new AFP initiatives such as the Early Access program.
Recommendation no.5
4.40 The AFP, in reviewing available support service options, uses a risk-based approach to determine the optimal mix of services to target identified organisational mental health risks, including:
- linking the outcomes of that review with the development of an organisational health and wellbeing strategy;
- ensuring the health and wellbeing strategy also addresses the cultural change required to support and encourage employees to access mental health services when required, particularly after involvement in critical incidents or prolonged exposure to high-stress roles; and
- establishing performance measures for the selected support services, and implementing monitoring and evaluation arrangements to ensure those services are systematically assessed.
Australian Federal Police response: Agreed.
4.41 The Phoenix Australia work seeks to undertake a structural review and reform process, and policy development on mental health of the AFP. In addition to mental health specific recommendations, the review is holistic incorporating leadership and training frameworks, culture and services.
4.42 The Phoenix review benchmarked the AFP against each element of the best practice framework for managing mental health in high-risk organisations. It identified that although there were shortcomings in the current support service, each component of the service was an important component of a comprehensive approach.
4.43 Using evidence based information to inform future investment is a key priority. Within the AFP, we are building our capability in data analytics to ensure that we align our proposed policies, practices and programs with areas and individuals of greatest need. By drawing on multiple inputs, the AFP will be positioned to have greater visibility of potential risk areas that may require additional support and to assist us in evaluating the effectiveness of the various service offerings.
Is information collected and used to monitor employee mental health?
The AFP’s information on employee mental health is held across a range of disconnected information systems and multiple hardcopy records which make it difficult for the AFP to monitor and respond to emerging issues in employee mental health.
The AFP holds data in areas such as workplace health and safety incident reporting, Comcare claims, unscheduled leave, exposure to critical incidents and explicit material and information on deceased personnel which, if linked and analysed appropriately, could assist in identifying known psychological injury risk factors. There is an opportunity for the AFP to conduct such analysis and inform more targeted monitoring and support services.
Collection of AFP mental health information
4.44 The systems and locations which hold AFP employee mental health information are outlined in Figure 4.5.
Figure 4.5: Sources of AFP employee mental health information

Source: ANAO analysis of AFP data.
4.45 The AFP Organisational Health function has six bespoke Microsoft Access databases to hold relevant information on AFP employees. These databases were designed and developed in-house by AFP staff to assist in managing information that had previously been held in hardcopy files. The databases are not supported by AFP ICT, have functionality limitations and do not integrate with the AFP’s corporate records management system. Records held on the databases only date back to the creation of each database and in 2017, the AFP contracted in maintenance support on a part-time, as needs basis, for the databases in the absence of ICT support.
4.46 In addition to these six databases, each AFP employee may have up to three separate hardcopy files held by the Organisational Health function for their Psychological, Medical and Work Health and Safety records. Internal AFP psychologists and social workers also maintain their own case file notes for employees that they see on an ongoing basis as clients. These case notes are not filed in a consistent manner and may be located on the AFP’s H-drive, attached to individual AFP employees’ psychological hard copy file or added to the PLANES access database. There can be significant delays before an individual’s psychological case note is placed in the appropriate hard copy file.
4.47 The AFP has recognised the risks associated with maintaining multiple hardcopy files and databases for employee health information. The Project Initiation Document for ‘Project Calypso: One AFP Member, One AFP Health File’, dated November 2014, states that:
This approach [of multiple employee health files] is inefficient and cumbersome and does not allow [Organisational Health] to provide the organisation with real time information on a range of health issues germane to business as usual processes, or the efficient processing of clearances for operational readiness and member deployment.
4.48 In the AFP’s most recent entity level risk profile, the three most significant risks faced by the organisation are all technology-related (all are rated critical). The three identified risks are: ‘we don’t have the right technological capability; we don’t sustain our information and communication systems and we don’t adequately manage or protect information’. As the AFP works to address these identified technology risks, it should consider opportunities to improve the management of employee health and wellbeing information.
4.49 In June 2017 Project Calypso was combined with an additional capital proposal for a Workers’ Compensation Management and Processing Solution (an end-to-end automated, integrated case management system for AFP workers’ compensation and rehabilitation). This proposal is subject to ongoing consideration by the AFP in relation to investment.
