Browse our range of reports and publications including performance and financial statement audit reports, assurance review reports, information reports and annual reports.
Administration of Medicare Electronic Claiming Arrangements

Please direct enquiries relating to reports through our contact page.
The objective of the audit was to assess the effectiveness of Medicare electronic claiming arrangements, including an assessment of the extent to which claiming and processing efficiencies for the Government, health professionals and Medicare customers have been achieved.
Summary and recommendations
Background
1. Electronic claiming for Medicare benefits was first introduced in 1992. Channels to facilitate electronic claiming were progressively introduced for use by medical practitioners, members of the public and private health insurers over the intervening decades. In 2016–17, claims for just over 97 per cent of the approximately $22 billion of Medicare benefits paid were lodged electronically.
2. The Department of Human Services (Human Services or the department) currently administers eight electronic claiming channels: six provider channels for point of service claiming1 and two channels for claiming by patients at their convenience. In addition Human Services provides a number of manual claiming options (in-person, dropbox, post and phone). Most of the electronic claiming channels were introduced ten or more years ago—prior to Medicare’s integration into the Department of Human Services in July 2011.2 The provider channels are:
- Simple Mail Transfer Protocol (1999);
- Medicare Online (2002);
- Electronic Claim Lodgement and Information Processing Service Environment (2004);
- Easyclaim (2007);
- Bulk Bill Webclaim (2015); and
- Patient Claim Webclaim (2016);
3. The additional channels for use by patients are Claiming Medicare Benefits Online (2011) and Express Plus Medicare Mobile App (2013).
4. The department’s administration of claiming channels is focussed on its overarching strategy of achieving as close as possible to 100 per cent electronic claiming.
5. On 19 October 2016, the Government announced it will replace the current systems used by Human Services to deliver health, aged care and related veterans’ payments as they are ‘old, complex and at risk of failure and therefore need to be upgraded’.3 The program of work is being led by the Department of Health and supported by the Departments of Human Services and Veterans’ Affairs, and the Digital Transformation Agency. This decision provides Human Services a further opportunity to consider what if any changes could be made to the current channel service offer.
Audit objective and criteria
6. The objective of this audit was to assess the effectiveness of Medicare electronic claiming arrangements, including an assessment of the extent to which claiming and processing efficiencies for the Government, health professionals and Medicare customers have been achieved.
7. To form a conclusion against the audit objective, the ANAO adopted the following high level criteria:
- Was effective planning undertaken for the implementation and ongoing delivery of Medicare electronic claiming channels?
- Has the implementation and ongoing delivery of Medicare electronic claiming channels been effective?
- Does Human Services monitor and evaluate the efficiency and effectiveness with which it delivers Medicare electronic claiming?
Audit methodology
8. The audit’s methodology included:
- examination of documentation relating to the administration of Medicare electronic claiming channels, including program documentation and performance reports;
- review and analysis of departmental data related to the performance (take-up, costs/savings and timeliness) of the range of electronic channels currently available;
- ANAO analysis of quantitative data from Human Services ICT systems; and
- interviews with relevant departmental staff.
Conclusion
9. The Department of Human Services has been effective in driving the take-up of Medicare electronic claiming, with more than 97 per cent of all claims for Medicare services being lodged electronically. The department’s approach to implementing future Medicare electronic claiming could be improved by clear analysis of the costs of developing and maintaining individual claiming channels and the extent to which planned efficiencies have been realised.
10. The objectives of introducing electronic claiming (to improve convenience and timeliness and reduce costs to Government and the health care sector) have been met through the introduction of a range of individual channels over time to allow claiming by different users. Human Services has mechanisms in place to identify issues and consider whether channels can be improved to meet user needs.
11. The introduction of electronic claiming channels has led to improved access to payments for the community and providers. More than 97 per cent of claims for Medicare services are lodged electronically and a majority of these are paid within one day of lodgement.
12. The ANAO reviewed the available data related to expected savings and costs from implementing electronic claiming channels. These expected savings were only estimated by Human Services in some cases. Where estimates were made either take-up rates or dollar savings have not been achieved.
13. Although the department monitors rates of electronic lodgement and tracks movements between channels by claim type and reductions in manual services, the long term benefits and relative efficiencies from introducing individual channels are largely unknown.
14. Human Services’ monitoring and reporting includes business analytics used to inform channel delivery, and departmental management of risks and issues are supported by a range of plans. The department’s delivery of claiming channels is not supported by either: benchmarking of expected achievements; or a full understanding of the costs and benefits of individual claiming channels. There is a lack of information on whether the development of individual channels has delivered the intended administrative savings; and whether the savings achieved have outweighed the costs of introducing new channels. As such the department has not established a sufficiently strong information base to inform its business decisions.
Supporting findings
Planning and strategy
15. The Department of Human Services has identified the objectives and intended benefits of electronic claiming. The overall intent of introducing electronic claiming has been to increase the convenience to providers and patients, reduce costs to government and medical providers and improve the timeliness of claim processing. These objectives are consistent with Human Services’ Channel Strategy and Digital Transformation Strategy and its current strategy to deliver as close as possible to 100 per cent of electronic claiming at point of service.
16. Electronic claiming channels have been developed to meet the needs of providers, patients and private health insurers, and to reduce manual processing for the department. The available channels allow claiming across the three claiming/billing methods and for the claims to be lodged at the point of service or at a time convenient to the claimant.
17. Human Services engages with peak stakeholder groups and providers to share information about business issues and consider improvements. The department measures channel usage and conducts analysis to identify health practices that continue to lodge manual claims. This data, along with the stakeholder feedback, is used by the department to target strategies to promote electronic claiming.
Implementation
18. The high level of provider and patient take-up of electronic claiming (with 97.1 per cent of claims for services lodged electronically at the point of service) reflects the convenience, accessibility and timeliness of electronic claiming.
19. Efforts undertaken by Human Services to increase electronic patient claiming rates for services provided by general practitioners and specialists have been successful albeit there is scope to improve claiming rates for other practitioners, in particular pathologists, although increasing the number of pathology claims lodged at the point of service may require adjustments to the legislative framework. Patient claims account for less than two per cent of all claimed pathology services but around 20 per cent of all patient claims lodged manually.
20. Given that Human Services has achieved 97.1 per cent electronic claiming at an aggregate level it is expected that savings to the department have been realised overall. The costs associated with introducing and maintaining these electronic claiming channels have not been tracked over time and the expected savings from introducing individual channels have not been realised within anticipated timeframes.
21. Anticipated savings for each channel have been estimated using standard assumptions of the price differential between manual and electronic claiming and projected channel take-up rates. The department has consistently overestimated the take-up rates when introducing new channels and has not followed up to determine whether the cost savings for individual channels have been met.
22. Human Services does not currently track the relative costs of maintaining each claiming channel. There would be benefit in Human Services developing the capability to better understand the costs of each channel, as well as the administrative savings and other benefits that have been realised, to support decisions about future directions for, and investments in, electronic claiming.
23. Electronic claiming allows for increased automation of processing and payment of Medicare benefits and has improved timeliness. Not all electronic claims are able to be processed automatically. Human Services continues to make system enhancements to reduce the amount of manual intervention required.
Monitoring and reporting
24. Human Services has established relevant monitoring and reporting against its objective of attaining as close as possible to 100 per cent electronic claiming at the point of service. These reporting mechanisms inform the department’s electronic claiming strategy. The department also monitors user satisfaction and service availability—information that can be used to highlight areas of improvement.
25. The department’s monitoring and reporting on channel delivery does not cover all relevant aspects of electronic claiming service delivery. The department does not monitor the ongoing administrative costs and benefits of individual channels and therefore has an incomplete understanding of the performance of each channel against their respective business objectives.
