Browse our range of reports and publications including performance and financial statement audit reports, assurance review reports, information reports and annual reports.
Australian Government Funding of Public Hospital Services — Risk Management, Data Monitoring and Reporting Arrangements

Please direct enquiries through our contact page.
The audit objective was to assess the effectiveness of risk management, data monitoring and public reporting arrangements associated with the Australian Government's funding of public hospital services under the 2011 National Health Reform Agreement (NHRA).
Summary and recommendations
Background
1. In 2016–17, there were 695 public hospitals in Australia. Each state1 operates its own public hospital system. Under the 2011 National Health Reform Agreement (NHRA), the Australian Government contributes to the cost of operating these public hospitals. In 2017–18, the Australian Government provided $19.94 billion under the NHRA, with the states providing $26.57 billion. The Australian Government contribution is provided primarily on the basis of ‘activity based funding’ (ABF) — a structure where hospitals are funded for the number and mix of patients they treat.2
2. The NHRA specified the establishment of two ‘national bodies’ plus a statutory position to administer the new public hospital funding arrangements; the Independent Hospital Pricing Authority (Pricing Authority), the National Health Funding Body (Funding Body), and the Administrator of the National Health Funding Pool3 (the Administrator).
3. Amongst other functions4, the Pricing Authority determines the National Efficient Price (NEP), a key input into the calculation of the Australian Government’s National Health Reform (NHR) ABF contribution. The Funding Body assists the Administrator in undertaking their functions, including advising the Treasurer on both the total Australian Government NHR payment contribution for the upcoming year and whether any adjustments should be made to payments after the end of the year due to changes in number of hospital services provided or other reasons. The Administrator also publishes reports on Australian and state government NHR funding levels and numbers of public hospital services.
Rationale for undertaking the audit
4. The Pricing Authority and Funding Body have important roles under NHRA arrangements through setting the efficient price of public hospital services and then calculating and administering Australian Government public hospital funding. The audit was selected as the integrity of key processes in both entities are highly reliant on the accuracy and completeness of state public hospital cost and service activity data.
5. The audit examines whether the NHR funding arrangements, including public reporting, provides transparency on the allocation of Australian Government funding. In a different context, the ANAO’s audit Monitoring the Impact of Australian Government School Funding5 highlighted a lack of sufficient assurance that relevant Australian Government funding had been distributed to schools on the basis of need as required by the relevant legislative framework. The current audit also assesses progress towards relevant policy objectives under the NHRA. The importance of monitoring the impact of Australian Government funding, and to provide greater accountability, was also a theme in the ANAO’s school funding audit.
Audit objective and criteria
6. The audit objective was to assess the effectiveness of risk management, data monitoring and public reporting arrangements associated with the Australian Government’s funding of public hospital services under the 2011 National Health Reform Agreement (NHRA).
7. To form a conclusion against this objective, the ANAO adopted two high-level criteria:
- the Pricing Authority and Funding Body have appropriate processes for managing risks to the accuracy of the public hospital service and cost data and to monitor significant changes to the data; and
- relevant Australian Government entities appropriately utilise available data to provide transparent public reporting on both the Government’s funding of public hospital services and progress towards the hospital-related policy objectives of the NHRA.
8. The audit scope does not include an assessment of the technical process through which the Pricing Authority determines the National Efficient Price or National Efficient Cost or through which the Funding Body calculates and subsequently reconciles Australian Government funding amounts.
Conclusion
9. The Pricing Authority and the Funding Body have effectively implemented data-related risk management and monitoring arrangements that are consistent with their public hospital funding roles under the National Health Reform Agreement (NHRA). Public reporting by a range of Australian Government entities provides reasonable transparency regarding funding levels, numbers of services and progress towards NHRA objectives of improved hospital efficiency, patient access, and safety and quality of clinical care in hospitals. The failure to implement the agreed reporting at the Local Hospital Network level has weakened the NHRA’s ability to drive systematic improvement in the performance of public hospitals across Australia.
10. The Pricing Authority and Funding Body have put in place controls to mitigate risks posed by inaccurate or incomplete data. The nature of these controls and other risk-related processes are consistent with their respective roles under the NHRA.
11. Both the Pricing Authority and Funding Body monitor public hospital service and cost data to identify and analyse any significant changes. The mandate of the Funding Body to undertake more detailed analysis on the causes of growth in Australian Government activity based funding (ABF) could benefit from clarification.
12. Agreement has also not been reached between stakeholders on an approach to manage the risks of the Australian Government making duplicate payments for the same public hospital service. Recent work indicates that these payments may be in the range of $172 million to $332 million per year.
13. There is public reporting by Australian Government entities on public hospital funding provided under NHRA. Transparency regarding the fulfilment of state governments funding commitments could be improved. Estimates of the number of public hospital services delivered by individual Local Hospital Networks are reported, noting that the actual number of services are only reported at the aggregated national level. The absence of the originally intended Local Hospital Network level performance reporting has weakened the reporting framework’s ability to achieve associated performance improvement objectives under the NHRA.
14. Public reporting shows mixed progress against NHRA hospital performance objectives. There have been some positive trends regarding hospital efficiency. On patient access, emergency department performance has declined slightly, but for elective surgery there have been improvements in some indicators. There has been no notable progress on improving the safety and quality of clinical care, although only a limited range of performance indicators are currently reported on.
Supporting findings
15. Under the NHRA, the Australian and state governments are responsible for the integrity of the data held within their systems, including data provided to the Pricing Authority and Funding Body.
16. The 2017 Addendum to the NHRA introduced additional data quality and integrity measures. Notably, state governments must include a statement of assurance regarding the accuracy and completeness of service activity data used to support the reconciliation of Australian Government ABF payments. The value of the statement of assurance process has been reduced by inconsistencies in the level of information provided by states against its required elements.
17. Both the Pricing Authority and Funding Body have embedded systematic risk management strategies and practices into the key ABF-related business processes that use state data. These include undertaking a range of data validation and quality review processes in relation to both cost and service activity data.
18. Through mutual representation on each entity’s advisory committees, the Pricing Authority and Funding Body have awareness of, and communicate about, their respective data-related risk management approaches.
19. Both the Pricing Authority and Funding Body have undertaken or commenced reviews of their broader risk management frameworks in 2018. Both entities regularly review their risk registers and other relevant process documents such as data plans.
20. The Pricing Authority and Funding Body monitor relevant data to identify significant changes and trends. States consider that the conduct of this work by the Funding Body is inconsistent with its key functions under the NHRA and the National Health Reform Act 2011.
21. In part due to lack of agreement between stakeholders about the use of relevant data, the Funding Body has not been able to accurately monitor the extent to which the Australian Government is making duplicate payments for public hospital services through the NHRA and Medicare Benefits Schedule (MBS). Preliminary work by the Funding Body does however indicate that potential duplicate payments may be in the range of $172 million to $332 million per year. The lack of agreement has also meant that the Department of Health has not had access to the matched public hospitals MBS data that would facilitate more comprehensive compliance and recovery action on potential duplicate MBS payments.
22. The Performance and Accountability Framework established under the NHRA was only partially implemented. Notably, the intended Local Hospital Network level reporting never occurred, weakening the framework’s ability to drive improved performance and achieve the associated objectives under the NHRA. Some public reporting against a limited set of performance indicators has occurred. Work has commenced to consolidate the existing multiple health reporting frameworks and develop a definitive set of performance indicators for public reporting.
23. Public reporting, mainly by the Administrator of the National Health Funding Pool, provides transparent information on Australian Government public hospital funding services down to the Local Hospital Network level. However, public reporting does not provide clarity on whether state governments are fulfilling their commitment in the NHRA to maintain their own 2017–18 funding of public hospital services at 2015–16 levels.
24. Public reporting by the Administrator of the National Health Funding Pool provides transparent information on the forecasted volume of public hospital funding services expected to be delivered at the Local Hospital Network level. The Administrator also reports the actual number of services delivered, but only at the aggregated national level rather than at the local level.
25. Existing public reporting provides a reasonable level of information about the mixed progress towards the hospital-related policy objectives under the NHRA of increased efficiency, patient access and safety and quality of clinical care. Reporting on efficiency suggests a modest improvement based on the stability of the national efficient price and improvements in the time a patient spends in hospital compared to expectations. Reporting on patient access suggests a slight decrease in performance against emergency department indicators, contrasted by a slight improvement in elective surgery related indicators. There has been no notable progress on improving the safety and quality of clinical care, although only a limited range of performance indicators are currently reported on.
26. The current development of a definitive set of performance indicators under the 2017 Australian Health Performance Framework should assist with the transparency and reliability of future reporting.
Recommendations
Recommendation no.1
Paragraph 2.61
The Department of Health:
- work with relevant state government entities to reach agreement on the appropriate data monitoring analysis roles for the Independent Hospital Pricing Authority and National Health Funding Body; and
- incorporate the agreed roles into the revised National Health Reform Agreement currently under negotiation.
Department of Health: Agreed.
Recommendation no. 2
Paragraph 2.72
The Department of Health:
- identify and prevent potential duplicate payments, including Medicare Benefits Schedule payments, by the Australian Government for public hospital services; and
- identify and recover past duplicate payments to the maximum extent permitted by law.
Department of Health: Agreed.
Recommendation no. 3
Paragraph 3.15
The Department of Health seek the agreement of states to implement reporting arrangements that provide transparency on whether state governments are maintaining public hospital services funding levels in accordance with National Health Reform Agreement obligations.
Department of Health: Agreed.
Summary of entity responses
27. Summary responses were received from the Department of Health and the Independent Hospital Pricing Authority and are provided below. The National Health Funding Body did not provide a summary response. The full responses of all three entities are at Appendix 1.
Department of Health
The Department is pleased that the ANAO found public reporting by a range of Australian Government entities in the Health Portfolio provides reasonable transparency regarding funding levels, number of services and progress towards the National Health Reform Agreement objectives of improved public hospital efficiency, patient access, and safety and quality of clinical care in hospitals.
Also positive, the report finds the Independent Hospital Pricing Authority and the National Health Funding Body have effectively implemented data-related risk management and monitoring arrangements are consistent with their public hospital funding roles under the National Health Reform Agreement.
The report has identified the absence of performance reporting at the Local Hospital Level (LHN) areas has limited the reporting framework’s ability to achieve the performance improvement objectives under the National Health Reform Agreement. While the proposal has merit, the department notes the LHNs vary considerably in characteristics, size and service mix, and their composition is determined by the states and territories. Any future performance reporting at the LHN level will be dependent on state and territories providing this data.
The report proposes more comprehensive compliance and recovery action on potential duplicate payments under the Medicare Benefits Schedule (MBS) and National Health Reform Agreement. MBS compliance activities are a part of the department’s normal business, however, the use of matched National Health Reform funding and MBS claims is required to comprehensively identify duplicate payments. A pilot data matching activity has been progressed in a careful and methodical manner given inter-agency and inter-jurisdictional complexity. The department agrees that the future effectiveness of related compliance action is largely dependent on agreement by stakeholders about the use of relevant data and will continue to work toward this outcome in National Health Reform Agreement negotiations.
Independent Hospital Pricing Authority
The Independent Hospital Pricing Authority (IHPA) has developed and implemented robust risk management processes since the agency was established in 2011.
Agency staff regularly reviews the strategic risk register, and risk treatments are in place for all significant risks that have been identified. Those risks and their treatments are considered by IHPA’s executive, its audit and risk committee and the Pricing Authority.
The quality of activity and cost data supplied by jurisdictions to IHPA for the purposes of determining the NEP and NEC has consistently been identified as a key risk. As a result IHPA has instituted a number of important strategies to validate and quality assure data supplied by states and territories, including the development of the Secure Data Management System (SDMS), which allows data submitters to validate data prior to submission to IHPA enabling them take steps to address any issues detected prior to submission.
Once data is submitted, IHPA undertakes considerable analysis of the data so as to understand the impact that decisions IHPA has taken may have had on the delivery of public hospital services.
Where potential issues are identified, IHPA works closely with jurisdictions through the Jurisdictional Advisory Committee (JAC) to identify and understand the underlying drivers.
IHPA works closely with the Administrator of the National Health Funding Pool and the National Health Funding Body (NHFB), and has commenced a process to address the formal identification of shared risks between the agencies, as required under the Commonwealth Risk Management Policy. As part of this a renewed Memorandum of Understanding between the NHFB and IHPA will be executed in early 2019.
Key messages from this audit for all Australian Government entities
Below is a summary of key messages, including instances of good practice, which have been identified in this audit that may be relevant for the operations of other Australian Government entities.
Governance and risk management
1. Background
Public hospitals in Australia
1.1 In 2016–17, there were 695 public hospitals in Australia providing 62,000 beds.6 Table 1.1 shows the geographic distribution of these facilities.
Table 1.1: Public hospitals in Australia, 2016–17
|
|
NSW |
Vic. |
Qld |
WA |
SA |
Tas. |
ACT |
NT |
Total |
|
Major cities |
66 |
53 |
20 |
19 |
15 |
0 |
3 |
0 |
176 |
|
Regional |
137 |
96 |
70 |
37 |
44 |
19 |
0 |
1 |
404 |
|
Remote |
19 |
2 |
33 |
35 |
18 |
4 |
0 |
4 |
115 |
|
Total |
222 |
151 |
123 |
91 |
77 |
23 |
3 |
5 |
695 |
Source: Australian Institute for Health and Welfare (AIHW).
1.2 Of the 695 public hospitals, 171 had 10 beds or fewer, and 302 had between 10 and 50 beds. The number of beds per head of population varies by location. In major cities, there are 2.43 beds per 1000 people. In regional areas, the figure is 2.79, and in remote areas, it is 3.58. On a national basis, the number of beds per head of population has remained virtually unchanged in the period 2012–13 and 2016–17.
1.3 The Australian Government does not operate any public hospitals.7 Each state8 operates its own public hospital system. Management of public hospitals within this system is through mainly regionally-based Local Hospital Networks (LHNs), of which there are 147 throughout Australia. Each LHN has an annual service agreement with the relevant state health department setting out the nature and number of public hospital services the relevant LHN will provide.
Public hospital funding under the National Health Reform Agreement
The National Health Reform Agreement
1.4 Prior to 2012, the Australian Government contributed to the cost of operating public hospitals primarily through multi-year ‘block’ funding arrangements.9 Payments were indexed by a range of factors, but generally included allowances for healthcare cost inflation, population and demographic changes, and higher demand for services resulting from better technology.10 During this period the Australian Government also funded public hospitals under a range of national partnership arrangements and programs.11
1.5 The National Health Reform Agreement (NHRA) was agreed by the Council of Australian Governments (COAG) in August 2011. It introduced a fundamental change whereby Australian Government payments to public hospitals would be primarily made on the basis of ‘activity based funding’ (ABF) — a structure where hospitals are funded for the number and mix of patients they treat.12 Apart from the quality and safety matters covered in Table 1.4, Australian Government funding levels under the NHRA are not dependent on the states achieving any performance benchmarks or implementing specific reform measures.
1.6 The NHRA specified the establishment of two ‘national bodies’ plus a statutory position to administer the new public hospital funding arrangements; the Independent Hospital Pricing Authority (Pricing Authority), the National Health Funding Body (Funding Body), and the Administrator of the National Health Funding Pool (the Administrator). The respective roles and responsibilities of these bodies, as well as those of other relevant Australian Government entities, are outlined in Table 1.2.