Monitoring and analysis of employee mental health data
4.50 The information which the AFP holds relating to employee mental health, if used appropriately, could assist in providing targeted and early intervention support services.
Work health and safety incident data
4.51 Under the Work Health and Safety Act 2011, the AFP is required to keep a record of all work related incidents and hazards, which are reported through completion of a Workplace Incident or Hazard Report form in the AFP’s human resources information system (HRIS).65 Workplace incidents reported to the AFP include both physical and psychological injuries. If a workplace incident is categorised as a ‘notifiable incident’66, the AFP’s system automatically notifies Comcare. Individuals who report psychological incidents to the AFP may also decide to report the incident to Comcare directly as a psychological claim.
4.52 Data from the Workplace Incident and Hazard Reports is exported to an Access database (‘WHSR Reporting’) along with other HR data such as employee identification numbers used in Organisational Health for analysis and reporting. Reports on this data are regularly provided to the Executive Leadership Committee, the National Safety Committee and the Regional Safety Committees.
4.53 The AFP does not currently bring together its incident data and Comcare claim data to assist in analysing those psychological incidents that result in a Comcare claim versus those that do not. Bringing together the incident and Comcare claim data would also assist in quality assuring the data as some employees may submit a claim directly to Comcare rather than lodging an incident report form with the AFP first. The AFP advised that since 2013 AFP case managers have been required to manually ensure that there is a matching AFP incident number for every Comcare claim.
Comcare data
4.54 The AFP has access to employee Comcare claim data through the Comcare Client Information System. As discussed in Chapter 1, both the volume and cost of AFP Comcare claims for psychological injury have increased from $2.8 million (and 11 claims) in 2007–08 to $16.7 million (and 35 claims) in 2016–17.67 In contrast, the volume and cost of AFP Comcare claims for physical injury have decreased over the same period.
4.55 The AFP regularly analyses Comcare claims data, including for psychological claims. For example, it examines changes over time in the number and cost of psychological Comcare claims, as well as weeks lost to injury. The AFP also tracks changes over time in its Comcare premium rate as well as the average cost of its return to work program and duration by injury category. The AFP’s analysis of changes to its Comcare premium rate has prompted organisational changes, for example, the inclusion of mental health as an enterprise risk for the first time in 2016—as discussed in Chapter 2.
4.56 There is the opportunity for the AFP to undertake further analysis of Comcare data in relation to the nature of psychological injury claims. As highlighted in Figure 4.6, Comcare data provides detail on the nature of claims, which could be used to inform the AFP’s mental health management and support arrangements provided to employees.
Figure 4.6: Number of accepted AFP Comcare claims, by nature of psychological injury
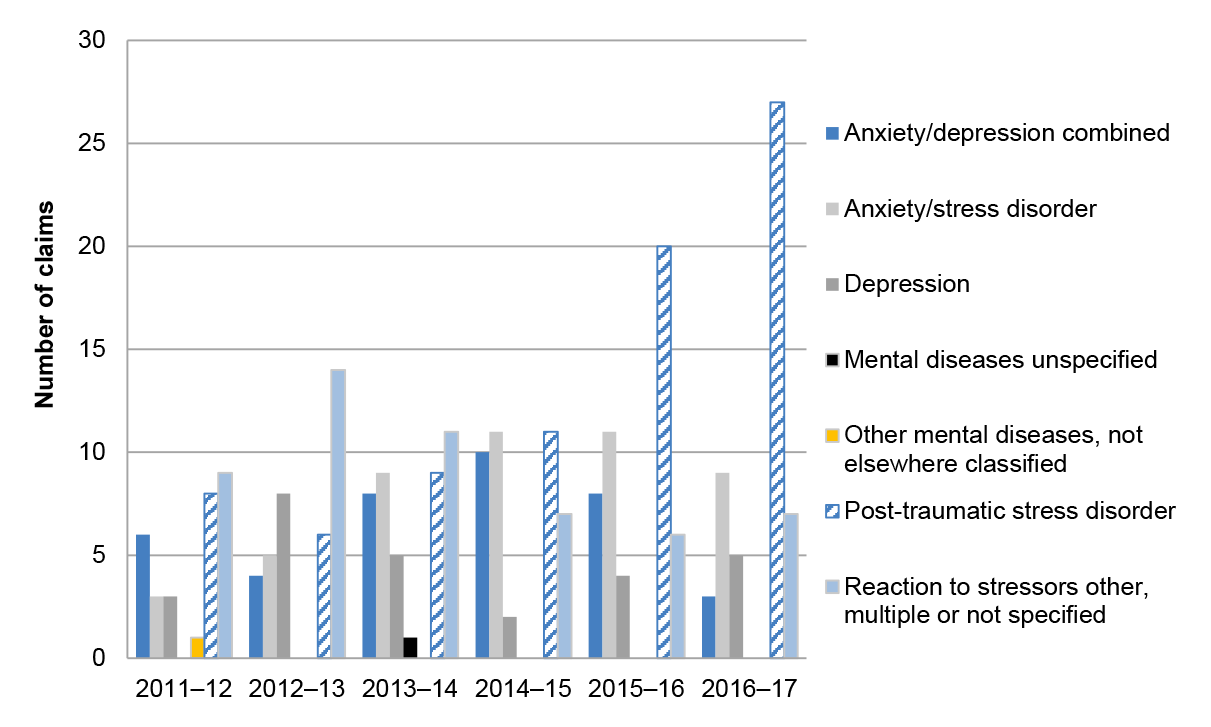