26. Risks to the administration of Medicare electronic claiming channels have been managed effectively. The key risks to Medicare payment integrity and system functionality are addressed in a range of plans.
27. The Modernising Health and Aged Care Payments Services Program is in its early stages. Human Services is supporting the lead agency, the Department of Health, to understand the current state of service delivery and technology. Human Services’ principal role comprises remediation activities to allow existing systems to continue to operate reliably and effectively.
Recommendations
Recommendation no. 1
Paragraph 4.19
To better inform its ongoing business decisions, the Department of Human Services should ensure its electronic claiming channel delivery strategy is supported by clear analysis of the costs and benefits of:
- establishing and maintaining electronic claiming channels; and
- maintaining manual Medicare claiming options.
Department of Human Services response: Agreed.
Summary of entity responses
28. The summary response to the report from Human Services is provided below, with the covering letter included in Appendix 1.
The Department of Human Services (the department) welcomes the ANAO’s key finding that Medicare electronic claiming arrangements are effective, with more than 97 per cent of all Medicare services now lodged electronically. In line with the recommendation, the department will ensure that future decisions on its electronic claiming channel delivery strategy are supported by clear analysis of the costs and benefits.
Key learnings and opportunities for Australian Government entities
Below is a summary of key learnings and areas of good practice identified in this audit report that may be considered by other Commonwealth entities when implementing electronic services.
Performance and impact measurement
1. Background
Introduction
1.1 Medicare was introduced in 1984 to subsidise a range of medical services for Australian residents and certain categories of visitors. In 2016–17, 24.9 million people were enrolled in Medicare and $22.4 billion was paid in benefits for more than 399 million services. Medicare accounts for one-third of the Commonwealth health budget, with spending expected to increase every year—from $23.7 billion in 2017–18 to $27.9 billion in 2020–21.
1.2 Legislation covering the main elements of the Medicare program is contained in the Health Insurance Act 1973 (the Act). The Act provides that Medicare benefits are paid for clinically relevant services provided in Australia that are consistent with the legislative framework.
1.3 For Medicare benefits to be payable, the relevant professional service must be listed in relevant legislation, including Determinations. The fees for the service are included in the Medicare Benefits Schedule (MBS)—a listing of most of the Medicare services that are subsidised by the Australian Government (known as items). The MBS may be updated at any time during the year and currently lists over 5700 items.
1.4 Medical practitioners are able to set their own fees for their services. The Medicare benefit is therefore a subsidy for patients to provide them with financial assistance towards the costs of their medical services in circumstances where the amount of the subsidy is less than the total fee for the service.
1.5 The payment of benefits only occurs after a service has been rendered by a registered medical practitioner (provider) to a patient who is eligible for Medicare benefits. One or a number of services can be submitted together in a ‘claim’. There are three types of claims: patient, bulk bill and simplified billing:
- A health provider can ‘bulk bill’ a patient—this means that the claimant has assigned their right for the Medicare benefit to be paid to the health professional. The health provider can claim the Medicare benefit from the Department of Human Services (Human Services or the department) as full payment for the service and not charge the patient a fee.
- If the health provider charges the patient a fee for the service, the patient can claim the Medicare benefit by:
- paying the account, and then, if the health provider or practice offers electronic claiming, practice staff can lodge the claim electronically with Human Services from the point of service;
- paying the account and then claiming the Medicare benefit from Human Services either by mail, phone, in person at a service centre or by one of the two electronic claiming channels available for use by patients;
- lodging an unpaid account with Human Services and receiving a cheque made payable to the health provider which the patient gives to the provider along with any outstanding balance; or
- Claims for in-hospital services provided to patients can be made through simplified billing arrangements which streamlines the way patients pay their accounts and claim benefits from Human Services and their private health insurer. Simplified billing claims can be lodged by hospitals, billing agents, providers and day surgeries with both the department and private health insurers either electronically or manually.
1.6 In 2016–17, 399 485 575 Medicare services were processed by Human Services. Of these services:
- 78.5 per cent (313 576 052) were claimed through bulk billing;
- 13.3 per cent (52 968 967) were patient claimed; and
- 8.2 per cent (32 940 556) were claimed through simplified billing.
1.7 Appendix 2 illustrates the Medicare bulk bill and patient claim process from the point the patient receives the service, noting the points of patient, provider and Human Services involvement.
1.8 In 1992, the Health Insurance Commission (now Medicare Master Program in Human Services) developed and implemented electronic claiming systems. In addition to a number of manual claiming options (in-person, dropbox, post and phone) Human Services currently offers eight electronic claiming channels (described in Chapter 2). Most of these channels were implemented ten or more years ago.
1.9 Figure 1.1 shows that most services are claimed under bulk billing arrangements and that electronic lodgement is the preferred method for all billing types. The figure also shows that the proportion of patient claim services lodged electronically has been more variable and has improved substantially over the last five years (see also Figure 2.1). Although patient claim services account for only around 13 per cent of all services claimed in 2016–17, it is reductions in manual lodgement of these claims that has most contributed to the department’s electronic claiming take-up rate in recent years.
Figure 1.1: Lodgement of claims for Medicare services by claim and transmission type, 2012–13 to 2016–17
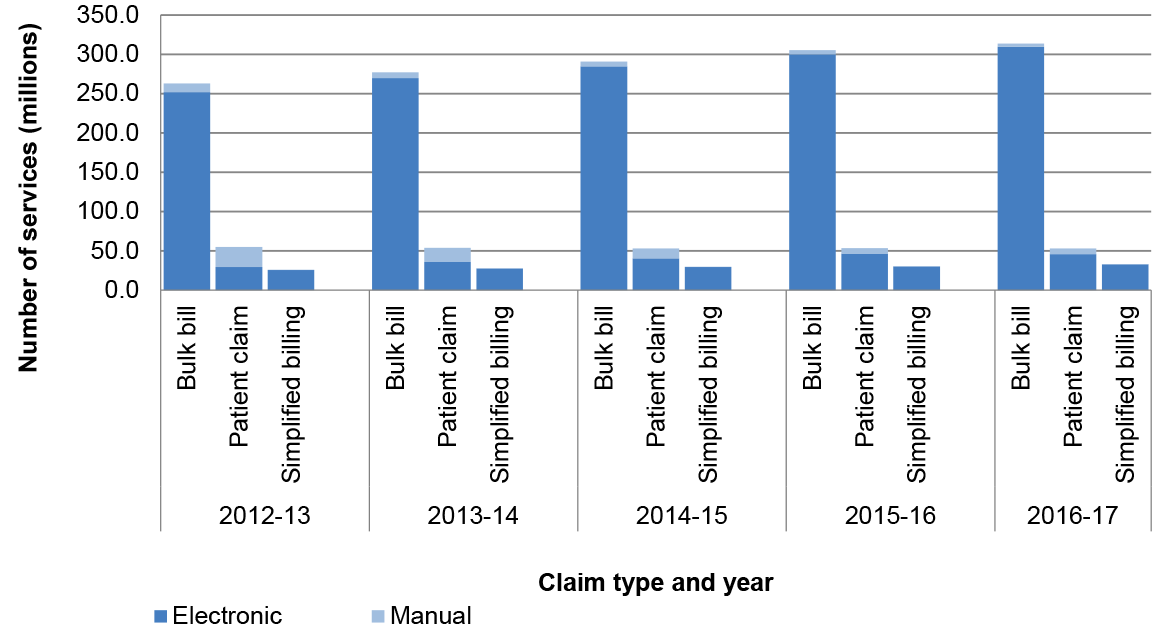
Source: ANAO analysis of Department of Human Services’ Annual Reports (2012–13 to 2016–17).