Table 1.2: Entity roles and responsibilities
|
Entity |
Roles and responsibilities |
|
Pricing Authority |
Determining the National Efficient Price (NEP), a key input into the calculation of the Australian Government’s National Health Reform (NHR) ABF amount. The NEP provides a price signal or benchmark for the efficient cost of providing hospital services. Determining the National Efficient Cost (NEC), which establishes the Australian Government funding contribution to (mostly rural) block funded hospitals. It represents the average cost of block funded hospitals across Australia. Determining the public hospital functions that are to be funded by the Australian Government. Developing national classifications for public hospital activity. |
|
Administrator |
Calculating the Australian Government NHR funding amounts and advising the Australian Government Treasurer on these. Overseeing payment of Australian Government NHR funding flowing through the National Health Funding Pool. Reconciling the estimated and actual volume of public hospital service delivery and advising the Australian Government Treasurer regarding any proposed additional reconciliation payments. Public reporting of funding and volume of services provided. |
|
Funding Body |
Assisting the Administrator in carrying out his or her functions. |
|
Treasurer |
Approving the NHR Australian Government funding amounts. |
|
Department of Health |
Providing health and hospitals policy advice to the Australian Government, including negotiating a new public hospital funding agreement to take effect from 2020. Administering related funding programs including the Medicare Benefits Schedule and Pharmaceutical Benefits Scheme. |
Source: National Health Reform Agreement 2011 and entity documentation.
1.7 The Pricing Authority was established under the National Health Reform Act 2011 and the Administrator and Funding Body under an amendment to the Act in 2012. Separating the pricing function (Pricing Authority) from the funds administration function (Administrator and Funding Body) into distinct independent entities was intended to address concerns raised by some states that the Administrator would be handling state funds and therefore would need to be an officer appointed by the states.13
Calculating Australian Government funding
1.8 Figure 1.1 shows NHR funding provided by the Australian Government and the states over the life of the NHRA. Australian Government funding in 2017–18 was $19.94 billion with total state government funding14 $26.57 billion.
Figure 1.1: National Health Reform Funding 2012–13 to 2017–18
Note: Funding refers to amounts actually paid in the relevant year. State funding has been adjusted for cross border payments
Source: ANAO analysis of public reporting by Administrator.
1.9 The Australian Government’s annual NHR funding contribution is the total of three funding components: activity based funding, block funding and public health funding.
Activity based funding
1.10 Australian Government ABF payments made in 2017–18 were $17.22 billion, and constituted 86.4 per cent of its NHR funding for public hospitals.
1.11 Under the funding formula set out in the NHRA, the Australian Government’s annual ABF contribution for each state is the sum of:
- the previous year’s Australian Government ABF amount15;
- a price adjustment — 45 per cent of any change in the NEP from the previous year; and
- a service volume adjustment — 45 per cent of any change in the estimated number of services to be delivered as compared to the previous year. 16
1.12 The key steps in calculating the NEP (and thus the ABF price adjustment) are outlined in Box 1.17
|
Box 1: Key steps in the Pricing Authority’s annual calculation of the National Efficient Price |
|
Step 1: Use state public hospital cost and service activity data to calculate the weighted average cost of delivering a public hospital service in Australia. Step 2: Deduct specified ‘out of scope’ funding and services to calculate a revised average cost. Step 3: Apply an indexation factor to allow for estimated increases (or decreases) in the cost of delivering services in the relevant NEP year. For example, the 2018–19 NEP is based on 2015–16 cost data and indexation allows these costs to be projected forward to 2018–19. |
1.13 Both the number of public hospital services, and the nature of those services, to be delivered change from year to year. For NHRA purposes, services are expressed as National Weighted Activity Units (NWAUs) (see Box 2).
|
Box 2: Measuring and pricing services: the National Weighted Activity Unit |
|
The NWAU provides a way to compare and value each public hospital service by weighting it for clinical complexity, with one NWAU equalling the ‘average’ hospital activity. Simple (and thus less expensive) hospital services are worth a fraction of an NWAU, while more intensive and expensive services have higher weightings. For example in 2018–19:
Given that the NEP for 2018–19 is $5012 per NWAU, the respective ‘efficient cost’ of delivering these services are:
Price weights and adjustments (expressed as NWAUs) are also applied to the price to reflect the legitimate and unavoidable variations in the cost of delivering health care services, such as the location of the patient’s residence and patient complexity. |
1.14 Under transitional arrangement accompanying the introduction of the NHRA, the pre-NHRA block funding amounts each state was receiving effectively formed the ‘base amount’ from which Australian Government ABF funding from 2014–15 onwards has been calculated. The net result is that current Australian Government ABF funding levels are still influenced by the varying proportions of each state’s public hospital costs that were funded by the Australian Government under pre-NHRA block funding arrangements. These arrangements were the result of calculations based on historical costs, intergovernmental negotiation and prior government decisions. These calculations incorporated funding growth based on population estimates rather than number and mix of patients treated, whereas ABF contributions are based on activity. As a consequence, each jurisdiction receives a different Australian Government ABF contribution per NWAU as shown in Table 1.3. Tasmania receives the highest funding at $2236 and the Northern Territory the lowest at $1497. On a national basis, Australian Government funding is $1940 per NWAU.
Table 1.3: Australian Government 2016–17 activity based funding
|
Jurisdiction |
Australian Government activity based funding per NWAU ($) |
Proportion of the National Efficient Price funded by Australian Government (%) |
|
New South Wales |
1849 |
37.9 |
|
Victoria |
1942 |
39.8 |
|
Queensland |
2058 |
42.1 |
|
Western Australia |
2071 |
42.4 |
|
South Australia |
1807 |
37.0 |
|
Tasmania |
2236 |
45.8 |
|
Australian Capital Territory |
2142 |
43.9 |
|
Northern Territory |
1497 |
30.7 |
|
National |
1940 |
39.7 |
Note: As at early December 2018, 2016–17 figures were the most recent reconciled figures. The 2016–17 National Efficient Price is $4883 per NWAU.
Source: ANAO analysis of Administrator and Funding Body documents.
1.15 The impact of the ABF formula (under which the Australian Government is funding 45 per cent of efficient growth) means the differences will reduce over time. Chapter 3 provides more information on Australian Government contributions and funding levels over time for each state.
1.16 Some people are admitted into public hospitals as private patients. Australian Government ABF is payable for such patients, but with a variable discount applied to account for the revenue received by the treating hospital from the health insurer as well as any Australian Government payments to treating doctors through the Medicare Benefits Schedule (MBS).18
Block funding
1.17 Under the NHRA some public hospital services and functions are considered to be more appropriately funded through block grants rather than ABF.19 The Pricing Authority has developed block funding criteria in consultation with the states, and these criteria determine which services and functions are eligible for block funding. Australian Government block funding totalled $2.33 billion in 2017–18.
1.18 The major categories of block funding are:
- approximately 400 small rural hospitals receive funding under the national efficient cost (NEC) process (total payments of $903 million for 2017–18);20
- funding for teaching, training and research (total payments $536 million for 2017–18);
- other non-admitted services (total payments of $890 million for 2017–18).21
1.19 The Pricing Authority receives hospital level cost data from the Australian Institute for Health and Welfare (AIHW)22 for the NEC model to determine block funding for small rural hospitals. The Pricing Authority does not receive cost data for the remaining categories in paragraph 1.18, instead relying on advice from the states on their expected expenditure. The Pricing Authority commissioned a review in 2018 to provide better information as to whether these block funding amounts accurately reflect actual costs.23
Public health funding
1.20 The Australian Government provided $387 million in 2017–18 for public health activities. This funding is calculated by the Australian Government Treasury and includes amounts for general public and youth health services and essential vaccines. Under the NHRA, states have complete discretion about how they use this funding in relation to their own health-related activities.
Public hospital funding flows
1.21 Under NHRA arrangements, a National Health Funding Pool (the Pool) has been created to consolidate all Australian Government ABF and block and state ABF. The Pool is comprised of separate Reserve Bank of Australia (RBA) bank accounts for each state. In addition, each state has a discrete State Managed Fund for the purpose of receiving block funding. Each State Managed Fund is administered by the individual jurisdictions and lies outside the RBA system.
1.22 The Australian Government Treasury makes monthly ABF, block and public health funding payments into the Pool, with the block funding amount flowing through the Pool to each of the State Managed Funds. Each state determines when and how much funding they deposit into the Pool and the State Managed Funds. With the exception of some payments that go direct to state government health departments, payments from the Pool and the State Management Funds are then transferred to the LHNs who are responsible for delivering public hospital services. A simplified representation of the relevant funding and payment flows is illustrated in Figure 1.2.
Figure 1.2: Simplified 2017–18 public hospital funding and payment flows

Note: Differences in the total funding and total payments are due to timing issues of funds moving into and out of the Funding Pool and State Managed Funds. Payments of activity based funding out of the National Health Funding Pool are made through a Department of Human Services payments system. The NSW Ministry of Health transfers the $10.09 billion shown above to NSW LHNs. See paragraph 3.9 for more detail.
Source: Administrator’s 2017–18 Annual Report and ANAO analysis.
1.23 The monthly payments made into the Pool are prospective payments based on LHN estimates of hospital service activity levels.24 At the end of each six-month (July to December) and annual (July to June) period, the states provide actual hospital activity data to the Funding Body (via the Pricing Authority) to enable it to reconcile these to the previous estimates. The Australian Government’s payments are then adjusted annually in arrears to account for this reconciliation.
1.24 The Pool’s accounts are audited each year by the respective Auditor-General for each state, and each audited financial statement is published in the Administrator’s annual report.
NHRA hospital related policy objectives
1.25 In addition to increasing the proportion of public hospital costs funded by the Australian Government and promoting the transparency of how public hospitals are funded, key NHRA objectives relating to the public hospital system are listed below.
- Improving public hospital efficiency. Efficiency is usually defined in terms of minimising the cost of a specific hospital service.
- Improving patient access to hospital services. Accessibility is usually defined as being able to obtain health care at the right place and right time.
- Improving standards of clinical care. This is usually defined in terms of patient safety (avoidance of adverse events) but more recently quality of care concepts, such as clinical outcomes and a patient’s experience in hospital, are being incorporated into development of new performance indicators.
The 2017 NHRA Addendum
1.26 The NHRA commenced in 2012–13 with a transition period for the first two years, whereby Australian Government funding to the states was capped at the funding levels that would have applied under previous National Healthcare Specific Purpose Payment block funding agreement. From 2014–15 to 2016–17 the Australian Government funded 45 per cent of increased costs flowing from the ‘efficient growth’25 of public hospital services.
1.27 Australian Government funding was to increase from 45 per cent of efficient growth to 50 per cent from 2017–18 onwards. However, with Australian Government NHR funding growth accelerating from 5.6 per cent in 2013–14 to over 11 per cent in both 2014–15 and 2015–16,26 the Australian Government negotiated an addendum to the NHRA that retained its contribution at 45 per cent. In addition, the addendum introduced a 6.5 per cent national cap on growth in the Australian Government contribution to apply from 2017–18.
1.28 Table 1.4 summarises key provisions in the addendum.
Table 1.4: Key 2017 NHRA Addendum provisions
|
Amendment |
Additional details |
|
Australian Government funding contribution |
Australian Government funding remains at 45 per cent of the cost efficient growth, subject to the funding cap. |
|
Funding Cap |
Limits total Australian Government funding increases to 6.5 per cent annually from 2017–18. Funding increases to individual states is also limited to 6.5 per cent except where slower growth in some jurisdictions allows left over funds to be proportionally redistributed to higher growth jurisdictions as part of the annual reconciliation process. |
|
Incorporation of quality and safety into hospital pricing and funding |
Any episode giving rise to a sentinel event27 will not be funded by the Australian Government. A pricing and funding model for hospital-acquired complications will be introduced from 1 July 2018, and an appropriate pricing and funding model for avoidable hospital readmissions will be determined after 1 July 2018. |
|
Reforms to decrease avoidable demand for public hospital services |
Agreement to develop a range of coordinated care reforms for patients with chronic and complex conditions to deliver better care and reduce avoidable demand for health services. |
|
Data quality and integrity |
A commitment to jurisdictions working together and with the national bodies to share and work towards best practice approaches. A data conditional payment to encourage the prompt provision of the required data for timely reconciliation. Each jurisdiction must annually issue a Statement of Assurance on the completeness and accuracy of approved data submissions to the Australian Government. Public reporting on compliance with data requirements by the Administrator. |
|
Certainty of reconciliation |
The final Australian Government funding entitlement of a jurisdiction will not be adjusted unless any issues affecting the accuracy of the entitlement is advised to the Administrator within 12 months of the end of the financial year. The Administrator can also identify issues including inaccuracies or errors within 12 months of the end of the relevant financial year. |
Source: NHRA Addendum.
1.29 At the time of the audit, a new five-year national funding agreement is being negotiated to take effect from July 2020. Figure 1.3 provides an overview of the timeframes of health care agreements from 1 July 2008.
Figure 1.3: Overview of health care agreement timeframes
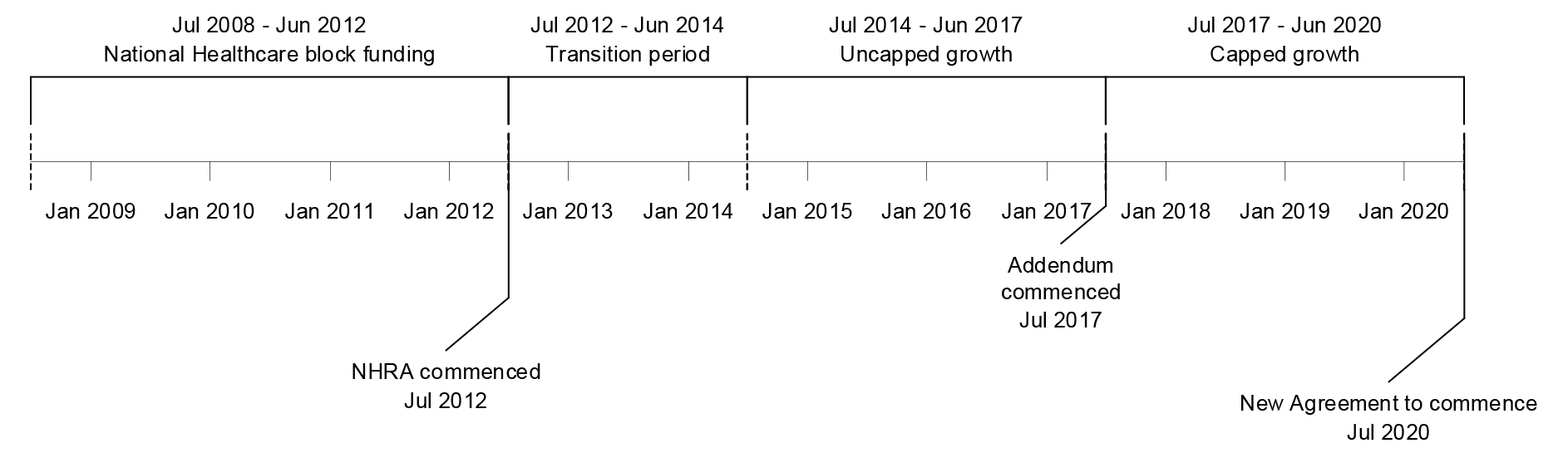
Source: NHRA, NHRA Addendum and COAG Heads of Agreement.