Note: Two categories of nature of psychological injury have had very few accepted claims against them since 2012 (mental diseases unspecified: 1 in 2014; other mental diseases, not elsewhere classified: 1 in 2012.)
Source: ANAO analysis of AFP Comcare information.
4.57 There would also be benefit in the AFP considering opportunities for geographically-based analysis of psychological Comcare claims (and psychological incidents), in addition to its current function-based analysis. Comcare data currently focuses on AFP functional areas (eg Crime Operations or Counter Terrorism, which are not specific to physical locations) rather than AFP locations. Geographically-based analysis would assist the AFP in ensuring that sufficient mental health management and support is being provided to regional and international locations and to identify emerging issues in particular regions or locations.
Unscheduled leave data
4.58 The AFP’s HRIS holds information on employee leave records, including unscheduled leave. Recognising that unscheduled leave can be an indicator of wider organisational issues, the AFP analyses and reports on this data. The AFP’s Strategic Leadership Group receives a quarterly report on unscheduled absences by sworn status, age and service groups, as well as function and state. The report identifies the functional areas of the AFP where unscheduled leave rates are higher than expected.
4.59 The AFP does not routinely connect its unscheduled leave data to its information holdings on psychological Comcare claims or psychological incident data. There would be benefit in the AFP undertaking such analysis to identify any correlations between higher rates of unscheduled leave and occurrence of psychological injuries.
Deceased personnel data
4.60 The AFP HRIS also holds data on the reason that individuals are no longer with the organisation, specifically whether they retired, resigned or are deceased. In relation to the deceased category, the system does not record any details in relation to the cause of death. There would be benefit in the AFP recording cause of death to enable analysis of contributing factors so that, if relevant, the AFP can adjust mental health management and support arrangements to better address identified factors.
Data on critical incidents and exposure to explicit material
4.61 As outlined in paragraph 1.24, within AFP there is an informal pilot project to link disparate data sources to track employee exposure to critical or potentially traumatic incidents.68 Combining data from its policing case management system with time charging records illustrated how many hours AFP members are charging to particular types of cases, and attendance at critical incidents. Such information can improve the targeting and timeliness of intervention support to employees who may be at risk from cumulative exposure to traumatic events and/or material.
4.62 The AFP’s Handbook on Explicit Material recommends limiting staff exposure to explicit material to four hours per day to allow time for rest and recovery. As the time allocation system for AFP employees does not differentiate between time spent exposed to explicit material and time spent on other work related to child sex offence cases, the AFP Executive cannot use time reporting to gain assurance that their controls on exposure to explicit material are being met.