Department of Human Services’ administrative roles and responsibilities
1.10 Human Services administers Medicare payments on behalf of the Department of Health. The Bilateral Head Agreement between the Secretaries of Human Services and the Department of Health sets out the governance framework and requirements for both departments.
1.11 Human Services administers the payment of Medicare benefits by:
- enrolling eligible Australians and visitors for Medicare and registering individuals and families for the Medicare Safety Net4;
- registering health practitioners (for Medicare provider numbers), accredited diagnostic imaging facilities and their equipment and, accredited pathology facilities;
- assessing eligibility for Medicare levy exemptions;
- assessing, approving and paying Medicare benefits (to patients, providers, Private Health Insurers and Billing Agents); and
- conducting patient compliance activities.5
Previous audit coverage
1.12 Previous ANAO audits relating to the administration of the Medicare program have included: audits of the accuracy of Medicare claims processing; the management of Medicare compliance audits; and the management and integrity of Medicare customer data.6
Audit objective, criteria and methodology
Audit objective and criteria
1.13 The objective of this audit was to assess the effectiveness of Medicare electronic claiming arrangements, including an assessment of the extent to which claiming and processing efficiencies for the Government, health professionals and Medicare customers have been achieved.
1.14 To form a conclusion against the audit objective, the ANAO adopted the following high level criteria:
- Was effective planning undertaken for the implementation and ongoing delivery of Medicare electronic claiming channels?
- Has the implementation and ongoing delivery of Medicare electronic claiming channels been effective?
- Does Human Services monitor and evaluate the efficiency and effectiveness with which it delivers Medicare electronic claiming?
1.15 The scope of the audit included a review of the arrangements in place to manage risks to payment integrity but did not otherwise examine the accuracy of claims processing, compliance arrangements or the integrity of customer data.
Audit methodology
1.16 The audit’s methodology included:
- examination of documentation relating to the administration of Medicare electronic claiming channels, including program documentation and performance reports;
- review and analysis of departmental data related to the performance (take-up, costs/savings and timeliness) of the range of electronic channels currently available;
- ANAO analysis of quantitative data from Human Services’ ICT systems; and
- interviews with relevant departmental staff.
1.17 The audit was conducted in accordance with ANAO Auditing Standards at a cost to the ANAO of approximately $432 100.
1.18 The team members for this audit were Tracy Cussen, Christine Preston, Hannah Climas, Fei Gao and Andrew Rodrigues.
2. Planning and strategy
Areas examined
This chapter identifies the objectives and anticipated benefits of implementing electronic claiming channels. It identifies the channels currently administered by the Department of Human Services and describes some of the mechanisms the department has in place to inform their understanding of channel user needs and experiences.
Conclusion
The objectives of introducing electronic claiming (to improve convenience and timeliness and reduce costs to Government and the health care sector) have been met through the introduction of a range of individual channels over time to allow claiming by different users. Human Services has mechanisms in place to identify issues and consider whether channels can be improved to meet user needs.
Have the objectives and intended benefits of electronic claiming been identified?
The Department of Human Services has identified the objectives and intended benefits of electronic claiming. The overall intent of introducing electronic claiming has been to increase the convenience to providers and patients, reduce costs to government and medical providers and improve the timeliness of claim processing. These objectives are consistent with Human Services’ Channel Strategy and Digital Transformation Strategy and its current strategy to deliver as close as possible to 100 per cent of electronic claiming at point of service.
Alignment with overarching strategies
2.1 Digital or electronic government service delivery is not a new concept. Since the late 1990s successive governments have made commitments7 to adopt online technologies to deliver services and improve business practices. Digital claiming of Medicare benefits is aligned with these commitments.
2.2 One of the objectives articulated in the Department of Human Services’ (Human Services or the department) Digital Transformation Strategy is to provide services that are ‘available digitally anywhere, anytime’. Key areas of focus under this strategy include: reducing demand on staff-assisted channels; migrating transactions to lower-cost channels; and complete end-to-end digitisation of processes.
Objectives and benefits of electronic claiming
2.3 A 2009 report8 identified that the Government’s overarching objectives in implementing Medicare electronic claiming were to:
- provide increased convenience to medical service providers and customers;
- provide cost savings for government and medical services providers; and
- improve the speed and quality of claims processing.9
2.4 Departmental documents from 2009 identified anticipated benefits from introducing electronic claiming including:
- reducing bulk bill paper claim form storage;
- enabling reconciliation of payments for bulk bill claims;
- improved customer service;
- reducing visits to Medicare offices;
- reducing the number of claims processing staff within Human Services;
- automating claims and payments processing; and
- reducing cheque payments to the public.
2.5 Table 2.1 indicates that most payments are made through Electronic Funds Transfer (EFT) and that the department has reduced or ceased less cost effective payment types over time. The department was unable to provide estimated administrative savings from reductions in the number of claims processing staff attributable to the introduction of electronic claiming.
Table 2.1: Medicare services by payment type, 2012–13 to 2016–17
|
|
2012–13 |
2013–14 |
2014–15 |
2015–16 |
2016–17 |
|||||
|
|
Number of services (million) |
% |
Number of services (million) |
% |
Number of services (million) |
% |
Number of services (million) |
% |
Number of services (million) |
% |
|
Cash to claimanta |
1.7 |
0.5 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
|
Cheque to health professionalb |
1.6 |
0.5 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
0.0 |
|
Cheque to claimantc |
3.4 |
1.0 |
3.3 |
0.9 |
3.0 |
0.8 |
2.7 |
0.7 |
-0.3 |
-0.1 |
|
EFT to claimantc |
34.4 |
10.0 |
36.6 |
10.2 |
35.6 |
9.5 |
35.3 |
9.1 |
38.0 |
9.5 |
|
EFTPOS payment to claimant |
9.3 |
2.7 |
8.6 |
2.4 |
9.8 |
2.6 |
11.0 |
2.8 |
11.6 |
2.9 |
|
EFT to health professional |
261.4 |
76.0 |
276.8 |
77.3 |
290.6 |
77.8 |
305.2 |
78.4 |
313.6 |
78.5 |
|
Pay doctor via claimant cheque |
6.4 |
1.9 |
5.4 |
1.5 |
4.8 |
1.3 |
4.3 |
1.1 |
3.7 |
0.9 |
|
Payment to private health fund or billing agent |
25.8 |
7.5 |
27.5 |
7.7 |
29.6 |
7.9 |
30.5 |
7.8 |
32.9 |
8.2 |
|
Total servicesd |
344.0 |
|
358.3 |
|
373.4 |
|
389.1 |
|
399.5 |
|
Note a: Cash payments were phased out from 1 July 2012.
Note b: Payments by cheque to health professionals for bulk billing services ceased on 1 November 2012.
Note c: From 1 July 2016 payments by credit EFTPOS in service centres or by cheque, with the exception of Pay Doctor Via Claimant Cheques, ceased.
Note d: Totals may differ due to rounding.
Source: ANAO analysis of the Department of Human Services’ Annual Reports (2012–13 to 2016–17).
2.6 In 2014, an internal Claiming and Payment Strategy business case was drafted to support ongoing activities to promote and strengthen electronic claiming. The business case outlined the department’s aim to create efficiencies for Government and reduce red tape for the health sector by:
- making it easier for the Australian public and health professionals to receive Medicare benefits through claiming channels that are efficient and easy to access; and
- creating savings for Government by transforming Medicare’s electronic claiming systems through new technology that provides efficiency and scalability for all claiming into the future.