Rationale for undertaking the audit
1.30 The Pricing Authority and Funding Body have important roles under NHRA arrangements through setting the efficient price of public hospital services and then calculating and administering Australian Government public hospital funding. The audit was selected as the integrity of key processes in both entities are highly reliant on the accuracy and completeness of state public hospital cost and service activity data.
1.31 The audit examines whether the NHR funding arrangements, including public reporting, provides transparency on the allocation of Australian Government funding. In a different context, the ANAO’s audit report Monitoring the Impact of Australian Government School Funding28 highlighted a lack of sufficient assurance that relevant Australian Government funding had been distributed to schools on the basis of need as required by the relevant legislative framework. The current audit also assesses progress towards relevant policy objectives under the NHRA. The importance of monitoring the impact of Australian Government funding, and to provide greater accountability, was also a theme in the ANAO’s school funding audit.
Audit approach
Audit objective, criteria and scope
1.32 The audit objective was to assess the effectiveness of risk management, data monitoring and public reporting arrangements associated with the Australian Government’s funding of public hospital services under the 2011 National Health Reform Agreement (NHRA).
1.33 To form a conclusion against the audit objective, the ANAO adopted the following high level criteria:
- the Pricing Authority and Funding Body have appropriate processes for managing risks to the accuracy of the public hospital service and cost data and to monitor significant changes to the data; and
- relevant Australian Government entities appropriately utilise available data to provide transparent public reporting on both the Government’s funding of public hospital services and progress towards the hospital-related policy objectives of the NHRA.
1.34 The audit scope does not include an assessment of the technical process through which the Pricing Authority determines the NEP and NEC or through which the Funding Body calculates and subsequently reconciles Australian Government funding amounts.
Audit method
1.35 The audit method comprised:
- analysis of relevant aspects of the Pricing Authority and Funding Body’s operations, including data-related risk management and monitoring process associated with core business processes;
- reviewing the activities of hospital financing and medical benefits areas of the Department of Health, including advice provided to the Australian Government;
- obtaining evidence from the offices of state Auditors-General about their recent work on public hospital funding and performance29;
- obtaining evidence from the Australian Institute for Health and Welfare, the Australian Commission on Safety and Quality in Healthcare, and the Productivity Commission regarding their hospital-related performance framework and reporting roles; and
- analysis of relevant data held and/or reported by the Funding Body, Administrator, Australian Institute for Health and Welfare, the Australian Commission on Safety and Quality in Healthcare, and the Productivity Commission.
1.36 The audit was conducted in accordance with ANAO Auditing Standards at a cost to the ANAO of approximately $572,785. The team members for this audit were Angus Martyn, Renee Hall, Michael Jones, Ailsa McPherson, Danielle Page, Paul Bryant and Julian Mallett.
2. Risk management and monitoring
Areas examined
The ANAO examined whether the Independent Hospital Pricing Authority (Pricing Authority) and National Health Funding Body (Funding Body) have appropriate processes for managing risks to the accuracy of public hospital service activity and cost data and to monitor significant changes to the data.
Conclusion
The Pricing Authority and Funding Body have put in place controls to mitigate risks posed by inaccurate or incomplete data. The nature of these controls and other risk-related processes are consistent with their respective roles under the National Health Reform Agreement (NHRA).
Both the Pricing Authority and Funding Body monitor public hospital service and cost data to identify and analyse any significant changes. The mandate of the Funding Body to undertake more detailed analysis on the causes of growth in Australian Government activity based funding (ABF) could benefit from clarification.
Agreement has also not been reached between stakeholders on an approach to manage the risks of the Australian Government making duplicate payments for the same public hospital service. Recent work indicates that these payments may be in the range of $172 million to $332 million per year.
Areas for improvement
The ANAO made two recommendations aimed at clarifying data monitoring and analysis roles and also preventing and/or recovering duplicate payments for public hospital services.
Does the National Health Reform Agreement include provisions about data quality and integrity?
Under the NHRA, the Australian and state governments are responsible for the integrity of the data held within their systems, including data provided to the Pricing Authority and Funding Body.
The 2017 Addendum to the NHRA introduced additional data quality and integrity measures. Notably, state governments must include a statement of assurance regarding the accuracy and completeness of service activity data used to support the reconciliation of Australian Government ABF payments. The value of the statement of assurance process has been reduced by inconsistencies in the level of information provided by states against its required elements.
2.1 Australian and state government entities are jointly responsible for the provision of a range of data to the Pricing Authority and Funding Body to enable them to carry out their functions under the NHRA, as outlined in Table 2.1.
Table 2.1: Key data provided to the Pricing Authority and the Funding Body
|
Type of data |
Data provider |
Data recipient |
Frequency of submission |
Purpose |
Accompanying data integrity statements |
|
Activity data |
|||||
|
Estimated number of services (expressed as National Weighted Activity Units or NWAUsa) to be delivered in coming year |
State government health departments |
Funding Body |
Annualb |
Input into calculating Australian Government Activity Based Funding (ABF) amounts |
Nil |
|
Actual number and detail of services delivered |
State government health departments |
Pricing Authority, who provides to the Funding Body |
Six monthlyc |
Input into calculating the Nationall Efficient Price (NEP) and National Efficient Cost (NEC); Input into reconciliation of Australian Government ABF payments against actual services delivered |
Statement of Assurance |
|
Cost data |
|||||
|
National Hospital Cost Data Collection |
State government health departments |
Pricing Authority |
Annual |
Input into calculating the NEP |
Data quality statement |
|
National Public Hospital Establishments Database |
Australian Institute for Health and Welfare (AIHW) |
Pricing Authority |
Annual |
Input into calculating the NEC |
Data quality statement |
|
Funding and other data |
|||||
|
De-identified pharmaceutical program payments |
Department of Health |
Pricing Authority |
Annual |
Input into calculating the NEP |
Nil |
|
De-identified Medicare Benefits Schedule (MBS) and Pharmaceutical Benefits Scheme(PBS) claims data |
Department of Health |
Funding Body |
Annual |
Match with activity data to identify potential duplicate payments |
Statement of assurance |
Note a: National Weights Activity Units (NWAUs) provide a way to compare and value each public hospital service by weighting it for clinical complexity, with one NWAU equalling the ‘average’ hospital activity. See Box 2 in Chapter 1.
Note b: Non-binding estimates can also be provided by states at any time.
Note c: Provided every six months up to 2017–18, however in accordance with the Pricing Authority’s three year data plan for 2018–19 to 2020–21, data will be submitted each quarter from 1 July 2018.
Source: ANAO summary of the three year data plans for the Pricing Authority and the Administrator.
2.2 Under the NHRA, governments are responsible for the integrity of data they provide to the national bodies, including the Pricing Authority and Funding Body.30 As part of this, all jurisdictions must have appropriate independent oversight mechanisms for data integrity.31
2.3 During the negotiation of the NHRA Addendum in 2016 and 2017, the Funding Body developed a range of proposed measures intended to enhance integrity and assurance arrangements relating to the ABF system. These included:
- the development of a National Data Integrity Framework to improve the quality and timeliness of state activity data; promote a consistent national approach; and establish a national standard against which state Auditors-General could undertake quality reviews; and
- that the Funding Body — on behalf of the Administrator of the National Health Funding Pool (the Administrator) — undertake a review of activity data to assist states to comply with their obligations under the NHRA.
2.4 Neither of these proposals were supported by the states as they were considered too prescriptive.32 However, agreement was reached that state governments must include a statement of assurance on the completeness and accuracy of the activity data submissions provided for the reconciliation process.
2.5 The required content of the statements of assurance, and associated administrative processes, were agreed between respective governments in December 2017. Under these processes, the statements of assurance are not made public but the Administrator does publicly report on whether a statement of assurance has been submitted by each jurisdiction.33 In terms of content, jurisdictions are required to provide commentary against three elements, with a fourth being optional, as illustrated in Table 2.2.
Table 2.2: Statements of assurance: summary of states’ commentary provided against agreed elements
|
|
Description provided of steps taken by state regarding completeness and accuracy of hospital service activity dataa |
Description provided of efforts by state to classify activity in accordance with current year’s standards, data plans and determinations |
Commentary on variations in activity levels and movements between ABF and block funding |
Any other commentary (optional) |
|
New South Wales |
Yes |
Yes |
Reports that activity growth was higher than expected due to increase in acute and emergency admissions. |
Provides links to new policies and describes strategies for improving health IT infrastructure. |
|
Victoria |
Yes |
Yes |
Reports lower than anticipated NWAU due to implementing a new coding standard. |
Nil information provided. |
|
Queensland |
Yes |
No |
Reports that there was no movement between ABF and block funding. |
Nil information provided. |
|
Western Australia |
Yes |
Yes |
Reports detailed information of changes in activity and movements between ABF and block funding at the hospital level. |
Provides information on changes in hospitals and their impact on the data collections. |
|
South Australia |
Yes |
No |
Nil information provided. |
Provides information on a discrepancy that is currently being investigated for one type of data. |
|
Tasmania |
Yes |
Yes |
Reports change in activity levels, and no movement between ABF and block funding. |
Provides information on technical issues with one data type. |
|
Australian Capital Territory |
No |
Yes |
Reports changes in two types of activity data. |
Nil information provided. |
|
Northern Territory |
Yes |
No |
Reports changes in activity data. |
Provides explanations for activity data streams affected by critical errors or high numbers of warning errors. |
Note a: This element is relevant to providing information on the oversight mechanisms for data integrity that each government has in place as per NHRA requirements.
Source: ANAO analysis of statements of assurance provided with the six month activity data submission in September 2018.
2.6 As shown in Table 2.2, there was significant variation in the detail of information against the second and third elements, and in some cases no commentary was provided at all, with no explanation provided for its absence. While it is to be expected that individual commentaries will reflect differences in the maturity of data collection and governance processes between jurisdictions, the value of the statement of assurance process largely depends on a reasonable level of information being provided against all three compulsory elements. This is particularly so in light of the lack of progress in providing the Administrator with state data integrity frameworks.34 Neither the Pricing Authority nor Funding Body took any follow-up action regarding the lack of commentary or information against some of the mandatory elements. However, the Funding Body did advise that it had used the statements of assurance to identify issues requiring investigation as part of the 2016–17 reconciliation process.
2.7 The Pricing Authority considered the statements could be enhanced if the results of any steps taken to promote completeness and accuracy of data (such as coding35 audits) were required to be included in the statement. This is a matter that could be usefully considered in the review of the content of the statements that is due to occur under the auspices of the cross-jurisdictional Health Services Principals Committee.
2.8 Cost data is accompanied by data quality statements, an arrangement that predates the introduction of statements of assurance. While under NHRA arrangements, jurisdictions are not required to provide these statements, all did so for the most recent (2016–17) round of cost data provided to the Pricing Authority. Jurisdictions provide information against four elements, as illustrated in Table 2.3.
Table 2.3: Data quality statement information: summary of states’ commentary provided against agreed elements
|
|
Indication of state’s conformance with Australian hospital patient costing standards (AHPCS)a |
Information on state’s data quality assurance arrangements |
Information on limitations in the provided data |
Notice of state’s plans to address data limitations (where relevant) |
|
New South Wales |
Data aligns with AHPCS version 3.1. |
Describes data reconciliation processes, audit program and third party peer reviews. |
Describes technical issues relating to five data types. |
Describes costing methodology changes to further refine and improve data collection. |
|
Victoria |
Data conforms with AHPCS version 3.1 — qualified for three data types. |
Describes compliance with Victorian cost data collection business rules and specifications, and data reconciliation reports. |
Describes technical or collection issues relating to four data types. |
Notifies it is transitioning to apply AHPCS standards for one data type. |
|
Queensland |
Data aligns with AHPCS version 3.1 — qualified for two data types. |
Nil information provided. |
Describes technical or collection issues relating to two data types. |
Nil information provided. |
|
Western Australia |
Data conforms with AHPCS version 3.1 — qualified for one data type. |
Describes data reviews by area health services and data reconciliation processes with the state health department; and data validation and matching processes with activity data. |
Describes: technical issues relating to one data type; that aggregate costs relating to one data type have been excluded; and notes the closure of hospitals and the impact on the casemix and service provision. |
Notifies that there is improved patient level costing process to allow for separate reporting of admitted emergency costs at all sites, and that it continues to work on costing the small amount of outpatient activity that remains at an aggregate level. |
|
South Australia |
Data conforms with AHPCS version 3.1. |
Describes the costing system and processing of data, and reviews by state health department in conjunction with Local Hospital Networks (LHNs). |
Describes technical and collection issues relating to four data types. |
Nil information provided. |
|
Tasmania |
Data conforms with AHPCS version 3.1. |
Limited information provided. |
Nil information provided. |
Nil information provided. |
|
Australian Capital Territory |
Data conforms with AHPCS version 3.1. |
Describes a recent system wide data review which included the cost data provided for 2016–17. |
Describes technical or collection issues with four data types. |
Nil information provided. |
|
Northern Territory |
Data conforms with AHPCS version 3.1 — qualified for three data types. |
Limited information provided. |
Describes technical and collection issues relating to three data types. |
Nil information provided. |
Note a: The Australian hospital patient costing standards (AHPCS) are intended to provide best practice principles to costing hospital products, with consistent application of the standards generating high quality, reliable and comparable data.
Source: ANAO analysis of data quality statements provided with 2016–17 cost data (used to calculate the 2019–20 NEP).
Have the Pricing Authority and Funding Body embedded systematic risk management strategies and practices into those key business processes that use state data?
Both the Pricing Authority and Funding Body have embedded systematic risk management strategies and practices into the key ABF-related business processes that use state data. These include undertaking a range of data validation and quality review processes in relation to both cost and service activity data.
2.9 The Commonwealth Risk Management Policy (CRMP) supports the Public Governance, Performance and Accountability Act 2013 (PGPA Act) and aims to strengthen the risk management practices of Australian Government entities. Entities subject to the CRMP ‘must ensure that systematic management of risk is embedded in key business processes’.
Risk management documentation
2.10 The ANAO reviewed the Pricing Authority and Funding Body’s key risk management policy and operational documents against the CRMP and relevant PGPA Act principles. The results of the review are outlined in Table 2.4.
Table 2.4: Pricing Authority and Funding Body risk management policy alignment
|
|
Pricing Authority |
Funding Body |
|
Entity type (as defined under the PGPA Act) |
Corporate Commonwealth entity |
Non-corporate Commonwealth entity |
|
CRMP requirements are mandatory |
Noa |
Yes |
|
Entity risk policy and framework aligned with CRMP |
Yes |
Yes |
|
Entity has risk register in place |
Yes |
Yes |
|
Entity risk register identifies relevant operational policies and procedures |
Yes |
Yes |
Note a: It is not mandatory for corporate Commonwealth entities (CCEs) to comply with the required elements of the CRMP however it states that CCE’s should review and align their risk management frameworks with the CRMP as a matter of good practice.
Source: ANAO analysis of entity risk management documentation.
2.11 The risk management policies and operational documents were largely aligned with the CRMP. The following minor improvements could be made:
- Pricing Authority36 — clear linking of its risk management policy to strategic objectives; and identifying the specific shared risks it manages through its communication and consultation practices. The management of shared risks between the Pricing Authority and the Funding Body is further discussed at paragraphs 2.33–41.
- Funding Body — clarifying its approach for measuring risk management performance.