4.63 The AFP’s activities to monitor employee exposure to critical incidents and traumatic material is in its early stages, and a project plan or budget has not been developed to further this initiative. The AFP has advised that work to improve data collection, tracking and presentation is ongoing, and that it will work closely with employees in relevant business areas as well as with other policing organisations to ensure that the system put in place is appropriate. There are benefits in better understanding the traumatic exposures of AFP employees in order to provide early intervention support in a timely manner.
Recommendation no.6
4.64 The AFP:
- consolidate disparate systems and hard copy records in order to establish an electronic health records management system that allows a single point of access to high level health information for each AFP employee; and
- establish a strategy for analysing employee health information against data in areas such as workplace incident reporting, Comcare claims, unscheduled leave, exposure to explicit material and information on deceased personnel in order to assist in identifying and addressing known psychological injury risk factors.
Australian Federal Police response: Agreed.
4.65 The AFP recognises a decline in investment of information technology systems over the years and has committed to enhance and consolidate these systems through the transformation program. Work has already commenced on an ICT roadmap and aligning ICT initiatives with the AFP’s transformation requirements. This includes investment in innovative early intervention strategies to manage workplace health proactively, including the automation of processes and procedures within the Organisational Health Branch.
4.66 Our commitment to change is further demonstrated by the establishment of the AFP’s Enterprise Transformation Office (ETO), dedicated to implement recommendations outlined in the 2016 Functional and Efficiency Review (FER) and to guide organisational change. As an organisation, we acknowledge that the AFP needs to change in order to meet the growing demand and complexity of the environment in which the AFP operates. Even within current staffing levels, the AFP is working under immense pressure and ongoing activity at current operational tempo will increase health risks for its staff. The transformation program seeks to address this.
4.67 We have invested significant resourcing over many years in employee health however know we have some way to go on this journey. I [AFP Commissioner] thank the Australian National Audit Office for prioritising the mental health of AFP employees in producing this report. The senior leadership group and I are committed to prioritising and protecting the mental health of all our employees.
Appendices
Appendix 1 Entity responses







Appendix 2 AFP committees which address elements of employee mental health

Note: Chief Operational Officer (COO); Deputy Commissioners (DCs); Chief of Staff (CoS) Deputy Chief Police Officer (DCPO); ACT Chief Police Officer (ACPO), National Manager (NM); Australian Federal Police Association (AFPA), Chief Medical Officer (CMO).
* During the course of the audit, the reporting arrangement was to the Minister for Justice.
Source: ANAO analysis of AFP documentation.
Appendix 3 ANAO summary of AFP mental health support services 2016–17
|
Service description |
Availability and access |
Reporting and/or usagea |
FTE and Annual Cost |
|
Supervisors |
All AFP locations |
n/a |
1971 FTE |
|
AFP Confidant Network |
109 Confidants in 15 national and international AFP locations. Confidants not available in seven AFP national locations. |
2.76% of AFP personnel utilised the Confidant Network in 2016–17. (data provided until 24 May 2017) |
$383 199 (2.35 FTE). There is no specific funding or allowance provided—employees perform Confidant role on a voluntary basis. |
|
AFP Chaplain |
AFP Senior Chaplain based in the ACT, with a majority focus on serving ACT Policing. One contract Chaplain available in ACT. Honorary AFP Chaplains available in NSW, NT, QLD, VIC, WA and ACT. |
No data is maintained on the usage of the Chaplaincy service. |
$226 412 (1 FTE). |
|
Organisational Health Triage team |
Located in the ACT, but available to all staff via email or phone. |
n/a – initiative commenced in July 2017 (during the course of the audit) and therefore was not examined. |
|
|
Psychological Services |
Located in the ACT, but available to all staff via email or phone. Some face to face services available to regions on a ‘fly-in / fly-out’ basis. |
Conducted 3370 sessions across 2493 individual employees in 2016–17. |
$1 384 643 (8.2 FTE). |
|
Employee Assistance Program (EAP) |
Nine AFP national locations serviced face-to-face. All AFP locations serviced by telephone. |
5.22% of AFP personnel utilised the EAP in 2015–16. |
$159 000 Outsourced service, which provides mix of counsellors and psychologists. |
|
AFP Welfare Officer Network |
Two Welfare Officers - Historically only available for ACT Policing. Ten additional Welfare Officers introduced in 2017, which are across AFP locations (ACT, NSW, Vic, WA, SA). |
There is no formal reporting or performance arrangements for the ACT Welfare Officers. The National Welfare Officer Network does not have performance data as it commenced in 2017. |
$304 822 in 2016–17 (ACT Welfare Officers, 2 FTE). $38 103 (National Welfare Officer Network – expenses only, does not include salaries). |
|
AFP Safe Place |
ACT based, available to all staff via email or phone |
4.87% of AFP personnel utilised the Safe Place service (In the period since establishment on 22 August 2016 through to 30 June 2017. |
$989 633 (4.94 FTE). |
|
Total actual cost of support services in 2016–17 |
$3 486 095 |
||
Note a: Service usage is measured as the number of staff using the service as a percentage of overall AFP staffing levels in 2016–17.