2.7 In February 2015 this strategy was launched as the Medicare Digital Claiming Strategy10 and remains the current operational electronic claiming strategy. The objective underpinning this strategy is to maximise digital claiming for Medicare benefits at the point of service as this:
requires the least amount of effort for customers as no additional engagement is required with the department for patients to make a Medicare claim [and] involves the lowest processing cost for the department.
2.8 Human Services has focused on increasing electronic patient claiming rates in support of their overall strategy. The number of services claimed by patients annually has remained relatively consistent over the last five years with a decrease of around 2 million claims between 2012–13 and 2016–17. The proportion of patient claimed services lodged electronically has risen substantially over this time—from around 54 per cent of all patient claimed services in 2012–13 (29.6 million services) to 86.4 per cent (45.8 million services) in 2016–17.
Figure 2.1: Patient claiming by lodgement type—electronic vs manual, 2012–2017
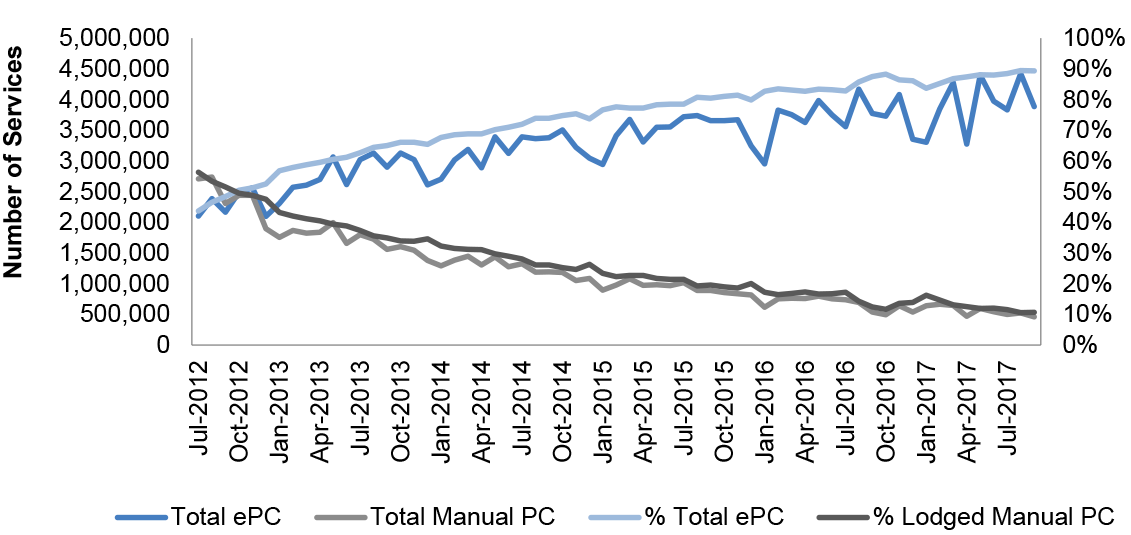
Note: References to PC and ePC in legend refer to Patient Claim and electronic Patient Claim.
Source: Department of Human Services’ administrative data.
Have channels been developed to meet the needs of the community, providers and government?
Electronic claiming channels have been developed to meet the needs of providers, patients and private health insurers, and to reduce manual processing for the department. The available channels allow claiming across the three claiming/billing methods and for the claims to be lodged at the point of service or at a time convenient to the claimant.
Human Services engages with peak stakeholder groups and providers to share information about business issues and consider improvements. The department measures channel usage and conducts analysis to identify health practices that continue to lodge manual claims. This data, along with the stakeholder feedback, is used by the department to target strategies to promote electronic claiming.
Channel coverage
2.9 Human Services’ documentation identifies that channel services were developed to: deliver payments in a timely, accurate and cost effective manner; ensure that intended recipients could easily access services; and provide an appropriate balance between convenience, reliability, security and efficiency in delivering payment services.
2.10 As noted in Chapter 1, the Medicare benefit is a patient benefit. If the provider agrees to accept the Medicare benefit as full payment for the service then the patient benefit becomes a ‘bulk bill’ claim and the health professional will claim the benefit directly from Human Services as full payment for the service. For services that are not bulk billed the patient pays the full fee charged11 for the service, and then claims the Medicate benefit through the practice submitting the claim electronically to Human Services on the patient’s behalf at the point of service or by using a self-service channel at a later time. For this reason claiming channels are required for both health care professionals and patients.
2.11 The channels are available across the three claiming/billing methods: bulk billing, patient claiming and simplified billing. The available channels also allow for the claim to be lodged at the point of service or in the recipient’s own time, depending on the circumstances (see Table 2.2).
Overview of electronic claiming channels
2.12 A number of current and historical drivers have impacted the development of claiming channels. These drivers include:
- the 1995 Private Health Insurance Reforms;
- the 2008 National eHealth Strategy;
- the 2010 Service Delivery Reform agenda;
- medical software vendors development of practice management software systems;
- electronic claiming development in other sectors (tax, private health insurance);
- consumer demand for electronic access;
- ICT investment decisions by health professionals; and
- the increased Government focus on reducing red tape for business.
2.13 Over time, electronic channels have evolved from systems that facilitate the lodgement of bulk billing claims by providers to systems that cater to a range of service settings (for example hospitals and medical practices) and those that allow patients to access claiming using digital channels.
2.14 There are currently eight electronic claiming channels: six of these channels facilitate point of service claiming by providers or patients and the remaining two patient channels facilitate claiming at the patient’s convenience. In addition, Human Services retains manual claiming options (in-person, dropbox, post and phone).
2.15 The Medicare electronic claiming options currently available are listed in Table 2.2. From these channels, collectively, around 388 million of the 399 million services (97.1 per cent) claimed in 2016–17 were lodged electronically. A breakdown of the volume and proportion of services claimed by individual channels is at Table 3.1.
Table 2.2: Current Medicare electronic claiming channels
|
How the claim is lodged |
Electronic claiming channel |
Channels details |
|
By the health professional at the point of service for both bulk bill and patient claims |
Medicare Online (2002) |
Supports claiming from doctor’s practices to Medicare via their practice management systems. There are approximately 300 vendors who have a Notice of Integration for online claiming which means their software is compatible with that used by Human Services. |
|
Medicare Easyclaim (2007) |
Allows practices to lodge claims using a secure EFTPOS network provided by five financial institutions contracted by Human Services. The Government pays the financial institutions 23 cents per successful transaction. |
|
|
Medicare Bulk Bill Webclaim (2015) |
Allows providers to lodge bulk bill claims using the Health Professionals Online Services (HPOS). |
|
|
Medicare Patient Claim Webclaim (2016) |
Allows providers to make claims on behalf of patients using the HPOS. |
|
|
By the patient after receiving an account (paid or unpaid) from the provider |
Claiming Medicare Benefits Online (CMBO) (2011) |
Allows patients to claim 23 of the most common MBS items over the internet. Claimants must register for a Medicare online account through myGov and are required to provide an image of the receipt. These claims are processed manually. |
|
Express Plus Medicare Mobile App (2013) |
Claimants must register for a Medicare online account through myGov and are required to provide an image of the receipt. These claims are processed manually. |
|
|
By hospitals, billing agents and providers for in-patient medical services where there is a Medicare and private health insurer component |
Electronic Claim Lodgement and Information Processing Service Environment, (ECLIPSE) (2004) |
Used for claiming Simplified Billing services. |
|
Simple Mail Transfer Protocol (SMTP) (1999) |
Used for claims lodged via email for claiming services provided in hospitals involving private health insurers paid directly to a provider, usually by EFT. |
|
Source: ANAO analysis of Department of Human Services’ documentation.