2.12 In relation to the data required by the Pricing Authority and Funding Body to undertake their primary functions, a key risk identified by both entities is that data is of poor quality, not reliable or cannot be used. To assist in managing this broad risk, each entity publishes a rolling three year data plan. The data plans, which are developed with input from all jurisdictions and are updated annually, set out the approved data classifications37 and specifications38 for the required data, submission schedules and compliance reporting requirements.
2.13 The respective data plans of the Pricing Authority and Funding Body are appropriately aligned through setting common requirements such as data specifications.39 They are consistent with the data rationalisation objective in the NHRA, particularly the ‘single provision, multiple use’ concept.
Pricing Authority — key data review strategies and practices
ABF data quality
2.14 Consistent with its Data Quality Assurance Framework40, the Pricing Authority applies a range of quality-related processes to the activity and cost data it receives from states. These processes are intended to deliver improved data over time.
2.15 Since March 2017, all cost and activity data is submitted to the Pricing Authority through a secure data management system (SDMS) portal.41 Developed and owned by the Pricing Authority, the SDMS allows each state to run a validation check against the required data specifications contained in the Pricing Authority’s data plan before it submits the data. Validation reports that show the type and number of any errors in the data are also produced by the SDMS for the Pricing Authority once the data is submitted.42 In October 2018, the Pricing Authority completed a post-implementation review of the SDMS. The review indicated that data preparation and validation processes introduced under the SDMS have led to a reduction in the number of errors contained in relevant submissions and thus contributed to better data quality.
2.16 Following validation, activity and cost data is linked to create a merged data set. Quality assurance reports are produced both at the individual hospital and state level. The quality assurance reports include information on anomalies43, outliers44 and comparison of data with previous year’s results.45 The merged data and quality assurance results are then classified into three categories — ‘no material issues’, ‘some issues’ and ‘many issues — review required’. The results are provided to the Pricing Authority’s costing and pricing teams for review and comment, and any significant issues are referred back to the states, requesting comment or corrective action.
2.17 The ANAO reviewed the eight state level quality assurance reports for the 2016–17 cost and activity data that are being used to determine the NEP for 2019–20. As shown in Figure 2.1, the reports noted ‘some issues’ were found in most submissions in the five activity data streams, with three jurisdictions requiring review due to ‘many issues’ with acute or subacute activity data.
Figure 2.1: Number of jurisdictions overall data quality assurance result for 2016–17
Note: The Pricing Authority reporting indicates that ‘many issues’ represents the volume of issues represented in a data stream. For example, in one state’s result ‘many issues’ in the non-admitted activity data stream was due to the identification of 13,637 outliers.
Source: ANAO analysis of jurisdiction-level quality assurance reports.
2.18 Issues may be resolved through the relevant jurisdiction providing confirmation that the submitted data is correct, or in some cases formal resubmission of amended data. The resolution of issues is monitored by the Pricing Authority through its executive committee.46 Major data issues that continue over multiple submissions from the same state without improvement or resolution are publicly reported on the Pricing Authority’s website.47
2.19 Since 2015 there has been only one instance where public reporting of non-compliance directly relating to data quality has been required. That was caused by technical issues that prevented the relevant state from being able to provide non-admitted patient level activity data within agreed deadlines. The state subsequently provided the required data.
Financial reviews of ABF cost data
2.20 As an additional data validation measure, the Pricing Authority commissions an annual financial review to assess whether the cost data submitted by a sample of hospitals and LHNs reconciles with broader financial data in the relevant hospital and Local Hospital Network (LHN) systems. Participation by the states in the review process is voluntary, however all states engage in the process. The review of 2015–16 cost data was published in January 2018. The review did not find any significant deficiencies in the cost data48 and concluded that recent measures introduced in a number of jurisdictions had contributed to a more robust costing process. It also noted that some additional quality-related measures would be incorporated into the 2016–17 cost data collection process.49
2.21 Selection of the specific hospitals and LHNs to participate in the review is undertaken by the respective state health departments from a shortlist of ABF-funded hospitals and LHNs provided to them by the Pricing Authority. The mix of hospitals and LHNs on the shortlist are designed to achieve a variety of hospital sizes, complexity of services provided, and geographic locations.50 The size of the sample selected of the 2015–2016 cost data represents approximately four per cent of relevant hospitals and less than one per cent of LHNs. The sample size and selection process is not underpinned by a specific methodology to provide confidence that the review findings apply to ABF cost data in general or that the review is targeting higher risk hospitals or LHNs. The Pricing Authority advised the ANAO that the review sample size reflects a need to ‘balance the cost and effort of increased scope, with the improved benefits that may result from widening the scope’.51
Block funding
2.22 The major data input for the calculation of the NEC, which relates to Australian Government block funding of small rural hospitals under the NHRA, is the public hospital expenditure reported in the National Public Hospital Establishments Database (NPHED). The NPHED is a national dataset which comprises a core set of data elements agreed for mandatory collection and reporting at a national level. The NPHED is maintained by the Australian Institute for Health and Welfare and provided annually to the Pricing Authority. A data quality statement on the NPHED is published online.
2.23 The NEC Determination includes other categories of block funding, for services such as teaching, training and research and non-admitted mental health services (see paragraph 1.18). The funding amounts for these services are determined by the Pricing Authority on advice from the states. Where a state or territory advises an amount that would result in funding growth rate for these services greater than the NEC growth rate in that year (which was 2.9 per cent in 2018–19), the Pricing Authority requires additional evidence from the state before agreeing to this amount such as publicly available state budget papers. Where a state is unable to provide such supporting evidence, the Pricing Authority sets the relevant funding at the previous year’s amount, indexed by the NEC growth rate.52
2.24 As mentioned in Chapter 1, the Pricing Authority has undertaken a review on block funding to gain better information on whether the data underpinning jurisdictional advice, including the processes in place in each state to determine their block funding amounts, and the link between the amounts included in the NEC Determination and the funding provided by states and territories. The review found that the requirements to justify block funded amounts requested by the states have become more stringent over time and that the majority of states could break down block funding amounts with actual costs or expenditure on the services. The review also made three recommendations for improving the process of states nominating block funding amounts for the NEC Determination. The report was provided to Australian and state government health ministers for comment in early December 2018.
Funding Body — key data review strategies and practices
Calculation of Australian Government ABF contribution
2.25 Each state government provides the Funding Body with estimates of the number of public hospital services (expressed as NWAUs) that they anticipate each of their LHNs will provide for the upcoming financial year. This is a key data input into the Funding Body’s calculation of the level of Australian Government ABF. Estimates are provided at agreed milestone dates53 and are then updated when required.54
2.26 Once the NWAU estimates from each LHN are received, the Funding Body compares these with the NWAU figures contained in the service level agreements (SLAs) that each LHN has established with their relevant state health department.55 The ANAO conducted targeted testing of a sample of 15 LHN NWAU estimates against the relevant SLAs from a total population of 147 received by the Funding Body. All NWAU estimates tested matched the NWAU figures contained in the corresponding SLA.
2.27 The Funding Body also undertakes a review of the submitted NWAU estimates to identify any significant changes in the various activity categories (such as acute care or non-admitted services) from the previous year. Where the Funding Body identified such significant changes in 2018–19 estimates, there was evidence that it contacted the relevant jurisdiction to confirm whether there was a reasonable explanation for the change.
2.28 Figure 2.2 shows that, since the start of the NHRA, the number of NWAUs delivered each year on a national basis has consistently exceeded the estimates provided by the states. This has contributed to significant additional Australian Government ABF payments being made through the reconciliation process, particularly for 2015–16 ($512 million above original forecasts) and 2016–17 ($661 million above original forecasts). However, NWAU estimates for 2017–18 were much more accurate.
Figure 2.2: National estimated and actual National Weighted Activity Units
Source: ANAO analysis of Funding Body data.
ABF reconciliation process
2.29 State government health departments provide actual activity data to the Funding Body via the Pricing Authority twice annually — 31 March for the preceding July to December half year period, and 30 September for the full year. The Funding Body uses this to calculate whether any reconciliation adjustments should be made to Australian Government ABF payments.
2.30 Actual activity data is submitted through the Pricing Authority’s SDMS, and goes through the validation process referred to in paragraph 2.15 before being forwarded to the Funding Body. The Funding Body reviews the data to determine whether data characteristics (such as age profiles, indigenous status, location of services, types of services) indicate that the data is reasonable for use in the funding reconciliation and again contact relevant jurisdictions as considered necessary to gain an understanding of any major changes in underlying data. Funding Body records show that for the 2016–17 reconciliation, some outstanding data issues were discussed through formal meetings with state health departments and other stakeholders (including the Pricing Authority) and/or discussed at the Administrator’s jurisdictional advisory committee (JAC).56
2.31 Following the completion of the reconciliation process, including technical input from the Pricing Authority, the Funding Body prepares advice for the Administrator on any proposed retrospective adjustments to Australian Government ABF. The Administrator then provides detailed advice to the Treasurer (the decision-maker) on any recommended adjustment, including how this was calculated. Based solely on actual NWAUs delivered in 2016–17, the indicative additional Australian Government ABF payment was $791 million above what had been estimated for the relevant period by the states. However, the Funding Body applied a range of adjustments57 to reduce this to $307 million.58 The Administrator’s advice to the Treasurer noted that the states were critical of the methodology used in some of these adjustments59 but considered the adjustments were consistent with the ‘back-casting’60 provisions in the NHRA and that they were supported by the Minister for Health.
2.32 The Treasurer’s determination for 2016–17, incorporating the adjustment recommended by the Administrator, was made via legislative instrument registered on 2 October 2018. Following a regular meeting of the Council of Australian Governments (COAG) Health Ministers on 12 October 2018, state governments announced that they did not accept the adjustment determined by the Treasurer. The issue of public hospital funding and future reconciliation processes was discussed at the December 2018 COAG meeting but no change was made to the Treasurer’s determination regarding 2016–17 Australian Government funding.
Are effective processes in place between the Pricing Authority and Funding Body to communicate and manage shared risks regarding data received from the states?
Through mutual representation on each entity’s advisory committees, the Pricing Authority and Funding Body have awareness of, and communicate about, their respective data-related risk management approaches.
2.33 The Commonwealth Risk Management Policy (CRMP) defines shared risks as:
those risks extending beyond a single entity which require shared oversight and management. Accountability and responsibility for the management of shared risks must include any risks that extend across entities and may involve other sectors, community, industry or other jurisdictions.61
2.34 While the Pricing Authority and Funding Body are independent statutory entities, their respective roles in administering NHRA public hospital funding arrangements means that their operations impact on each other. Notably, changes to pricing methodology and hospital services classifications by the Pricing Authority can have significant impacts on the Funding Body’s calculation of Australian Government ABF payments. These impacts have contributed to delays in determining the final Australian Government reconciliation payments for 2015–16 (determined in April 2018) and 2016–17 (determined in October 2018).
2.35 The degree of explicit articulation of shared risk issues and their management varies between the two entities. A key risk identified on the registers of both the Pricing Authority and Funding Body is that data is of poor quality, not reliable or cannot be used. As previously mentioned, the entities have prepared and aligned three year data plans to assist in managing this broad risk.
2.36 The Funding Body recognises the Pricing Authority’s role with regard to data provision in its risk management documentation, in particular in its: external systemic risk framework62; enterprise risk register; and draft funding pool risk register.63 In some instances, specific Pricing Authority processes are recognised as a control to manage Funding Body risks such as the inaccurate calculation of Australian Government funding.
2.37 While the Pricing Authority does not do the same, its current risk management policy provides that communication and consultation processes are used to manage shared and cross-jurisdictional risks. Shared risks are not explicitly identified.
2.38 The ANAO’s review of Pricing Authority advisory committee and working group records indicate that there has been communication about, and consultation on, an extensive range of data-related matters, including:
- understanding the impacts on jurisdictions of collecting the required data;
- timelines to incorporate standardised data collection methodologies;
- processes that ensure data accuracy;
- preliminary results from hospitals; and
- data quality.
2.39 Transparency is provided through the Pricing Authority’s advisory processes. For example, the Pricing Authority’s review of activity data is tabled at its technical advisory committee (TAC)64 and jurisdictional advisory committee (JAC)65 meetings. The Funding Body and Department of Health also attend the Pricing Authority JAC meetings.
2.40 The Administrator’s policies articulate the reconciliation and calculation processes, including the required data specifications provided to external stakeholders. The jurisdictions are able to comment on these documents prior to their publication at the Administrator’s JAC. During the reconciliation process, the Funding Body works with the Pricing Authority to discuss issues relating to the activity data and the calculation process and confirm NWAU calculations have been applied correctly.
2.41 A cooperation and information exchange memorandum of understanding (MOU) was in place between the two entities up until 2015. As at November 2018, the Pricing Authority and Funding Body had commenced discussions about developing a new MOU.66
Are the effectiveness of data-related risk management strategies and practices periodically reviewed?
Both the Pricing Authority and Funding Body have undertaken or commenced reviews of their broader risk management frameworks in 2018. Both entities regularly review their risk registers and other relevant process documents such as data plans.
Pricing Authority
2.42 The Pricing Authority started a review of a broad range of its governance and security policies during the conduct of the audit in August 2018. The review included its risk management policy and strategic risk register.67 As at November 2018, the Pricing Authority’s risk appetite statement had been updated and communicated to all staff, however remaining risk management aspects of the review have yet to be completed.
2.43 Prior to the review, the risk management policy was last updated in August 2016. As at October 2018, the risk register reflects recent developments such as the introduction of the SDMS in 2017, organisational changes68 and policy/process changes.69
2.44 Key policies identified as treatments in the Pricing Authority’s strategic risk register such as its three year data plan and data compliance policy have been updated in the last two years, however the data quality assurance framework, which is relied on as a key risk treatment, has not been reviewed since May 2012. While the data quality assurance framework document includes procedures that are currently undertaken by Pricing Authority staff, the policy terminology is outdated. A review of the data quality assurance framework would be timely.
2.45 To address risks with data management processes, including the effectiveness of the full lifecycle of processes and controls from data submission to management, use and disposal, the Pricing Authority has established a rolling annual internal audit ‘to review the design and operating effectiveness of the controls in place at the … [Pricing Authority] … in relation to Data Governance Processes.’ There have been six recommendations arising from the first two data management internal audits (July 2015 and February 2017) and all recommendations have been reported as implemented to the audit risk and compliance committee within six months. A third audit in September 2017 resulted in no recommendations.
Funding Body
2.46 The most recent review of the Funding Body’s overarching risk framework and risk policy, which also looked at implementation issues, was completed in March 2018. Two key findings in the review were that:
- the Funding Body’s risk management documentation was detailed, comprehensive and aligned with the Commonwealth Risk Management Policy; and
- the complexity of the risk framework and other shortcomings meant that staff did not always use it to inform their own day-to-day risk management practices.
2.47 The Funding Body has implemented the recommendations in the review.70 Notably, the number of risks in the Funding Body’s risk register was reduced from 28 to 11. While the current version (July 2018) was updated to better document risk management controls, some controls such as the comparison of state provided estimates to LHN service level agreements (part of the process to calculate Australian Government ABF payments for the coming year) and the comfort gained by the use of the Pricing Authority’s SDMS portal, were not included in the register. The Funding Body should continue to improve its documentation of risks and their treatments, including that the documented controls reflect the underlying controls in place.