Source: ANAO analysis of AFP information.
Footnotes
1 Sworn staff consist of police officers and protective service officers (PSOs). Both groups hold specific powers under the Australian Federal Police Act 1979. PSOs provide an armed, uniformed protective security layer to detect, deter and respond to criminal and national security incidents at Australian government critical infrastructure and sites and interests in Australia and overseas. Professional staff work in operational roles such as forensic crime scene investigators, as well as support and corporate positions.
2 World Health Organisation, Mental Health Action Plan 2013–2020 [Internet], WHO, Switzerland, p. 6, paragraph 6, available from <http://apps.who.int/iris/bitstream/10665/89966/1/9789241506021_eng.pdf?ua=1>, [accessed 23/8/2017].
3 Department of Health, What is mental illness? [Internet], available from <http://www.health.gov.au/internet/publications/publishing.nsf/Content/mental-pubs-w-whatmen-toc~mental-pubs-w-whatmen-what>, [accessed 21/8/2017].
4 The Australian Government’s Work Health and Safety insurer, regulator and scheme manager.
5 Comcare, Psychological injury claims – with a date of injury on or after 13 April 2007, last updated 26 November 2015 <https://www.comcare.gov.au/claims_and_benefits/case_managers/psychological_injury _claims_how_comcare_determines_initial_liability/pychological_injury_claims_-_with_a_date_of_injury_on_or_after_13_april_2007> [accessed 26/10/2017].
6 Raphael, et al. World Health Organisation, Promoting Mental Health: Chapter 11: Links between mental and physical health and illness, 2005, pp. 132–147.
7 Studies include: 1.Victoria Police, Victoria Police Mental Health Review: An Independent Review into the Mental Health and Wellbeing of Victoria Police Employees; 2. P Cotton and PM Hart, ‘Occupational Wellbeing and Performance: A Review of Organisational Health Research’, Australian Psychologist, Vol 38 (2), 2003, pp. 118-127; and 3. Queensland Audit Office, Report 2: 2017–18 Managing the mental health of Queensland Police employees, Queensland Audit Office.
8 Victoria Police, Victoria Police Mental Health Review: An Independent Review into the Mental Health and Wellbeing of Victoria Police Employees, pp. 22-23.
9 Queensland Audit Office, Managing the Mental Health of Queensland Police Employees: Report 2 2017–18, October 2017, p. 15.
10 Australian Federal Police, Australian Federal Police Draft Mental Health Review: Appendix 2 Survey, 11 October 2017, p. 12; A McMillen, ‘Brisbane’s Story Bridge: a tale of tragedy for far too long,’ The Australian, 5 September 2015; M Palin, AFP agents’ harrowing stories: ‘My life has never been the same’, news.com.au, 17 February 2017, available from <http://www.news.com.au/national/afp-agents-harrowing-stories-my-life-has-never-been-the-same/news-story/b6e6326963affff801338caf13538d22> [accessed 17 February 2017].
11 The AFP has positioned staff across Australia and a number of locations overseas. AFP staff are deployed overseas to work with international partners on short and long term engagements, or in response to incidents such as aircraft accidents or terror motivated bombings involving Australians.
12 Victoria Police, Victoria Police Mental Health Review: An Independent Review into the Mental Health and Wellbeing of Victoria Police Employees, 2016, p. 14.