2.16 Although there is some overlap in the coverage of the electronic claiming channels (by claimant group and billing type) each was introduced to promote different efficiency objectives or to target different stakeholder groups:
- Medicare Online was introduced in 2002 as part of business improvement initiatives aimed at modernising claiming and payment processing.
- ECLIPSE, introduced in 2004, was developed to streamline the claims process for in-hospital patients covered by both Medicare and a private health fund.
- Easyclaim was introduced in 2007 as an alternative to Medicare Online, which at the time was seen to be a costly and ‘cumbersome’ channel. Easyclaim was designed to provide real time approval of claims and payments using EFTPOS technology.
- CMBO was introduced in 2011 to provide an alternative electronic claiming channel for claimants who could not, or choose not to, use claiming at point of service.
- The Express Plus Medicare Mobile App was introduced in 2013 to use new technologies and was developed in line with the Human Services’ introduction of Mobile App services to support Centrelink programs.
- Bulk Bill Webclaim and Patient Claim Webclaim, introduced in 2015 and 2016 respectively, were implemented, in part, to provide a free electronic claiming option in response to complaints from providers regarding the cost of purchasing practice management software to enable digital online claiming using other channels.
2.17 A 2014 discussion paper prepared within Human Services identified Medicare Online as ‘the gold standard claiming channel for the Department due to its simplicity for both providers and customers and high levels of program integrity for the department’ despite being the oldest claiming channel (aside from SMTP).
2.18 Providers can choose which channel they use, depending on their circumstances. Their choice may be influenced by the requirements established by Human Services to use electronic claiming which differ by channel. For example, use of both Medicare Online and ECLIPSE requires providers to purchase integrated practice management software and to comply with authentication and security requirements.12 For patients to use CMBO they must register for a Medicare online account, including providing bank account details, and link this account with myGov. For providers to use Easyclaim they must have an EFTPOS terminal provided by one of the five financial institutions contracted by Human Services to provide Easyclaim services.
Understanding user needs
2.19 Human Services engages with peak stakeholder groups and providers to support the ongoing management of channels. These forums provide opportunities to share information about business issues and consider improvements and have been effective in identifying barriers to stakeholder take-up of electronic claiming channels.13 The key engagement mechanisms are:
- Stakeholder Consultative Group—with representation from peak provider groups14;
- ECLIPSE Reference Group—with private health insurance industry representatives;
- Financial institutions—those under contract with Human Services to deliver Easyclaim services; and
- Outreach networks—Business Development Officers and Medical Liaison Officers that provide support to practices, providers and Aboriginal Medical Services.
Outreach networks
2.20 Human Services’ Business Development Officers (BDOs)15 undertake activities based on identified business priorities and the strategic direction of the department. To promote electronic claiming their role is broadly focused on educating health professionals about the range of electronic services available and how these services can reduce provider administrative costs and increase the timeliness of payments. The information gathered can then be used by Human Services to identify improvements or business process enhancements required for existing channels16 and in the development of new channels.
2.21 Departmental documentation reviewed by the ANAO indicates that, from 2012 through 2017, BDOs engaged providers, in-person or over the phone, to understand barriers to the take-up of electronic claiming and to discuss a range of business process enhancements. The impact of the strategies employed by BDO’s is discussed further in Chapter 3.
2.22 Human Services has identified that the barriers to stakeholders using electronic claiming are both cultural and system-based. The top five barriers to electronic claiming are:
- lack of knowledge of electronic claiming options;
- knowledge gaps in using practice management software;
- investment and upkeep of practice management software;
- understanding the Medicare Benefit Schedule and complexities associated with claim scenarios/items that can be claimed by channel; and
- patients not registering for a Medicare online account or failing to provide their bank details to the department.
2.23 The actions taken by the department to address these barriers include: educating practice staff and the public about electronic claiming availability and processes; discussing software-related issues with software vendors; making enhancements or amendments to system and business rules to improve functionality (see for example the discussion of the Reduction in Manual Intervention project from paragraph 3.64); and developing web-based claiming channels (Bulk Bill and Patient Claim Webclaim) that do not require investment in practice management software.
2.24 Human Services has also undertaken analysis to identify providers/practices that do not use or under-use electronic claiming. Several targeted strategies have been launched to promote the take-up of electronic claiming by these users. These are described in Chapter 3 from paragraph 3.16.
3. Implementation
Areas examined
This chapter examines the Department of Human Services’ delivery of electronic claiming objectives: improving access; providing savings/reducing costs for the department, practitioners and patients; and improving claim processing and payment timeliness.
Conclusion
The introduction of electronic claiming channels has led to improved access to payments for the community and providers. More than 97 per cent of claims for Medicare services are lodged electronically and a majority of these are paid within one day of lodgement.
The ANAO reviewed the available data related to expected savings and costs from implementing electronic claiming channels. These expected savings were only estimated by Human Services in some cases. Where estimates were made either take-up rates or dollar savings have not been achieved.
Although the department monitors rates of electronic lodgement and tracks movements between channels by claim type and reductions in manual services, the long term benefits and relative efficiencies from introducing individual channels are largely unknown.
Has electronic claiming improved the ease of access to payments for the community and providers?
The high level of provider and patient take-up of electronic claiming (with 97.1 per cent of claims for services lodged electronically at the point of service) reflects the convenience, accessibility and timeliness of electronic claiming.
Efforts undertaken by Human Services to increase electronic patient claiming rates for services provided by general practitioners and specialists have been successful albeit there is scope to improve claiming rates for other practitioners, in particular pathologists, although increasing the number of pathology claims lodged at the point of service may require adjustments to the legislative framework. Patient claims account for less than two per cent of all claimed pathology services but around 20 per cent of all patient claims lodged manually.
3.1 Electronic claiming provides an alternative way to claim Medicare payments to either visiting Medicare offices or posting claim forms. The convenience of lodging electronic claims for both providers and patients is evident. In 2016–17:
- 97.1 per cent of claims for services were lodged at the point of service;
- 2.9 per cent (around 11 million services) of claims were submitted manually; and
- 0.03 per cent of claims were lodged electronically, but not at the point of service.
3.2 Electronic claiming facilitates more timely payment of benefits (discussed further from paragraph 3.55). Medicare Online uses the bank account details provided by the patient to deposit their Medicare rebate into their bank account. Payment is generally received within two to three working days. Around 83 per cent (around 322 million) of all claims for services are lodged through this channel. Medicare Easyclaim provides a more immediate transfer of funds to the customer through the EFTPOS network. Easyclaim was used to lodge around eight per cent (around 32 million) of all claims for services in 2016–17.
Take-up of electronic claiming
3.3 The overall take-up of electronic claiming is high but there are marked differences in the use of each of the channels. Table 3.1 shows the proportion and volume of services lodged from seven of the current electronic claiming channels17 for the previous two financial years. The most widely used channel is Medicare Online which, on a monthly basis, is used by around half of all medical practices and was used to lodge around 83 per cent of all electronic claims in 2016–17 (92 per cent of electronic bulk bill claims and 64 per cent of electronic patient claims). For Simplified Billing claims, Electronic Claim Lodgement and Information Processing Service Environment (ECLIPSE) is the most commonly used channel (85 per cent of electronic claims).