2.48 Following the Funding Body’s implementation of the 2018 risk framework and risk policy review, the ANAO examined the updated risk management documentation against the elements of the CRMP that were directly relevant to the scope of the audit. The only gap identified was that the enterprise level Risk Management Framework and Policy did not outline the Funding Body’s approach for measuring and reporting against risk management performance. The Funding Body has risk management KPIs in place, but as at November 2018 they required updating to reflect changes following the review, and it was unclear how the results of performance against these KPIs are reported on or otherwise used to inform ongoing risk management.
2.49 The Funding Body made improvements to data related processes in light of issues that came out of the 2015–16 reconciliation process. This included providing a more detailed Reconciliation Framework for 2016–17 and Funding Body staff identifying issues requiring further investigation in a more timely manner in 2016–17 than during the 2015–16 reconciliation.
2.50 In addition to changes made through formal review processes, Funding Body business units update their individual risk management plans yearly as part of their business planning processes. The Data Modelling, Policy and Analysis section, which primarily deals with state government data, updated their risk management plan a number of times over 2016 and 2017, including responding to comments from the Funding Body audit committee. The Funding Body also participates in the annual Comcover Risk Management Survey.71
Do the Pricing Authority and Funding Body monitor public hospital service and cost data to identify and analyse any significant changes and provide appropriate advice to decision makers?
The Pricing Authority and Funding Body monitor relevant data to identify significant changes and trends. States consider that the conduct of this work by the Funding Body is inconsistent with its key functions under the NHRA and the National Health Reform Act 2011.
In part due to lack of agreement between stakeholders about the use of relevant data, the Funding Body has not been able to accurately monitor the extent to which the Australian Government is making duplicate payments for public hospital services through the NHRA and Medicare Benefits Schedule (MBS). Preliminary work by the Funding Body does however indicate that potential duplicate payments may be in the range of $172 million to $332 million per year. The lack of agreement has also meant that the Department of Health has not had access to the matched public hospitals MBS data that would facilitate more comprehensive compliance and recovery action on potential duplicate MBS payments.
Pricing Authority
2.51 During the Pricing Authority’s data quality review process, cost and activity data is assessed for growth when compared with the previous year’s data, and outliers and anomalies are identified.72 The initial analysis and monitoring of changes in the data is conducted at the hospital level and jurisdiction level using the quality assurance reports73 shared with Pricing Authority teams and the states.
2.52 After each six monthly submission of activity data by the states, and following completion of data quality review processes, the Pricing Authority analyses the data and provides a report on trends and significant drivers of services growth for the whole data set. The resulting data reports are presented for review by all jurisdictions through the Pricing Authority’s technical advisory committee and jurisdictional advisory committee, providing an opportunity for identification of trends or errors in reporting.74
2.53 Following this, the analysis is provided to Pricing Authority Board meetings. In response to a significant growth in Australian Government funding in 2015–16, a detailed analysis of activity data has also been provided to the Board for both year-on-year and over the life of the NHRA.75 As a result of this analysis, the Board has directed that Pricing Authority staff undertake further work with the states to understand the drivers of growth and also with the Funding Body to determine the best treatment of newly reported activity in the calculation of efficient growth.
2.54 Cost data analysis reports are publicly released annually at the end of each round of cost data collected. The reports are presented to the Pricing Authority cost data committee and jurisdictional advisory committee for comment before tabling at Board meetings.76 Stakeholders use the cost data reports for a range of purposes including benchmarking and contractual arrangements. The cost data reports summarise the: number of hospitals/local hospital networks that provided data, total expenditure by data stream; average costs; and average cost per weighted separation. The reports can also include information from the data quality statements supplied by each state to highlight key aspects that can influence a jurisdictions results.
2.55 The Pricing Authority is currently expanding its capability for data analysis and trends reporting, and recently introduced tools such as dashboards for reporting to decision makers. Additionally, the Pricing Authority’s 2018–19 plan requires that activity data be submitted quarterly, rather than six-monthly.
Funding Body
2.56 The Funding Body monitors activity data received from the states as part of the reconciliation process, including reasonableness checks on the distribution of data and NWAU outcomes by state, local hospital network and service category. Statements of assurance on activity data provided by the states are also used by the Funding Body to identify issues within the data sets. As referred to in paragraph 2.30, issues identified through this process are discussed with states and the Pricing Authority, and outcomes formally presented at the Administrator’s jurisdictional advisory committee.
2.57 The Funding Body has also undertaken additional analysis at the request of the Australian Government Treasurer in response to the significant growth reflected in the 2015–16 reconciliation process.77 The report on this analysis, released to jurisdictions in June 2017, attributed the major underlying drivers of this growth to NWAU increases of 6.8 per cent, flowing from both an increased number of services delivered plus changes to the case mix. Price increases accounted for another 3.7 per cent of ABF growth. This reporting led to further referrals to the Pricing Authority to address a number of issues that arose in the 2015–16 data.78 The conclusion presented to jurisdictions in February 2018 was that there were issues in relation to pricing, counting methodology and classification. As a result, the final 2015–16 reconciliation payment was reduced by $123 million79 compared to from what had originally been calculated by the Funding Body and Administrator.
2.58 In December 2017, the Funding Body commissioned further work on the changes in activity data from 2015–16 to 2016–17. Included in this work was a review of outliers and anomalies contained within the state data sets, the reasonableness and proportionality of state data and insight into the underlying drivers of activity, and Australian Government contribution growth and changes between 2015–16 and 2016–17. The key points from this analysis were presented to state government officials and other stakeholders in May 2018. Notably, the analysis concluded that a change in how some hospital services were classified under the Pricing Authority’s national standards system resulted in an unexpected increase in the number of NWAUs delivered which then affected funding growth.80 The impact of this change was addressed by the Pricing Authority applying a ‘back-casting’ adjustment to the previous year’s (2015–16) activity data in order to account for changes in classifications.81 This enabled consistency between years when calculating the Australian Government’s efficient growth between 2015–16 and 2016–17 in accordance with clause A40 of the NHRA. The Administrator’s advice to the Treasurer provided information on the treatment of the issue, including the views of the states. As referred to in paragraph 2.32, state governments have challenged the Treasurer’s determination of 2016–17 reconciliation payments.
2.59 Broader monitoring and analysis of data by the Funding Body has been prevented by concerns from jurisdictions around its mandate to be able to perform such work. The analysis report on 2015–16 activity data that was requested by the Treasurer saw a jurisdiction obtaining legal advice that the analysis within the report was outside of the Administrator’s authority, and that the Treasurer’s request should have been directed to the Pricing Authority.
2.60 The states have also previously expressed concerns with the Funding Body’s capacity to undertake analysis and provide strategic advice to governments on linked hospital activity and MBS/PBS data sets.82 The states indicated that they consider such work could ‘potentially undermine its role of ensuring equity, accuracy and integrity in the distribution of Commonwealth funding between states’. A lack of definition around the mandate for the Funding Body to perform analysis has restricted its ability to undertake detailed analysis of the datasets it receives and to provide advice to stakeholders.
Recommendation no.1
2.61 The Department of Health:
- work with relevant state government entities to reach agreement on the appropriate data monitoring analysis roles for the Independent Hospital Pricing Authority and National Health Funding Body; and
- incorporate the agreed roles into the revised National Health Reform Agreement currently under negotiation.
Department of Health response: Agreed.
2.62 The department agrees it is important that the Independent Hospital Pricing Authority and National Health Funding Body undertake data matching and analysis in order to ensure the accuracy and integrity of Commonwealth funding. The department will seek to reach agreement with the states and territories on these roles and incorporate them within the new National Health Reform Agreement.
Data Matching under A6 of the Agreement.
2.63 The NHRA specifies that the Australian Government will not fund a hospital service if the service is funded through any other Australian Government program, including the Medicare Benefits Schedule (MBS)83 and the Pharmaceutical Benefits Scheme (PBS).84 There are similar provisions in the MBS legislation to prevent double funding.
2.64 The NHRA does not specify a mechanism to prevent and/or recover Australian Government duplicate funding for services. In 2013, the Funding Body developed data matching business rules to identify situations where services are funded by both NHRA and MBS sources, and applied these to deterministically linked85 data using Medicare PINs (de-identified Medicare numbers).86 This data matching process identified potential situations of duplicate funding yet did not result in adjustments to Australian Government funding as further investigation was required to confirm a duplicate payment actually occurred. In addition, the states requested that the Australian Government undertake MBS compliance activities to prevent double funding and recover payments from health providers, rather than adjusting NHRA funding.
2.65 Since 2014 Australian and state government ministers and officials have discussed options to improve data matching under the NHRA provisions. In-principle agreement was reached in August 2016 for the Department of Health (Health) to conduct a data matching pilot for MBS compliance purposes that would require access to, and the use of, the matched data sets held by the Funding Body. Concerns from the states about the scope of the pilot and the end use of the data sets by Health resulted in delays, with the issue being referred to COAG health ministers in April 2018. In March 2018, Health also sought advice from the Australian Government Solicitor about other options for obtaining state public hospital activity data for matching with MBS/PBS data for compliance purposes. These options were not pursued at that time.
2.66 Following agreement by Ministers in April 2018 to proceed with the data matching work, the Funding Body reviewed and updated the business rules developed in 2013 and applied these rules to data from 2014–15 to 2016–17. From this work, Table 2.5 shows the estimates of MBS benefits paid that have been identified through data-matching, noting that these matches have not been investigated further to confirm that duplicate MBS/NHRA funding actually occurred.87
2.67 The difference in the amounts in the two rows in Table 2.5 relate to data-related difficulties in establishing whether a MBS claim relating to medical service provided on the day of a patient’s hospital admission or discharge was actually provided by the hospital rather than another person or facility. Excluding all MBS payments relating to admission and discharge days in 2016–17 gives a lower estimate of $172 million of potential duplicate payments. If admission and discharge days are counted, the estimate rises to $332 million.
Table 2.5: Estimates of potential Australian Government duplicate payments for public hospital services
|
|
2014–15 |
2015–16 |
2016–17 |
|
Total potential matched MBS payments paid excluding any MBS payment relating to day of admission and separation/discharge |
$122m |
$130m |
$172m |
|
Total potential matched MBS payments paid including any MBS payment relating to day of admission and separation/discharge |
$249m |
$272m |
$332m |
Note: Because of technical difficulties regarding matching of non-admitted care records, the above amounts likely underestimate potential duplicate payments for non-admitted care.
Source: ANAO analysis of Funding Body documentation.
2.68 As at November 2018 the data had not yet been provided to Health, in part due to ongoing concerns from the states regarding the scope of the pilot and intended use of the data. Health advised the ANAO that:
The timeframe for the release of data to the Commonwealth is a decision for the Administrator. However the Department hopes to be in a position to act on outcomes from the data matching pilot mid–2019.88
2.69 In addition to ‘business as usual’ MBS compliance activities, in 2012 Health was provided with $1.8 million to implement the ‘Fraud prevention and compliance — Improve billing practices within public hospitals’ budget measure over a four year period. This measure was originally aimed to address inappropriate billing by hospital emergency departments for pathology and diagnostic imaging services, and was expected to provide savings of $24.7 million. In 2014 the scope was expanded to include education and compliance for all public hospital services. Health estimates $22.5 million in savings were achieved over 2012 to 2016, with 98 per cent of these savings a result of behavioural change in providers.89 In 2018, Health developed a new ‘behavioural change’ evaluation methodology to assist in measuring the impact of MBS compliance activity. Health does not currently report on the impact of its ongoing MBS compliance work on possible inappropriate MBS claiming from providers working in the public hospital sector.
2.70 An April 2017 report by Health on the outcomes of the 2012 budget measure included eight recommendations to further enhance Medicare program integrity in public hospitals and address compliance barriers. To date these recommendations have not been finalised. An amendment made to the Health Insurance Act 1973 introduces a shared debt recovery scheme from 1 July 2019, so that where contractual or other arrangements exist between a practitioner and an employer or corporate entity, both may be held responsible for the repayment of the debt. However, the terminology in the Business Rules for the NHRA regarding the use of Medicare in public hospitals has not been amended for clarity and consistency with the Health Insurance Act 1973.
2.71 The amounts outlined in Table 2.5 show potential duplicate MBS and NHR payments are increasing every year. Given the lack of an effective mechanism to prevent their occurrence, or achieve their recovery, these payments represent a significant inefficiency in the Australian Government funding for some public hospital health services. The payments are also contrary to the NHRA. The draft new funding agreement does contain additional clauses related to MBS compliance activities, which if adopted in the final agreement, would facilitate Health’s ongoing access to the necessary data to underpin more comprehensive compliance activities regarding public hospital services.
Recommendation no.2
2.72 The Department of Health:
- identify and prevent potential duplicate payments, including Medicare Benefits Schedule payments, by the Australian Government for public hospital services; and
- identify and recover past duplicate payments to the maximum extent permitted by law.
Department of Health response: Agreed.
2.73 Medicare Benefits Schedule compliance activities, including for providers rendering services in hospitals, is an existing function of the department. The department will continue to work with the states and territories and the independent agencies to identify, prevent and recover duplicate payments for public hospital services under MBS compliance, including where the service is identified through agreed data matching arrangements.
3. Reporting
Areas examined
The ANAO examined how public hospitals funding, service and performance levels are reported.
Conclusion
There is public reporting by Australian Government entities on public hospital funding provided under National Health Reform Agreement (NHRA) arrangements. Transparency regarding the fulfilment of state governments funding commitments could be improved. Estimates of the number of public hospital services delivered by individual Local Hospital Networks are reported, noting that the actual number of services are only reported at the aggregated national level. The absence of the originally intended Local Hospital Network level performance reporting has weakened the reporting framework’s ability to achieve performance improvement objectives under the NHRA.
Public reporting shows mixed progress against NHRA hospital performance objectives. There have been some positive trends regarding hospital efficiency. On patient access, emergency department performance has declined slightly, but for elective surgery there have been improvements in some indicators. There has been no notable progress on improving the safety and quality of clinical care, although only a limited range of performance indicators are currently reported on.
Areas for improvement
The ANAO has made a recommendation to improve reporting on whether all states are meeting their NHRA obligation to maintain public hospital funding levels.
Is there a national framework in place for public hospital performance reporting?
The Performance and Accountability Framework established under the National Health Reform Agreement (NHRA) was only partially implemented. Notably, the intended Local Hospital Network level reporting never occurred, weakening the framework’s ability to drive improved performance and achieve the associated objectives under the NHRA. Some public reporting against a limited set of performance indicators has occurred. Work has commenced to consolidate the existing multiple health reporting frameworks and develop a definitive set of performance indicators for public reporting.
3.1 An important element of the NHRA agreed by the Council of Australian Governments (COAG) in 2011 was the development of ‘clear and transparent performance reporting’ in relation to health and hospital services through the establishment of a Performance and Accountability Framework. The Performance and Accountability Framework was intended to underpin public reporting across three broad objectives:
- equity (patient access);
- effectiveness (safety and quality, and patient experience); and
- efficiency in the delivery of services.
3.2 Reporting was to be undertaken by the National Health Performance Authority (Performance Authority), established under the National Health Reform Act 2011.
3.3 The Performance Authority was to publicly report on the performance of Local Hospital Networks (LHNs), and the public hospitals within them, against 17 indicators across the above three objectives. The NHRA also provided that the Performance Authority would use the reporting arrangements to identify:
- high-performing Local Hospital Networks … and hospitals … [to] … facilitate sharing of innovative and effective practices; and
- poorly performing Local Hospital Networks … to assist with performance management activities.