13 Australian Government, Comcare, Safety, Rehabilitation and Compensation Commission Annual Reports 2016–17, p. 2.
14 Costs reflect both the cost-to-date as well as Comcare’s estimated future costs.
15 Commonwealth, Additional Estimates, Legislative and Constitutional Affairs Committee, 28 February 2017, A Colvin, Australian Federal Police Commissioner.
16 The AFP had initial discussions with the contractor from November 2016, with the formal contract being signed on 22 March 2017.
17 The ANAO’s report uses information from the contractors’ aggregated survey report only.
18 Australian Federal Police, Mental Health Strategy Board Terms of Reference, February 2017.
19 The Equipt app is confidential and the information entered into it by a user can only be accessed by that user.
20 Queensland Audit Office, Managing the Mental Health of Queensland Police Employees: Report 2 2017–18, October 2017; Auditor General of Canada to the Parliament of Canada, Independent Audit Report 4 – Mental Health Support for Members – Royal Canadian Mounted Police, Spring 2017; Audit Office of New South Wales, Preventing and Managing Worker Injuries, 13 October 2016.
21 The ANAO’s report uses information from the contractors’ aggregated survey report only.
22 Australian Federal Police, National Safety Committee Terms of Reference, May 2017.
23 The four Enterprise Risk Profile risk categories are: people, health, culture and safety; operational outcomes; resourcing, workforce planning and management; and support capability.
24 Risk 1.3: mental health injury to AFP personnel.
25 Controls are risk reduction measures currently in place, while treatments are planned risk reduction measures that have not yet been implemented.
26 Australian Federal Police, Risk Assessment and Treatment Plan: Organised Crime and Cyber, August 2017.
27 Australian Federal Police, Risk Assessment and Treatment Plan: ACT Policing, August 2017.
28 Australian Government, Australian Federal Police Act 1979, sections 24, 40C and 40EB.
29 Psychological clearances are required due to the work involved in certain specialist roles such as those requiring exposure to explicit material in child protection operations, forensics, counter terrorism or roles in the Specialist Response Group and International Operations. These roles also require regular mental health assessments discussed at paragraph 3.29.
30 The Clearance database holds information on AFP clearances. The PLANES database holds information on AFP employee use of psychological services and consultations. The Comcare CIS database holds information on active and inactive Comcare claims. If an employee has an existing stress-related Comcare claim the employee will not be approved. The range of information systems that hold information on AFP employee mental health are outlined and discussed in greater detail in Chapter 4: Mental health support services.
31 The Psychological Services Assessment Form covers general employment information, health history (including mental health conditions), strategies for stress and life challenges, relationships and support available. It also includes: an AUDIT-C questionnaire designed to identify hazardous alcohol usage; a DASS21 questionnaire designed to measure the negative emotional states of depression, anxiety and stress; and a PCL-5 questionnaire to screen for PTSD symptoms.
32 This interview may be conducted face-to-face or over the phone by an AFP registered psychologist.
33 Psychological assessments for child protection roles include an online pyschEval Personality Questionnaire (PEPQ) designed to assess factors related to mental health pathology (for example emotional stability, anxious depression, apprehension, low energy). The online test is outsourced on a per-user cost basis.
34 The ANAO reviewed the PLANES database clearance records for AFP’s JACET employees as at August 2017. This review did not include all Child Protection Operation employees, many of whom are based in Canberra; only regionally-based JACET employees.
35 AFP, Agenda item 7: Mental Health Report, to the National Safety Committee, 19 October 2017.
36 AFP Minute, Risk management of AFP member health issues, 15 April 2015.
37 AFP Minute, Risk management of AFP member health issues, 15 April 2015.
38 Measurement of risk factors has limitations as a predictive tool as not everyone exposed to a mental health risk factor will have an adverse outcome. Risk factors interact, and multiple and persistent risk factors predict more strongly than any individual risk factor.
39 Risk factors are occurrences that increase the likelihood that a mental health problem or mental illness will develop. For example the AFP has recognised that exposure to explicit material is a psychological health and safety workplace hazard.
40 Enhancing factors are those that decrease the likelihood that a mental health problem or mental illness will develop, such as good social support.