Table 3.1: Volume of services by claiming channel in 2015–16 and 2016–17
|
Channel |
Type of claim |
2015–16 |
2016–17 |
||
|
|
|
Proportion of paid services (%) |
Volume of paid services (million) |
Proportion of paid services (%) |
Volume of paid services (million) |
|
Medicare Online |
Bulk Bill or patient |
80 |
312 |
81 |
322.3 |
|
Medicare Easyclaim |
Bulk Bill or patient |
8 |
31.1 |
8 |
31.9 |
|
Bulk Bill Webclaima |
Bulk Bill |
0.07 |
0.27 |
0.21 |
0.82 |
|
Patient Claim Webclaima |
Patient |
n/a |
n/a |
0.01 |
0.04 |
|
ECLIPSE |
Simplified Billing |
6.2 |
24.4 |
7.0 |
28.0 |
|
Simple Mail Transfer Protocol (SMTP) |
Simplified Billing |
1.5 |
6 |
1.2 |
4.8 |
|
Claiming Medicare Benefits Online (CMBO) |
Patient |
0.05 |
0.2 |
0.03 |
0.13 |
Note a: Both Bulk Bill and Patient Claim Webclaim are less established channels having been introduced in June 2015 and August 2016 respectively. See also Table 2.2 for the date each of the channels was introduced.
Source: Department of Human Services’ documentation.
3.4 The point of access to each of the eight available electronic channels differs as do the MBS service item numbers that can be claimed:
- Claims can be made at the point of service through Medicare Online, Easyclaim and the Bulk Bill/Patient Claim Webclaim channels at practices that have electronic claiming capability.
- In-hospital services can be claimed by providers and billing agents through ECLIPSE or SMTP.
- Patients can claim from any location providing access to the internet/wifi using CMBO or the Express Plus Medicare Mobile App.
- Both Easyclaim and CMBO have restrictions on the MBS items that can be claimed from those channels. All other channels accept claims for all MBS items.
3.5 When patient claims are lodged at the point of service, the patient’s claim is lodged by the provider on behalf of the customer, improving convenience to the customer. In 2016–17, 86 per cent of patient claims were lodged at point of service. Additionally, 98.7 per cent of bulk bill claims and 99.5 per cent of simplified billing claims were lodged at point of service.
Take-up by practices and provider type
3.6 Medical practices may lodge claims from multiple channels. In June 2017, 43 066 medical practices lodged claims for 34 625 336 Medicare services. Claims for more than 97 per cent of these services (around 33.8 million) were lodged electronically from 37 529 practices. 21 832 practices provided services (around 843 000) for which claims were lodged manually. Table 3.2 shows the number of practices lodging claims for services in June 2017 by lodgement channel and billing type.
Table 3.2: Medicare services claim transmission as at June 2017
|
|
Bulk billing |
Simplified billing |
Patient claiming |
|
Electronic (SMTP) |
0 |
5770 |
0 |
|
HPOS |
2294 |
0 |
299 |
|
Medicare Online |
19 065 |
0 |
13 917 |
|
Medicare Easyclaim |
10 927 |
0 |
8650 |
|
ECLIPSE |
0 |
7806 |
0 |
|
Claiming Medicare Benefits Online |
0 |
0 |
3377 |
|
Scanned |
1414 |
0 |
0 |
|
Manual |
1204 |
305 |
20 486 |
|
Total practicesa |
31 481 |
8798 |
28 552 |
|
Electronic transmitting sites for Medicare Online and Easyclaim |
|||
|
Total no. of transmitting Medicare Online sites |
22 006 |
||
|
Total no. of transmitting Medicare Easyclaim sites |
15 871 |
||
|
Total no. of transmitting HPOS sites |
2435 |
||
|
Total no. of transmitting Electronic sites (Medicare Online +/or Easyclaim) |
33 493 |
||
Note a: Totals do not sum as practices may use multiple claim transmission methods.
Source: Department of Human Services’ administrative data.
3.7 The proportion of patient claimed and bulk bill services lodged electronically varies by provider type. The data shows that all provider types are most likely to bulk bill electronically. However, as bulk billing is the most common claiming type by volume, the number of manual bulk bill claims remains high and represents more than 35 per cent of all manually lodged claims.
3.8 A majority of patient claim services are also lodged electronically by general practitioners, specialists and other providers, but not by pathologists. Only two per cent of pathology claims are patient claims with almost 93 per cent of these claims lodged manually (see Table 3.3).
3.9 Human Services advised that pathology claims are often more complex than other claims and that while current legislation does not prevent a pathologist from electronically lodging a patient claim18, knowledge of processes and software limitations have been identified by providers as barriers to electronic lodgement during consultations with Human Services Business Development Officers (BDOs). In 2015, Human Services commenced discussions with peak pathology organisations to discuss these barriers. Human Services data indicates that electronically lodged patient claiming by pathologists rose from one per cent in 2013–14 to 5.2 per cent in 2015–16 and 7.2 per cent in 2016–17.
Table 3.3: Medicare services processed by provider type and lodgement method, 2016–17
|
|
Bulk bill |
Patient claim |
||||||
|
|
Electronic |
Manual |
Electronic |
Manual |
||||
|
|
Number |
% |
Number |
% |
Number |
% |
Number |
% |
|
General Practitioner |
136 053 120 |
98.1 |
2 602 428 |
1.9 |
20 748 777 |
95.7 |
927 859 |
4.3 |
|
Specialist |
64 770 549 |
98.8 |
784 347 |
1.2 |
19 958 411 |
85.4 |
3 422 059 |
14.6 |
|
Pathologist |
84 150 884 |
100 |
25 792 |
0.0 |
113 027 |
7.2 |
1 461 225 |
92.8 |
|
All other providersa |
24 546 245 |
97.4 |
642 687 |
2.6 |
4 942 571 |
78 |
1 395 038 |
22 |
|
Total |
309 520 798 |
98.7 |
4 055 254 |
1.3 |
45 762 786 |
86.4 |
7 206 181 |
13.6 |
Note a: All other providers includes optometrists, dentists/orthodontists, other practitioners and new providers (not yet classified with a major speciality by Human Services).
Source: ANAO analysis of Department of Human Services’ administrative data.
3.10 ANAO analysis of jurisdictional data shows some differences in access to bulk bill services by state/territory and nationally by Australian Statistical Geography Standard Remoteness Structure classifications.19 In 2016–17, more than 94 per cent of all services and more than 82 per cent of all patient claim services are claimed electronically at the point of service in each state and territory. However there were variations in the proportion of electronic patient claims for services claimed at point of service by state, with New South Wales and the Australian Capital Territory having the lowest proportions at 82 per cent of services, and South Australia having the highest proportion at 95 per cent of services.
3.11 Data on claiming by region (see Table 3.4) shows that very remote and remote Australian regions have the highest proportion of point of service claiming, with 96 per cent of patient claims for services claimed at point of service in these areas. Major cities of Australia were the region with the lowest level of point of service, with 85 per cent of patient claims for services being made at point of service. These regional differences are due in part to higher proportions of bulk bill claiming in remote (87 per cent) and very remote areas (94 per cent) compared to other regions. Almost all providers who bulk bill use electronic services which will then be available for the practice to lodge the claim on behalf of the patient.
Table 3.4: Proportion of claims for patient services claimed at point of service by Australian Region in 2016–17
|
Australian region |
Proportion of claims for patient services claimed at point of service (%) |
|
Inner Regional Australia |
92 |
|
Major Cities of Australia |
85 |
|
Outer Regional Australia |
90 |
|
Remote Australia |
96 |
|
Very Remote Australia |
96 |
Source: ANAO analysis of Department of Human Services’ data.
Human Services’ initiatives to increase take-up of Medicare electronic claiming
3.12 Since 2015, several strategies have been used by Human Services BDOs to achieve as close to 100 per cent electronic claiming at the point of service as possible. Human Services uses analysis of claiming trends by practices and provider types to target practices with high volumes of manual patient claiming.