3.4 The Performance Authority would provide advice to the Australian and state governments on identified poor performing LHNs, with the states agreeing to remediate any ongoing poor performance. This LHN-level reporting system was never implemented as governments did not reach agreement on a process to identify poor performing LHNs.
3.5 In 2016, the Performance Authority was abolished, with reporting functions transferred to the Australian Institute of Health and Welfare (AIHW) and the Australian Commission on Safety and Quality in Healthcare (Safety and Quality Commission). As at November 2018, the AIHW ‘MyHospitals’ website reports on six of the 17 Performance and Accountability Framework hospital indicators.90 Specifically:
- healthcare associated staphylococcus aureus infections (these can cause can cause serious complications such as bloodstream infections, pneumonia, or bone and joint infections);
- Emergency Department waiting times by urgency category;
- percentage of emergency department patients transferred to a ward or discharged within four hours, by triage category;
- elective surgery patient waiting times by urgency category;
- average length of stay; and
- cost per average admitted hospital service.
3.6 A review of Australia’s health system performance information and reporting frameworks was commissioned by the Australian Health Ministers’ Advisory Council in 2016–17. The review found that the purpose and audiences of the frameworks were unclear and that there were gaps in the current range of performance indicators, including too few indicators measuring the patient’s experience or clinical outcomes. In September 2017, the COAG Health Ministers Council agreed to combine the Performance and Accountability Framework with the National Health Performance Framework91 to form the Australian Health Performance Framework. The Australian Health Performance Framework is intended to:
provide a single, enduring and flexible vehicle to support system-wide reporting on Australia’s health and health care performance, to support the assessment and evaluation of value and sustainability, and to inform the identification of priorities for improvement and development.
3.7 In July 2018, agreement was reached between all jurisdictions to develop a consolidated set of indicators under the Australian Health Performance Framework for future public reporting. This work, to undertaken by a cross-jurisdiction working group, co-chaired by Department of Health (Health) and the AIHW, is due to be completed in the first half of 2019. While the Australian Health Performance Framework does not explicitly mandate LHN level performance reporting, it is intended that the data collected under the framework will enable ‘tiered reporting’, including at the LHN level.
Does existing public reporting provide transparent information about the level of Australian Government funding of public hospitals to states and the local hospital networks within them?
Public reporting, mainly by the Administrator of the National Health Funding Pool, provides transparent information on Australian Government public hospital funding services down to the Local Hospital Network level. However, public reporting does not provide clarity on whether state governments are fulfilling their commitment in the NHRA to maintain their own 2017–18 funding of public hospital services at 2015–16 levels.
3.8 Public reporting by the Administrator provides detailed information on Australian and state government National Health Reform (NHR) funding, including the amounts received by individual LHNs.
3.9 The Funding Body receives data from the states that it uses to create the Administrator’s reports. For Australian Government block funding, the Funding Body relies on advice from the states that relevant amounts have been transferred from state managed funds to LHNs. For Australian Government activity based funding (ABF) amounts, the relevant amounts are checked back to the ‘Commonwealth Contribution Model’ entitlement for each LHN. Entitlement amounts are uploaded to an Australian Government Department of Human Services hosted payment system, to assist in allocating the calculated entitlement to the relevant LHNs when payments are scheduled. Under the NHRA, amounts can be paid directly to LHNs or third parties on the behalf of an LHN or a number of LHNs within a State. In all but one jurisdiction, Australian Government ABF amounts (the Commonwealth Contribution Model entitlement) were paid directly to the individual LHNs. The exception was NSW where in 2017–18 $10.09 billion of combined Australian Government and New South Wales (NSW) government funding92 was allocated through the NSW Ministry of Health under a shared services arrangement. The Funding Body relies on advice from NSW regarding the subsequent transfer of funds on to the relevant LHNs.93
3.10 NHR funding by all governments represents 82.4 per cent of estimated total funding of public hospital services.94 Public reporting by the AIHW provides information on the level of funding outside NHRA arrangements, including government and non-government funding associated with private patients.
3.11 As shown in Figure 3.1, Australian Government NHR funding has increased from $13.13 billion in 2012–13 (the first year of NHRA arrangements) to $19.94 billion in 2017–18, an overall increase of 51.9 per cent over five years.95 Total state government NHR funding has increased by 16.5 per cent over the same period.96
Figure 3.1: National Health Reform funding 2012–13 to 2017–18
Note: Funding refers to amounts actually paid in the relevant year. State funding has been adjusted for cross border payments.
Source: ANAO analysis of public reporting by Administrator.
3.12 As at November 2018, Australian Government NHR funding payable in 2018–19 is estimated to be $21.42 billion.97 From the implementation of the NHRA Addendum in 2017–18, annual Australian Government funding growth is limited by the operation of the 6.5 per cent funding cap.98 As at November 2018, total Australian Government funding growth for 2017–18 hospital services99 is estimated to be under the cap at around 4.2 per cent, mainly due to a slight decline in the number of NWAUs delivered by public hospitals.100
3.13 Figure 3.2 shows the proportion of total NHR funding provided by the Australian Government to each state in 2017–18 as compared to 2012–13. Consistent with the intent of the NHRA, the share of NHR funding provided by the Australian Government has increased nationally from 36.5 per cent in 2012–13 to 42.9 per cent in 2017–18. Figure 3.2 also shows that the share of NHR funding provided by the Australian Government varies between jurisdictions. In part, these variations reflect that initial NHR funding levels were based on the previous block funding arrangements outlined in Chapter 1. Fluctuations from year to year in the Australian Government’s share of NHR funding reflects changes in public hospital funding levels by individual states, or potentially because states are funding NHR eligible services outside of NHRA arrangements.101
Figure 3.2: Australian and State Government funding as a proportion of total National Health Reform funding 2012–13 and 2017–18
Note: Analysis is based on amounts actually paid in the relevant year. State funding has been adjusted for cross border payments
Source: ANAO analysis of public reporting by Administrator.
3.14 The NHRA provides that state governments agree to maintain their own 2017–18 to 2019–20 funding of public hospital services to at least at 2015–16 levels. This provision does not specify that funding must be directed through NHR arrangements, nor does it outline how compliance will be assessed. According to public reporting by the Administrator, the level of NHR public hospital funding by the Western Australian Government has decreased from $3.18 billion in 2015–16 to $2.36 billion in 2017–18. AIHW reporting indicates that total Western Australian Government public hospital funding (including funding outside the NHRA) has decreased from $2.98 billion in 2015–16 to $2.73 billion in 2016–17, with 2017–18 figures not available as at November 2018.
Recommendation no.3
3.15 The Department of Health seek the agreement of states to implement reporting arrangements that provide transparency on whether state governments are maintaining public hospital services funding levels in accordance with National Health Reform Agreement obligations.
Department of Health response: Agreed.
3.16 The department agrees there is benefit in reporting requirements to ensure transparency over jurisdictional maintenance of effort in funding public hospital services. The introduction of these requirements needs to be negotiated between the Australian Government and state and territory governments as part of the new National Health Reform Agreement.
3.17 Under the NHRA, hospital funding is to be provided by the Australian and state governments using ABF where practicable and block funding in other cases. Figure 3.3 shows the relative proportions of total NHR funding provided via ABF. On a national basis, ABF has risen from 73.3 per cent in 2012–13 to 84.4 per cent in 2017–18.
Figure 3.3: National Health Reform funding type 2012–13 and 2017–18
Note: Analysis is based on amounts actually paid in the relevant year. State funding has been adjusted for cross border payments. Cross border payments are counted as ABF.
Source: ANAO analysis of public reporting by Administrator.
Does the existing public reporting provide transparent information about the volume of services delivered by local hospital networks that receive Australian Government funding?
Public reporting by the Administrator of the National Health Funding Pool provides transparent information on the forecasted volume of public hospital funding services expected to be delivered at the Local Hospital Network level. The Administrator also reports the actual number of services delivered, but only at the aggregated national level rather than at the local level.
3.18 The volume of services (expressed as NWAUs) forecast to be provided annually by each state and LHN is publicly reported by the Administrator on a monthly basis. The actual volume of services delivered by each LHN is provided by the states to the Funding Body but is publicly reported only at the national level on an annual basis. Total NWAUs have increased from 5.904 million in 2012–13 to 8.413 million102 in 2017–18, an overall increase of 42.5 per cent over five years. As referenced in Chapter 2, the Pricing Authority and Funding Body carry out a range of data validation and quality processes to mitigate the risk of inaccuracies in the service activity data supplied to them by the states. Figure 3.4 shows the growth in the number of NWAUs delivered in each jurisdiction103 between 2012–13 and 2017–18.
Figure 3.4: Number of National Weighted Activity Units delivered 2012–13 and 2017–18
Source: ANAO analysis of public reporting by Administrator and Funding Body documentation.
3.19 ANAO analysis shows variations between the jurisdictions on the volume of NWAUs delivered per head of population. As shown in Figure 3.5, in 2016–17, while most jurisdictions delivered around 300 to 400 per 1000 people, in the Northern Territory the figure was over 600. This is likely connected with the high proportion of Indigenous Australians in the Northern Territory combined with the fact that Indigenous Australians in the territory receive five times the number of episodes of hospital care per head of population as non-Indigenous persons.
Figure 3.5: Number of National Weighted Activity Units delivered per 1000 people 2012–13 and 2017–18
Source: ANAO analysis of public reporting by Administrator, Funding Body documentation and Australian Bureau of Statistics data.
3.20 Jurisdictions provide the Funding Body with estimates of the number of NWAUs they anticipate their respective LHNs will deliver in the upcoming year. This is a key input for determining how much the Australian Government will contribute. Significant under estimations in 2015–16 and 2016–17 have contributed to the Australian Government being required to make additional NHR funding payments following the reconciliation process. For 2016–17, the additional Australian Government NHR reconciliation payment was $661 million in total across the jurisdictions.104
Does the existing public reporting provide transparent information about progress towards the hospital-related policy objectives of the National Health Reform Agreement?
Existing public reporting provides a reasonable level of information about the mixed progress towards the hospital-related policy objectives under the NHRA of increased efficiency, patient access and safety and quality of clinical care. Reporting on efficiency suggests a modest improvement based on the stability of the national efficient price and improvements in the time a patient spends in hospital compared to expectations. Reporting on patient access suggests a slight decrease in performance against emergency department indicators, contrasted by a slight improvement in elective surgery related indicators. There has been no notable progress on improving the safety and quality of clinical care, although only a limited range of performance indicators are currently reported on.
The current development of a definitive set of performance indicators under the 2017 Australian Health Performance Framework should assist with the transparency and reliability of future reporting.
3.21 In addition to increasing the proportion of public hospital costs funded by the Australian Government, the NHRA objectives include improving:
- public hospital efficiency;
- patient access to hospital services; and
- standards of clinical care.
3.22 Public reporting by the Administrator, the Productivity Commission, the AIHW and the Safety and Quality Commission provides information on a range of indicators connected to the above policy objectives.
3.23 There are no nationally agreed performance targets in relation to these objectives. Targets for patient access were in place under the National Partnership Agreement on Improving Public Services. However, the Australian Government terminated this agreement with effect from July 2015.105
Efficiency
3.24 ‘Efficiency’ is not defined in the NHRA. However, the average cost per admitted acute weighted separation106 is commonly reported as an indicator of efficiency107 in the Productivity Commission’s annual Report on Government Services.108 Cost per NWAU measure can also be indicative of efficiency, as it is derived from the weighted average cost of separations, but with a range of costs removed and various adjustments made to account for cost difference in delivering the service (such as remoteness). As shown in Figure 3.6, the rate of growth of both indicators109 has slowed since the commencement of the NHRA in 2012–13.
Figure 3.6: Cost of public hospital services 2007–2008 to 2018–19
Source: ANAO analysis of Funding Body, Productivity Commission and Pricing Authority data.
3.25 Change in the national efficient price is also relevant as a more up to date indicator of efficiency. As Figure 3.6 shows, it has remained reasonably flat for most of the period where the NHRA has applied. Notably, the cost indexation factor used in national efficient price calculations has declined from 5.1 per cent per annum in the initial (2012–13) national efficient price to 1.6 per cent in the most recent period (2018–19). Given this indexation factor is below the forecast underlying Australian inflation rate of two per cent in 2018–19, this may indicate a modest improvement in efficiency. The Pricing Authority’s forecasts out to 2021–22 project an average annual increase in the national efficient price of 1.1 per cent.
3.26 ANAO analysis in Figure 3.7 shows that, from 2012–13 to 2017–18, the number of NWAUs delivered per $1000 of combined Australian Government and state NHR funding has increased on a national basis from 0.16 to 0.18 (a 12.5 per cent increase).110 On a jurisdictional basis, the number of NWAUs delivered per $1000 of total NHR funding in 2017–18 varies between 0.12 in the Northern Territory to 0.20 in New South Wales.
Figure 3.7: Number of National Weighted Activity Units delivered per $1000 of National Health Reform funding 2012–13 and 2017–18
Note: Analysis is based on amounts actually paid in the relevant year.
Source: ANAO analysis of public reporting by Administrator.
3.27 The time a patient spends in hospital compared to expectations based on their medical condition can also be used as an efficiency indicator. While changes to the patient data included in this measure limits the direct comparability of year on year figures, this ‘relative stay index’ measure indicates a steady improvement (an average of 3.1 per cent a year) on a national basis in efficiency in public hospitals since the commencement of the NHRA.
Patient access
3.28 Performance regarding patient access to public hospital services is currently measured by both emergency department and elective surgery waiting times.
3.29 Patients attending emergency departments are triaged into five urgency categories, each of which have a prescribed time in which they should start to receive clinical care. Specifically:
- resuscitation (immediate);
- emergency (within 10 minutes);
- urgent (within 30 minutes);
- semi-urgent (within 60 minutes); and
- non-urgent: (within 120 minutes).
3.30 Figure 3.8 shows the proportion of patients seen within the prescribed time for their urgency category in both 2012–13 and 2017–18. On a national basis, performance has dropped slightly from 73 per cent to 72 per cent. Reports by some state Auditors-General in recent years have highlighted data quality and governance issues in relation to emergency department performance reporting.111
Figure 3.8: Proportion of emergency department patients seen within recommended time 2012–13 and 2017–18
Source: AIHW data.
3.31 In relation to elective surgery, at the time a person is being placed on the public hospital elective surgery waiting list112 a clinical assessment is made of the urgency with which the person should undergo the relevant surgical procedure. This ranges from 30 days for the most urgent category, to one year for the least urgent. Figure 3.9 shows that, in all but one jurisdiction, the proportion of surgery conducted within recommended times has increased over the life of the NHRA.113,114
Figure 3.9: Proportion of elective surgery patients operated-on within the recommended time 2012 and 2017–18
Note: 2012 data was published on a calendar year basis. Subsequent data was published on financial year basis.
Source: AIHW data.
Safety and quality of clinical care
3.32 A range of safety and quality indicators have been publicly reported in recent years. Other measures such as mortality indicators have been developed, but are not nationally reported, largely due to the inconsistent coding of data between states. Consolidation of safety and quality indicators is within the scope of the previously mentioned Australian Health Performance Framework development work, including aligning safety and quality reporting between public and private hospitals.