41 Department of Health, National Mental Health Policy 2008, 2.3 Preventing mental health problems and mental illness, and reducing suicide risk, available from: <http://www.health.gov.au/internet/publications/publishing.nsf/Content/mental-pubs-n-pol08-toc~mental-pubs-n-pol08-2~mental-pubs-n-pol08-2-3> [accessed 21/08/2017].
42 ibid.
43 NSW Government, Mental Health and Wellbeing Strategy for First Responder Organisations in NSW, 2016, p 15.
44 Victoria Police, Victoria Police Mental Health Review: An independent review into the mental health and wellbeing of Victoria Police employees, May 2016, p 10.
45 ibid. p 32.
46 The 2017 Handbook replaces the previous AFP Practical Guide on Wellbeing Support for Members Dealing with Explicit Material.
47 The requirements are for mental health assessments to be conducted annually (at a minimum) and to have a psychological clearance in place before commencing in a JACET position.
48 Psychological clearances are required prior to an individual commencing in a role and are discussed in paragraphs 3.3 and 3.4. Mental health assessments are discussed in paragraphs 3.29 and 3.30 and are (at a minimum) annual mental health check-ins with employees in high risk roles.
49 AFP, AFP Weekly National Managers Forum, 20 March 2017, p 17.
50 Queensland Audit Office, Managing the Mental Health of Queensland Police Employees: Report 2 2017–18, October 2017, pp. 35-36.
51 The debrief form includes a Traumatic Stress Exposure Scale – Revised (TSES-R) questionnaire designed to measure the frequency and severity of traumatic events during deployment, a list of major stressors that can occur while on deployment and the extent they affected the employee.
52 AFP Comcare claim information pre-1989 was held in the previous AFP system and was not available for analysis.
53 Comcare, Guidelines for Rehabilitation Authorities 2012: Safety, Rehabilitation and Compensation Act 1988 Section 41.
54 Treatment options may include, but are not limited to: three GP consultations and six psychological sessions.
55 Queensland Audit Office, Managing the Mental Health of Queensland Police Employees: Report 2 2017–18, October 2017, pp. 54-55.
56 Auditor General of Canada to the Parliament of Canada, Independent Audit Report 4 – Mental Health Support for Members – Royal Canadian Mounted Police, Spring 2017, p 19.
57 Since the establishment of the Welfare Officer Network in July 2017, the Family Liaison Officer has received the same training and support as Welfare Officers and provides support to family dependants on and offshore.
58 AFP employees who are exposed to a critical or traumatic incident (for example vehicle accident scene, deceased person, assault) can get focused support 24 hours a day. This may involve immediate response in accordance with AFP policies, follow-up counselling support of the individual and in some cases family follow-ups, as appropriate.
59 The main activities of the Chaplaincy include: spiritual, religious and pastoral wellbeing support to members, retired members, and families; support in/to critical and traumatic incidents and their follow-on effects, or other emergency situations; and special memorial and commemorative services.
60 AFP, Standard Operation Procedure: AFP Chaplaincy Network, June 2017.
61 The app is confidential and the information entered into it by a user can only be accessed by that user.
62 Heads Up and Beyond Blue, Good practice framework for mental health and wellbeing in first responders organisations, May 2016, p. 29.
63 An example of a post-employment support service is the Retired Peer Support Officer Program, which is a volunteer group of former Victoria Police officers who support former colleagues who ‘may not be travelling too good’. Further information on this service is available from <www.retiredpeersupport.com.au>.
64 Although included as a ‘support service’ in the survey, the AFP guidance to staff does not include ‘colleagues’ as a support service and was not included in the average response analysis.
65 Or in hard copy.
66 Under the Work Health and Safety Act 2011, a ‘notifiable incident’ is one that involves the death of a person; a serious injury or illness of a person (that, for example, requires immediate hospitalisation); or a dangerous incident (such as exposure to the collapse or partial collapse of a structure).
67 Costs reflect both the cost-to-date as well as Comcare’s estimated future costs.
68 The pilot was prompted by academic research indicating that cumulative exposure to traumatic events increases the risk of psychological injury, with rates of Post-Traumatic Stress Disorder and depression increasing with each additional traumatic exposure.