3.13 Human Services’ data demonstrates increases in electronic patient claiming rates since these strategies commenced. Overall, in December 2014, around 31 per cent of practices lodged 100 per cent of their claims electronically and by May 2017 this proportion had risen to around 45 per cent (see Table 3.5).
Table 3.5: Practices transmitting Medicare services electronically December 2014, May 2016 and May 2017
|
|
December 2014a |
May 2016 |
May 2017 |
|||
|
|
Number of practices |
Proportion of total practices (%) |
Number of practices |
Proportion of total practices (%) |
Number of practices |
Proportion of total practices (%) |
|
‘zero’ electronic practices |
9000 |
23 |
7751 |
18.3 |
6182 |
14.1 |
|
‘some’ electronic practices |
18 000 |
46 |
18 427 |
43.5 |
17 992 |
41.2 |
|
100 per cent electronic practices |
12 000 |
31 |
16 193 |
38.2 |
19 544 |
44.7 |
|
Total practices |
39 000 |
100 |
42 371 |
100 |
43 718 |
100 |
|
Practices transmitting electronically |
30 000 |
77 |
34 620 |
81.7 |
37 536 |
85.9 |
Note a: December 2014 figures are rounded.
Source: Department of Human Services’ administrative data.
3.14 Human Services data also demonstrates improvements for targeted provider types, for example:
- from January to June 2015 targeted practices increased electronic patient claiming by four per cent, while the increase in non-targeted sites was only 1.1 per cent; and
- electronic patient claiming in target sites rose from 44.3 per cent in December 2015 to 68.1 per cent in April 2017.
3.15 Targeting of specialists (by BDOs) led to growth in electronic claiming from around 21 per cent in 2012 to around 85 per cent in 2017 (see Table 3.6).
Table 3.6: Practices transmitting patient claims electronically, March 2012, 2016 and 2017
|
Patient point of service claims |
FYTD ending |
FYTD ending |
FYTD ending |
Increase |
||||
|
|
number |
% |
number |
% |
number |
%
|
number |
% |
|
Totala |
14 859 033 |
34.8 |
32 229 192 |
81.3 |
34 113 693 |
85.9
|
19 254 660 |
51.1 |
|
by General Practitionersb |
10 205 002 |
55.0 |
15 843 739 |
93.8 |
15 674 641 |
95.5 |
5 469 639 |
40.5 |
|
by Specialistsb |
3 712 646 |
21.2 |
13 566 128 |
78.4 |
14 842 231 |
84.7 |
11 129 585 |
63.5 |
Note a: Total includes claims submitted by all providers. Percentage refers to proportion of claims that were patient claims.
Note b: Percentages refer to the proportion of electronic claims submitted by the relevant provider type.
Source: Department of Human Services’ documentation.
3.16 Human Services has developed several new strategies to support engagement by BDOs to increase point of service claiming. Business proposals indicate that these strategies will target different cohorts not covered by previous strategies and are intended to provide education and support to transition to the most appropriate digital channel. These strategies, which commenced in 2017, are:
- Allied Health Engagement Strategy;
- Manual to Digital Bulk Bill transition; and
- Digital Claims Realisation 1 and 2.
3.17 To support these strategies Human Services undertook analysis of claiming trends. That analysis identified that allied health providers submitted 98 357 manual patient claims in November 2016, around 25 per cent of all patient claims for this group and around 13 per cent of the total manual claims for all groups and claiming channels over the timeframe. Further analysis conducted by Human Services identified that dentists/orthodontists submit a majority of their claims manually and have therefore been included as a target group in the Allied Health Engagement Strategy.
3.18 The Manual to Digital Bulk Bill transition strategy focuses on practices that continue to exclusively lodge claims manually. When developing the strategy the department identified that in the month of October 2016, 4561 practices were lodging manual bulk bill claims and of these, 2754 (60 per cent) lodged only manual bulk bill claims.
3.19 Finally, the Digital Claims Realisation strategies (DCRS 1 and 2) will involve BDOs, data analysis, and reporting. DCRS 1 will involve practices that submitted 100 or more manual patient claims in March 2017 and DCRS 2 will engage practices who submitted 50–99 manual patient claims. These sites are primarily comprised of specialists and some general practitioners.
3.20 These strategies are in addition to government and departmental strategies undertaken over the years to promote electronic claiming, including subsidies and the removal of cash and cheque payment services (see Appendix 3).
Have the costs and savings from delivering electronic claiming been realised and tracked over time?
Given that Human Services has achieved 97.1 per cent electronic claiming at an aggregate level it is expected that savings to the department have been realised overall. The costs associated with introducing and maintaining these electronic claiming channels have not been tracked over time and the expected savings from introducing individual channels have not been realised within anticipated timeframes.
Anticipated savings for each channel have been estimated using standard assumptions of the price differential between manual and electronic claiming and projected channel take-up rates. The department has consistently overestimated the take-up rates when introducing new channels and has not followed up to determine whether the cost savings for individual channels have been met.
Human Services does not currently track the relative costs of maintaining each claiming channel. There would be benefit in Human Services developing the capability to better understand the costs of each channel, as well as the administrative savings and other benefits that have been realised, to support decisions about future directions for, and investments in, electronic claiming.
3.21 One of the objectives of introducing electronic claiming is to achieve cost and administrative savings for government (as discussed previously in paragraph 2.3). These savings can be achieved through reductions in manual claims processing, including efficiencies gained from reducing points of contact between the department, providers and patients.
3.22 It is likely that, at an aggregate level, the department has realised administrative savings. Between 2002–03, when Medicare Online was first introduced, and 2016–17, the number of claims for services lodged manually reduced from 98.4 million to 11.4 million. This reduction has occurred alongside an overall increase of 178.1 million services claimed over this time period. The uptake of electronic claiming also occurred against a backdrop of greater access to information technology and communications infrastructure.
3.23 A review of Medicare electronic claiming undertaken by the department in 2009 stated that the take-up of electronic claiming had, to date, not been sufficient to realise savings and that it was unlikely to achieve a return on the investments until 2010–11 when it expected take-up in the order of 30 per cent for patient claiming and 93 per cent for bulk billing. These take-up rates were achieved within this timeframe as shown in Figure 3.1.
Figure 3.1: Percentage of Medicare claims lodged electronically 2010–11 to 2016–17
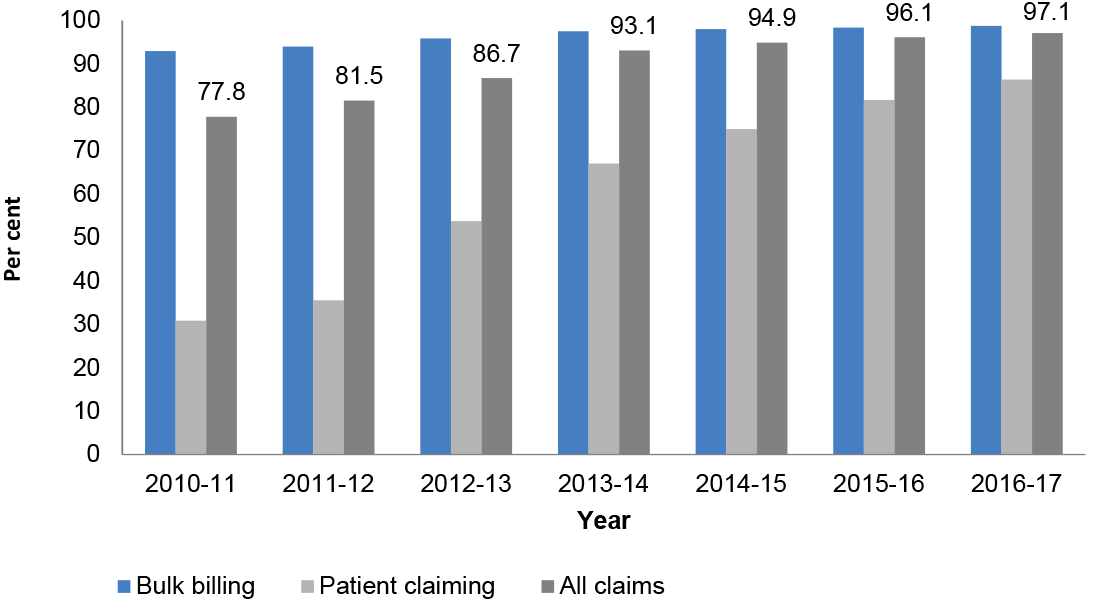
Source: ANAO analysis of Department of Human Services’ Annual Reports (2010–11 to 2016–17).