3.33 Improved data collection and reporting of safety and quality is also being driven by changes introduced through the 2017 Addendum to integrate safety and quality into NHR funding. From 2017, the Australian Government will not fund a hospital service that was provided to a patient during which a sentinel event occurs. From 2018, funding will also be reduced for a service in which a hospital acquired-complication occurs. As at November 2018, the timetable for introducing reduced funding for avoidable readmissions had yet to be finalised.
3.34 Adverse events are incidents in which harm resulted to a person receiving healthcare. They include adverse effects of drugs, injuries that occur during care and conditions that occur following procedures such as infections and bleeding. According to the Pricing Authority, estimates in Australian and internal costing studies indicated that adverse events constitute between 12.0 and 16.5 per cent of total hospital costs. As shown in Figure 3.10, the rate of occurrence of adverse events in public hospitals has not changed significantly (6.5 to 6.6 events per 100 separations) between 2012–13 and 2016–17.
Figure 3.10: Separations with an adverse event per 100 separations in public hospitals 2011–12 to 2016–17
Source: Productivity Commission data.
3.35 Figure 3.11 shows the number of sentinel events in public hospitals between 2011–12 and 2015–16.
Figure 3.11: Number of sentinel events in public hospitals 2011–12 to 2015–16
Source: Productivity Commission data.
3.36 Public reporting on unplanned/avoidable readmissions is limited, with the AIHW reporting relating to selected surgical procedures only, as shown in Figure 3.12. Four out of the seven reported procedures show increases in unplanned readmission rates. In 2018, the Safety and Quality Commission developed an agreed list of conditions considered to be avoidable hospital readmissions and associated condition-specific time intervals.115
Figure 3.12: Selected unplanned public hospital readmissions rates per 1000 separations, by surgical procedure 2011–12 to 2016–17
Source: ANAO analysis of AIHW data.
Use of data to inform Australian Government public hospital funding policy objectives
3.37 As covered in paragraphs 3.21–3.36, there is extensive public reporting of indicators relevant to NHRA hospital-related policy objectives. As the lead Australian Government entity for hospital funding policy, the Department of Health has provided advice to the Minister for Health regarding some of the reported results. The department advised the ANAO that it sought to achieve:
efficiency and improved outcomes in the [hospital] system largely in the context of negotiating the NHRAs, with the implementation of such reforms taking place over the course of the agreement. Examples of this include the department drawing on data to identify adverse impacts on access and system sustainability as a result of an increase in the numbers of private patients in public hospitals and to press for reform in this area.
3.38 Significant changes were made to the NHRA through the 2017 Addendum. Changes addressed the high growth rates in Australian Government funding (through the introduction of the 6.5 per cent funding cap) reducing health costs more generally (through various measures to decrease the avoidable demand for public hospital services) and improving standards of clinical care (including by incorporating quality and safety factors into how future Australian Government funding was to be calculated). Health has also chaired a working group to develop a National Clinical Quality Registry116 Strategy. The strategy seeks to achieve the better use of data at the clinical level, including in public hospitals, to promote NHRA-related objectives of improved efficiency, patient access and standards of clinical care.
Appendices
Appendix 1 Entity responses
Formal responses received by ANAO following circulation of the draft report are reproduced in Appendix 1.
Responses were received from:
Department of Health

Independent Hospital Pricing Authority
National Health Funding Body

Appendix 2 State audit reports of public hospital activity and performance data
|
Jurisdiction |
Year |
Report focus |
Key findings |
|
New South Wales |
2015 |
Activity based funding data quality |
Data quality governance for ABF is adequate, although there are some areas for improvement. All Local Health Districts117 use a standardised process to cost the services they provided, and there is a new mandatory internal audit program focused on the costing process that has been rolled out to all Local Health Districts. NSW Health has developed, but is yet to implement, a comprehensive data quality framework. There are workforce related issues that may impact on data quality for ABF in NSW. There are reported issues with maintaining the capacity of the clinical coding workforce. |
|
Victoria |
2016 |
Effectiveness and efficiency of emergency care |
The lack of segregation between data entry and data validation in many health services increases the risk of data error and manipulation. This has been identified in audits of the health department since 2010. |
|
Victoria |
2017 |
Public hospital operating theatre efficiency |
Operating theatre data is not being collected consistently by health services, with resulting impacts on decision making, evaluation and benchmarking. |
|
Queensland |
2014–15 |
Emergency department performance reporting |
Controls over emergency department data have been, and remain, weak or absent. The quality of data reported relies primarily on the integrity and diligence of individuals. The introduction of data integrity controls to reduce errors and prevent deliberate data manipulation have not been satisfactorily addressed. |
|
Western Australia |
2017 |
Accuracy of WA Health’s Activity Based Funding data |
Testing of patient activity records found an error rate of 5.2 per cent. A much higher error rate was found in a few elements of the suite of mental health information. Weaknesses in processes and controls for collecting and reporting activity data were identified, in particular there is no data quality framework in place covering data submissions. Data quality controls are inconsistent and weaknesses increase the risk of errors or unauthorised changes. Processes and controls for the non-admitted data collection needs the most improvement. |
|
South Australia |
2015 |
Hospital activity data integrity review |
ABF data integrity controls are operating effectively for admitted and emergency department patient activity data. Limited testing of non-admitted activity data showed controls for the components tested were effective. Areas requiring remedial action include:
|
|
Australian Capital Territory |
2015–16 |
Integrity of data in the Health Directorate |
The integrity of ABF data for admitted patient and emergency department services is adequate. Non-admitted patient data integrity data is inadequate. Errors detected by the Audit Office in the last six months could have resulted in around $2 to $3 million being under-claimed. The Health Directorate’s management of ABF data is generally effective, with the exception of non-admitted patient data. There are opportunities for improvement. |
Appendix 3 Performance and Accountability Framework: hospital-related indicators
|
Indictor |
Sub indicator |
Is there current national public reporting? |
|
Effectiveness — Safety and quality |
Hospital Standardised Mortality Ratio |
No |
|
Death in low-mortality Diagnostic Related Groups |
No |
|
|
In hospital mortality rates for select conditions |
No |
|
|
Unplanned hospital readmission rates for patients discharged following management of select conditions |
No |
|
|
Healthcare-associated Staphylococcus aureus infections |
Yes |
|
|
Healthcare-associated Clostridium difficile infections |
No |
|
|
Rate of community follow up within the first seven days of discharge from a psychiatric admission |
No |
|
|
Effectiveness — patient experience |
Measures of the patient experience with hospital services |
No |
|
Equity and effectiveness — patient access |
Access to services by type of service compared to need |
No |
|
Emergency Department waiting times by urgency category |
Yes |
|
|
Percentage of Emergency Department patients transferred to a ward or discharged within four hours, by triage category |
Yes |
|
|
Elective surgery patient waiting times by urgency category |
Yes |
|
|
Cancer care pathway — waiting times for cancer care |
No (current reporting is 2012–13 year) |
|
|
Efficiency |
Relative Stay Index for multi-day stay patients |
Yes |
|
Day of surgery admission rates for non-emergency multi-day stay patients |
No |
|
|
Cost per weighted separation and total case weighted separations |
Yes (but 2018 reporting is based on 2014–15 year costs) |
|
|
Financial performance against activity funded budget (annual operating result) |
No |
|
Source: ANAO Analysis of the National Health Reform Performance and Accountability Framework and performance indicator reporting in AIHW My Hospitals website.
Appendix 4 Costs in individual jurisdictions
Figure A.1: Average cost per jurisdiction for admitted acute weighted separation (2015–16)
Source: ANAO analysis of Productivity Commission data.
1. Average costs can also vary considerably between comparable hospitals. According to a November 2018 AIHW report, cost per NWAU in 2014–15 at individual large metropolitan public hospitals included in the AIHW study ranged from $3500 to $6300, with an average of $4460. The average 2014–15 cost of the all 27 hospitals in the AIHW study was $4860, an inflation adjusted decrease of 1 per cent from 2012–13.
Footnotes
1 Consistent with the terminology in the National Health Reform Agreement, ‘state’ includes references to the Northern Territory and the Australian Capital Territory.
2 Funding can also occur outside of the NHRA through Medicare Benefits Schedule (MBS) payments. The MBS is a program under which the Australian Government partly or fully subsides a range of medical and hospital services.
3 See paragraphs 1.21–1.22 for more information about the National Health Funding Pool.
4 A more comprehensive summary of entity roles and responsibilities is in Table 1.2.
5 Auditor-General Report No. 18 2017–18 Monitoring the Impact of Australian School Funding.
6 This compares to 657 private hospitals, providing 34,300 beds. While most people treated in public hospitals are admitted as public patients, an increasing proportion are admitted as private patients — that is, where private health insurance covers at least some of the costs. In 2016–17, private patients represented 13.8 per cent (or about 911,700) of public hospital separations, up from 8.2 per cent in 2006–07. ‘Separations’ is the standard term to describe the total number of episodes of care that a hospital provides over a set period. Most commonly, a separation will occur if a person is discharged from hospital, including if they are transferred to another facility or type of care.
7 From 2008 to 2017, the Australian Government owned and directly funded the Mersey Community Hospital in Tasmania. It was operated by a regional health organisation under the Tasmanian Government. The Australian Government also has agreements with all state governments to provide treatment and care to eligible members of the veteran community in their public hospitals.
8 Consistent with the terminology in the National Health Reform Agreement (NHRA), ‘state’ includes references to the Northern Territory and the Australian Capital Territory.
9 In 2011–12, the Australian Government provided $12.55 billion through the National Healthcare Specific Purpose Payment (NHSPP) block funding agreement.
10 Over the three-year life of the NHSPP, the annual growth in Australian Government funding was 6.1 per cent.
11 For example, in 2011–12, the Australian Government provided $759.3 million under the National Partnership Agreement (NPA) on improving Public Hospital Services. This NPA ceased on 1 July 2015.
12 Under the NHRA, State Governments have sole responsibility for capital funding of public hospitals.
13 The position of the Administrator is underpinned by legislation in each state as well as the Australian Government. Appointment of the Administrator requires the agreement of all jurisdictions. The Administrator can be dismissed by a majority vote of the Australian and state health ministers.
14 Subject to some broad funding commitments contained in the NHRA, it is up to individual state governments to determine the funding amounts they provide to the public hospitals within their health systems.
15 For Australian Government ABF calculation purposes, the previous year’s funding amount may adjusted through a ‘back-casting’ process. This is to ensure the calculation of funding is not adversely impacted by changes to ABF classification systems or costing methodologies made between consecutive years.
16 Services are measured as national weighted activity units (NWAUs). See Box 2 for an explanation of NWAUs.
17 Before undertaking the calculation of the NEP and NEC, the Pricing Authority releases an annual Pricing Framework for Australian Public Hospital Services consultation paper to seek feedback on a range of technical and policy considerations relevant to the determination of the NEP and NEC. Stakeholder submissions are published by the Pricing Authority on its website.
18 The accuracy or effectiveness of this discount applied to ABF for private patients is not within the scope of this audit. The general issue on MBS payments for public hospital services in discussed in paragraphs 2.63-71.
19 Reasons include when the number of services provided by a hospital is too small for them to have sufficient economy of scale to be funded under the national efficient price arrangements; or where hospital functions such as teaching, training and research are not yet able to be measured in ‘activity’ terms.
20 The National Efficient Cost for 2018–19 is $5.171 million and represents the average cost of small rural hospitals across Australia. Small rural hospitals are grouped according to their type, service volume and location, and funded according to their grouping with reference to the NEC.
21 These are the payments calculated prior to the application of the Funding Cap.
22 The AIHW is an Australian Government statutory entity. Its purpose is to create authoritative and accessible information and statistics that inform decisions and improve the health and welfare of all Australians.
23 The results of the review are discussed in paragraph 2.24.
24 Clause A39 of the NHRA states that the calculations for the Australian Government percentage funding rate for each service category for each state relate to preliminary payment entitlements, with final payment entitlements being made after reconciliation adjustments have been completed.
25 Efficient growth means the combined effect of the price and service volume adjustments referred to in paragraph 1.11.
26 This is based on the actual amount paid in the relevant year: $13.870 billion in 2013–14, $15.463 billion in 2014–15 and $17.179 billion in 2015–16.
27 Sentinel events are a list of defined adverse events occurring in hospital that result in death or serious harm to a patient. An example is a patient dying because of a medication error.
28 Auditor-General Report No. 18 2017–18 Monitoring the Impact of Australian School Funding.
29 Evidence was obtained from six of the eight offices of state Auditors-General. Contact was also made with state health departments – evidence was obtained from one department.
30 Data integrity is not defined for the purpose of the NHRA, however the OECD statistical glossary defines data integrity as ‘values and related practices that maintain confidence in the eyes of the users in the agency producing statistics and ultimately in the statistical product’.
31 Some state Auditors-General have also undertaken audits of governance arrangements for the collection of ABF-related data in their jurisdictions. Further details are in Appendix 2.
32 A number of states did agree to provide their data integrity frameworks to assist the Funding Body to better understand the rigour and approach undertaken to data integrity. However, this work has been delayed while other priorities have been progressed, notably the finalisation of the 2015–16 and 2016–17 reconciliation processes during 2018.
33 Data compliance reports are published on the Administrator’s website.
34 See footnote 32.
35 Hospitals will assign a code from a nationally agreed classification list to every hospital service (episode of care) they provide. The code affects the NWAU value assigned to the service and ultimately the amount of Australian Government funding received.
36 The Pricing Authority is currently conducting a review on all its corporate policies for alignment with Commonwealth requirements, including its risk management policy and framework. Refer paragraph 2.42.
37 Classifications are comprised of codes that provide clinically meaningful ways of relating the types of patients treated by a hospital to the resources required. Classification systems enable clinical information that is written in medical charts to be converted into manageable data categories. The approved classifications applicable to each activity data stream contribute to the ability to group hospital data as needed to develop the NEP. The Pricing Authority undertakes reviews and updates of existing classifications and is also responsible under the National Health Reform Act 2011 for introducing new classifications for those service categories without an existing classification for activity based funding purposes.
38 Data specifications relate to the technical standard to which the relevant data is being collected. For example, data can be collected according to: existing national minimum data sets standards, which has nationally agreed metadata standards for health statistics and information; or, national best endeavours data set standards, where metadata sets are not mandated for national collection but there is commitment to provide nationally on a best endeavours basis. The data specifications for ABF are published annually for each activity data stream and stored in the AIHW’s metadata online registry.
39 The entities also tailor information in their three year data plans. The Funding Body’s 2018–19 data plan provides that activity data is able to be directly submitted to the Funding Body through a dropbox.
40 As at November 2018, the Pricing Authority was updating the Data Quality Assurance Framework to reflect current NHRA terminology.
41 The introduction of the SDMS in 2017 also facilitates the ‘single submission, multiple use’ principle under the NHRA.
42 The severity of the error, the volume of errors and the type of data field affected by the error influences how the Pricing Authority responds to the jurisdiction. The Pricing Authority will not accept activity data if the file fails the data structure validation or if the file contains a fatal error where the state record identifier is either blank or not unique. Cost data is rejected if the data contains critical errors that are outlined in the data specification requirements. The Pricing Authority communicates with the jurisdiction and may request resubmission where validation errors may impact on the ability of the Pricing Authority to use the data in the models to determine the NEP and the NEC.
43 Anomalies are unusual changes in data, such as a large increase in the number of episodes of activity or the cost of activities compared to the previous year, which may or may not be within the thresholds defined by the Pricing Authority. The Pricing Authority highlights these changes for an explanation from the states.
44 Outliers are reported for each activity data stream and are measured against thresholds defined by the Pricing Authority for each category. For example, the low cost threshold for episodes of acute activity is $23 and the high cost threshold is $500,000. All data results falling outside of these parameters are identified and reported. Data streams with high levels of outliers are indicated for further review.
45 The quality assurance reports include traffic light reporting on the number of issues found in the five streams of activity data collected: acute; subacute; emergency; non-admitted; and mental health. The reports also include movements in cost and activity by stream and product type, average cost by product, proportion of overheads and intensive care hours. All the activity data used in the report is included by stream with the associated total separations and average total cost for the previous and the current year.
46 Traffic light reporting indicates the status of data submissions in terms of timeliness and issues being dealt with by the Pricing Authority data acquisition team are also noted.
47 Clause B102 of the NHRA requires that ‘each body will publish details of the Commonwealth and State compliance with the data requirements of the national bodies on a quarterly basis’. The Pricing Authority maintains a schedule of data submission timeframe requirements, articulated in its data plan, to enable sufficient time for resubmissions, validation and quality assurance processes, as well as consultation periods required during the price setting.
48 The review did recommend that hospitals and jurisdictions should continue to investigate reasons for unlinked/unmatched and out-of-scope activity to ensure appropriate treatment in future rounds. The remaining recommendations were regarding adjustments to the review process.
49 A financial and activity reconciliation must accompany the cost data for each hospital/costing site; and each jurisdiction would have to confirm that they have applied the Australian hospital pricing costing standards, or identify where and why the standards were not applied. This is currently provided in the data quality statements that accompany state cost data submissions.
50 The sampled hospitals and LHNs are named in the review report, and commentary included regarding how the sampled population conforms to the guidelines.
51 For the 2017-18 cost data collection (relevant data is due to be submitted by 28 February 2019), states have been asked to supply a self-assessment for each hospital or LHN as part of the National Hospital Cost Data Collection (NHCDC) data specifications requirements. The Pricing Authority advised that ANAO the self-assessment covers many of the areas in the financial review, and that the data items collected in the self-assessments are anticipated to inform the selection of hospitals for the financial reviews in the future.
52 The most recent example of this happening was in 2015–16. However, in that instance, the relevant state did provide further information after the initial NEC determination. As a result, the block funding amount was revised upwards through a supplementary determination.
53 State governments provide aggregate NWAU estimates by service category by 31 March to inform the Commonwealth Budget Process. They provide NWAU estimates by LHN by the 30 May to enable funding for the upcoming financial year.
54 These updates can be binding meaning that funding is adjusted going forward and revision of the relevant local hospital network service level agreement is required, or non-binding, which involves the Funding Body informing the relevant state the funding impact of the service level revision.
55 The format and content of SLAs varies between jurisdictions, but all SLAs reviewed by the ANAO contained the forecast level of public hospital services (expressed as NWAUs) that the relevant LHN would provide in each service activity category such as admitted acute care, emergency department and outpatient care. SLAs are updated annually.
56 The jurisdictional advisory committee to the Administrator includes representatives of the state and Australian Government health departments, with the Pricing Authority and Department of Treasury also attending. The committee advises on the potential effects of proposed or existing processes relating to the responsibilities of the Administrator and also provides collaboration on the relevant operational arrangements and priorities under the Agreement and the National Health Reform Act.
57 The major adjustments related to changes to technical classifications of some hospital procedures (reduction of $203 million) and changes to classifications involving some long-stay mental health patients (reduction of $91 million).
58 Combined with the $354 million 2016–17 half year adjustment already made, this $307 million took the total 2016–2017 adjustment to $661 million.
59 One of the criticisms noted in the Administrator’s advice was that states considered adjustments associated with changes to classifications were effectively ‘retrospective … and States had planned on the basis of the estimated Commonwealth payment’.
60 ‘Back-casting’ applies current year factors to the previous year, to enable growth calculations on comparable data. This is further discussed at paragraph 2.58.
61 As previously mentioned in Table 2.4, the CRMP provides that it is a matter of good practice for the Pricing Authority to align its risk management frameworks as a corporate Commonwealth entity. The Funding Body, as a non-corporate Commonwealth entity must comply with the CRMP.
62 The Funding Body relies on the Pricing Authority for processing the hospital activity data. Additional to the Pricing Authority, the Funding Body’s external systemic risk framework also identifies the following key entities in relation to data: state health ministers and Departments for the provision of activity data; and, the Commonwealth Department of Health for provision of MBS and PBS data for data matching purposes.
63 The draft funding pool risk register lists a number of entities with which the Funding Body has recognised shared risks, including: the Pricing Authority; state governments; the Department of Health and the Department of Human Services. The funding pool risk register includes a high level description of risks associated with its dependencies on other entities to conduct its functions.
64 The technical advisory committee (TAC) is a sub-committee of the Pricing Authority’s jurisdictional advisory committee and includes membership from the each state, the Australian Department of Health and the Funding Body. The TAC oversees the technical aspects on the delivery of costing, classification, data processing and modelling that underpins the development of activity based funding.
65 The Pricing Authority jurisdictional advisory committee is established under s.195 of the National Health Reform Act 2011 and provides advice to the Pricing Authority Board on matters relating to the entity’s work program. Membership consists of a Chair, plus a representative from each state and the Commonwealth Government.
66 The Department of Finance RMG 211 Implementing the Commonwealth Risk Management Policy - Guidance states that it is ‘important that entities, in collaboration with their stakeholders cooperate to identify and manage risks, develop clear roles and responsibilities for managing these risks and agree to outcomes.’ RMG 211 suggests that one option in this regard is for entities to ‘establish memoranda of understanding with partners to formalise an agreed understanding of responsibilities and expectations for managing shared risks.’
67 The review includes all policies except for information and communication technologies (ICT) policies; human resource policies; and procurement and finance documentation.
68 New teams were created in the Pricing Authority for classifications and data analytics work.
69 For example the Pricing Authority’s three year data plan for 2018–19 to 2020–21 includes a requirement to change from biannual submission of activity data to quarterly submissions.
70 The Funding Body’s actions relating to the 2018 reviews finding around cyber security were not assessed by this audit.
71 In 2018, the Funding Body’s risk management framework was assessed as ‘integrated’ – the third highest level from a possible six levels of maturity.
72 The Pricing Authority analyses changes in: product type; the average cost by product; proportions of overheads; average cost of cost buckets and overheads by data stream; outlier episodes for each stream; and the total hours of intensive care unit episodes. All the activity data used in the quality assurance report is shown grouped by data stream and product, including total separations and average costs of activity.
73 Clause B95 of the NHRA states that the Commonwealth (Australian Government) and states will take responsibility for the data integrity within their systems, which means that the Pricing Authority does not have a specific mandate to undertake formal quality assurance of activity data, such as audits.
74 Reporting includes information on separations and NWAU counts by service stream by state, including percentage changes across recent reporting periods.
75 The Australian Government Health Minister requested that the Pricing Authority to assess and investigate changes and anomalies in hospital reporting and trends across all service categories (including changes as a result of service complexity); and provide advice on possible drivers and causes of unexplained activity/NWAU growth. The report covered analysis of activity data from 2012 to the available data in the first half of 2016–17 and was provided to the Commonwealth Minister in August 2017. A second report was completed in April 2018 and provides analysis on the growth in admitted acute activity data and non-admitted activity data between 2015–16 and 2016–17, identifying the significant drivers of growth. The report builds on previous activity data analysis provided in response to the request from the Commonwealth Health Minster to explain the increase in Commonwealth funding contributions.
76 Once endorsed the cost reports are provided to states for a 45 day consultation period as required under the NHRA Act, prior to publication.
77 As previously mentioned in paragraph 2.28 in 2015–16 reconciliation funding was $512 million above original estimates, and similarly in 2016–17 it was $661 million above original estimates.
78 At the same time that the Funding Body was investigating the reasons for growth, the Pricing Authority was undertaking analysis on activity data in response to the Commonwealth Minister for Health (refer footnote 75).
79 Made up of $81.1m reduction for pricing errors, $15.2m for counting methodology issues and $26.4m for classification issues.
80 This change was the result of the move from Australian Refined Diagnosis Related Group (AR-DRG) v7.0 to AR-DRG v8.0. AR-DRGs are an Australian admitted patient classification system which provides a clinically meaningful way of relating the number and type of patients treated in a hospital (known as hospital casemix) to the resources required by the hospital. Each AR-DRG represents a class of patients with similar clinical conditions requiring similar hospital services. The change from AR-DRG v7.0 to v8.0 saw an increase in separations of patients with major complexity diagnosis codes and therefore increase in major complexity NWAUs.
81 Clause A40 of the NHRA provides that if the Pricing Authority makes any significant changes to the ABF classification systems or costing methodologies, the effect of such changes must be back-cast to the year prior to their implementation for ABF calculation purposes.
82 In March 2016 a combined Administrators jurisdictional advisory committee, chief financial officer and reconciliation advisory group workshop was held to discuss the use of linked data, including: legislation and governance; data analysis; and privacy, data security and access.
83 The MBS is a program under which the Australian Government partly or fully subsides a range of medical and hospital services. Depending on the circumstances, the providers of the service can receive a payment from the Australian Government according to the rebate amount listed in the MBS.
84 The Australian Government also subsidises the cost of medicines listed in the PBS. While PBS medicines are mostly dispensed by pharmacists, some medicines (such as chemotherapy drugs) and are only accessible at specialised medical services, usually hospitals.
85 Deterministic linking uses a unique identifier to link records that refer to the same entity. In this case, the Medicare PIN links the hospital service to the MBS record.
86 The two data sets that are ‘linked’ are hospital services data provided by states, and MBS data provided by the Australian Government.
87 A similar data matching process for PBS data in 2013–14 matched a total of PBS benefits of $6.8 million, though these matches have not been confirmed as ‘true’ matches of double funding. There was no adjustment to Australian Government funding as a result of these matches.
88 The Funding Body also advised the ANAO that they anticipated that a report on the data matching project would be provided to COAG Health Ministers for possible endorsement around May 2019.
89 The remaining $0.5 million was recovery of incorrectly paid benefits for pathology and diagnostic imaging services in public hospital emergency departments.
90 A full list of the Performance and Accountability Framework hospital-related indicators is in Appendix 3.
91 The National Health Performance Framework was developed in 2001 under the auspice of the Australian Health Minister’s Advisory Council. It was intended to provide a conceptual framework to understand and evaluate the health of Australians and the health system, including to assist planning efforts. The AIHW reports biennially on the national health performance indicators in the Australia’s health report.
92 Total Australian and state government NHR funding for NSW public hospitals in 2017–18 was $13.25 billion, of which $6.02 billion was Australian Government Funding.
93 ABF amounts transferred to LHNs are also reported in the NSW State Pool Financial Statements which form part of the Administrator’s annual report. These amounts are independently audited by the NSW Audit Office.
94 This is based on the most recent available (2016–17) comparative figures: $44.11 billion total NHR funding (adjusted for cross border payments); and $53.51 billion total public hospital funding reported by the AIHW. The Funding Body advised the ANAO that discussions have commenced with the AIHW regarding how the two organisations report public hospital funding levels.
95 Note the amount actually paid by the Australian Government in each financial year partly depends on the timing of when final reconciliation payments for prior year services are made. For example, $0.55 billion of the total amount paid in 2017–18 was for services delivered in the 2014–15, 2015–16, and 2017–18 years.
96 There has been significant variation between jurisdictions: state government NHR funding of Northern Territory public hospitals has increased by 81.5 per cent over five years; in NSW the increase has been 6.7 per cent, and in Western Australian there has been a decrease of 30.7 per cent. For these calculations cross border funding received by a state are counted towards its funding amount.
97 This consists of $20.79 billion for 2018–19 services and $0.63 billion for services provided in 2016–17 and 2017–18.
98 The cap applies to limit the growth of funding payable for services delivered in consecutive years rather than the funding actually paid in consecutive years.
99 This excludes reconciliation payments made for prior year services but includes estimated 2017–18 reconciliation payments to be made post 1 July 2018.
100 The notional funding entitlement for the Northern Territory grew by 8.2 per cent in 2017–18. Under the cap arrangements, ‘surplus’ Australian Government funds can be distributed to states that exceed 6.5 per cent growth.
101 The NHRA does not require states to direct all their public hospital funding to the National Pool or State Managed Funds, reducing the overall transparency of funding flows. Clause B22 of the NHRA does allow for ‘additional streams of funding’ to be incorporated in to National Funding Pool arrangements to ‘optimise transparency’ but this has not been used.
102 These are the number of NWAUs to be delivered by ABF hospitals within the LHNs. The 270,000 NWAUs delivered by small block funded rural and regional public hospitals are not included in the Administrator’s public reports.
103 Where patients normally reside in one jurisdiction and receive a public hospital service in another jurisdiction, the relevant NWAUs are recorded against the jurisdiction in which the service is provided.
104 Actual NWAUs delivered in 2016–17 were 5.9 per cent greater than forecast. Notably, changes to hospital service classification applying in 2016–17 which were designed to more accurately reflect the clinical complexity (and hence NWAU weighting) of services contributed to unexpected growth in NWAUs. Essentially, the number of NWAUs grew faster than the number of separations. Previously, growth in separations had outstripped NWAU growth.
105 According to Health’s 2014–15 Portfolio Budget Statement, the agreement was terminated ‘in light of States’ and Territories’ limited performance to date against [the] targets’.
106 In this measure, the average cost is adjusted, or ‘weighted’ to take account of case mixes so as to allow a comparison of costs between different hospitals and over time.
107 However, this indicator needs to be viewed in the context of the set of performance indicators as a whole, as decreasing cost could also be associated with decreasing quality and effectiveness.
108 SCRGSP (Steering Committee for the Review of Government Service Provision) 2018, Report on Government Services 2018, Productivity Commission, Canberra.
109 A comparison between jurisdictions regarding the weighted average cost of separations is in Appendix 4.
110 By comparison, for Australian Government funding only, the number of NWAUs per $1000 delivered on a national basis has declined slightly from 0.44 in 2012–13 to 0.42 in 2017–18 (a 4.5 per cent decrease)
111 See findings by the ACT, Victorian and Queensland Auditors-General summarised in Appendix 2.
112 A person is generally only placed on the waiting list once they have been seen by a specialist. Given there can be delays in accessing a specialist, the AIHW is developing reporting that will measure waiting time from the date of referral by the patient’s general practitioner.
113 However the AIHW reports have noted variation in the assignment of the urgency categories, both among and within jurisdictions, and for individual surgical specialties and surgical procedures. These variations means that caution should be used when comparing the relative performance between jurisdictions. The nature of the data has also not allowed the ANAO to calculate a national average.
114 The other main indicator for patient access to elective surgery – median waiting time – has however has increased over the life of the NHRA from 36 days in 2012-13 to 40 days in 2017–18.
115 A person must be readmitted to the same public hospital within the relevant time period to be counted as an ‘avoidable’ readmission.
116 Clinical quality registries collect and analyse health data to monitor the quality of health care against benchmarks and identify variations in clinical outcomes. They feed this information back to clinicians to inform clinical practice and decision making.
117 NSW uses a local name ‘Local Hospital Districts’ to refer to the national entity name ‘Local Hospital Networks’ (LHNs).