3.24 When introducing individual channels Human Services has consistently over-estimated take-up rates, and under-estimated implementation challenges. Some of the increase in take-up of individual channels likely represents a shift between electronic channels in addition to a shift from manual to electronic claim lodgement. These factors have contributed to anticipated savings for individual channels not being achieved in the timeframes originally planned.
Savings and other benefits from individual claiming channels
3.25 For the three oldest current channels: Simple Mail Transfer Protocol (SMTP) (implemented in 1999), Medicare Online (implemented in 2002); and ECLIPSE (implemented in 2004), Human Services was unable to provide documentation which identified the intended objectives and savings expected from these claiming channels. Human Services also advised that documentation was not developed to support the implementation of the Express Plus Medicare Mobile App in 2013. For those electronic claiming channels for which documentation has been available, the ANAO has assessed whether the expected savings from claiming channels were identified and have been achieved.
Webclaim
3.26 Bulk Bill Webclaim, and Patient Claim Webclaim, implemented in 2015 and 2016 respectively, are Human Services’ two most recently implemented claiming channels. The key objective of the Webclaim channels was to deliver a lower cost option via the existing Health Professional Online Services to those practices for whom implementing a vendor product is not financially viable.
3.27 The sole measure of success for the Bulk Bill Webclaim program was identified in internal documentation to be the delivery of savings which were originally (in February 2014) estimated to be around $22.3 million and later re-forecasted by Human Services to be around $10.8 million in late 2015.
3.28 A separate estimate of the regulatory impact of implementing Bulk Bill Webclaim was undertaken by the department in 2015. The estimated regulatory saving of $16.8 million annually for health providers was based on reductions in compliance costs from moving from paper-based to online claiming. This estimated saving was reported in the Government’s Annual Red Tape Reduction Report 2015.
3.29 Following the implementation of Bulk Bill Webclaim, Human Services internally reported in its project closure report that the project delivered all in-scope items and successfully met its objectives. The closure report highlighted that the implementation of the project had achieved savings however the value of these savings were not quantified. Subsequent information provided by the department identified that a number of factors affected full benefits realisation for the introduction and use of Bulk Bill Webclaim. Human Services advised that these factors included legal concerns expressed by software vendors and delays in system development that impacted the launch of the channel.
3.30 Patient Claim Webclaim was introduced as part of a suite of initiatives that formed the ‘Increasing Digital Health Transactions’ strategy, aimed at increasing the volume of digital claiming. Human Services projected that administrative savings to the department resulting from these initiatives would be $81 million over four years commencing in 2015–16. Internal Human Services documentation did not clearly specify whether these projected savings were expected solely from the implementation of the channel or from other initiatives included in the proposal. The expected savings, whether from the channel or from the suite of initiatives, were to be driven by an overall reduction in the remaining manual patient claim services. These reductions were over-estimated.
3.31 Table 3.7 shows the expected take-up rate and savings projected by Human Services as part of costing the Increasing Digital Health Transactions strategy. The projected savings for the strategy from 2015–16 to 2018–19 was based on a flawed methodology. The projected patient claim service figures were based on 2013–14 data and did not account for the downward trend in manual transactions already occurring. The fact that the projected take-up was for electronic claiming as a whole, rather than for the new channel, also meant that the benefits from introducing Patient Claim Webclaim would be less clearly known. In addition, the savings were calculated by multiplying the expected volume of new electronic claims by $1.61 per claim. This value was used by Human Services as the assumed cost differential between processing manual claims and electronic claims.
Table 3.7: Expected uptake and savings from Patient Claim Webclaim 2015–16 to 2018–19
|
Number |
2015-16 |
2016-17 |
2017-18 |
2018-19 |
Total |
|
Projected Manual Patient Claim Services |
17 755 824 |
17 755 824 |
17 755 824 |
17 755 824 |
|
|
Potential uptake of electronic claiming |
7 102 330 |
11 718 844 |
14 559 776 |
17 045 591 |
|
|
Remaining Manual Patient Claim Services |
10 653 494 |
6 036 980 |
3 196 048 |
710 233 |
|
|
Calculated savings |
$11 434 751 |
$18 867 339 |
$23 441 239 |
$27 443 402 |
$81 186 730 |
Source: ANAO analysis of Department of Human Services’ documentation.
3.32 The Patient Claim Webclaim channel was implemented on August 2016, two months later than initially indicated in the project management plan. In 2016–17, 43 725 claims were made using Patient Claim Webclaim.
3.33 Following the implementation of Patient Claim Webclaim Human Services internally reported in its project closure report that the project delivered all in-scope items and successfully met its objectives. The closure report identified that no direct savings were associated with the introduction of Patient Claim Webclaim.
Claiming Medicare Benefits Online
3.34 The objective of Claiming Medicare Benefits Online (CMBO) was to support the take-up of electronic Medicare claiming by developing and implementing an alternative, home-based, electronic channel for members of the public who either do not have the opportunity, or choose not to, use point of service claiming. The CMBO channel was also intended to reduce the manual channel servicing costs within the portfolio and generate savings of $6.6 million over four years. These savings were calculated based on the estimated take-up of CMBO claiming over the four year period multiplied by the unit price per claim of $1.61.
3.35 While the implementation of CMBO achieved its objective of providing an internet-based Medicare claiming solution, lower than expected take-up rates have resulted in expected savings not being achieved. In addition changes made to the delivery of the channel, to mitigate identified compliance risks (see paragraph 4.28), have led to all claims for this channel now being manually processed, making the channel less efficient that initially intended.
3.36 During its first year of implementation, CMBO exceeded its expected take-up rate by nearly 9000 claims; however, the increase in take-up in subsequent years was far below projections. Table 3.8 shows the expected and actual take-up and savings for Claiming Medicare Benefits Online.
Table 3.8: Projected and actual claim rate and savings for the Claiming Medicare Benefits Online channel, 2011–12 to 2014–15
|
Financial year |
Expected Take-up |
Projected claim rate |
Projected savings |
Actual claim ratea |
Estimated savingsb |
|
2011–12 |
0.2% |
124 228 |
$200 007 |
133 000 |
$214 130 |
|
2012–13 |
0.5% |
424 430 |
$683 332 |
211 200 |
$340 032 |
|
2013–14 |
2.0% |
1 531 249 |
$2 465 310 |
251 500 |
$404 915 |
|
2014–15 |
3.3% |
2 018 546 |
$3 249 859 |
352 400 |
$567 364 |
|
Total |
|
4 098 453 |
$6 598 508 |
948 100 |
$1 526 441 |
Note a: The actual claim rate has been determined using figures reported in Human Services’ Annual Reports.
Note b: The estimated savings have been calculated by multiplying the actual claim rate by the unit price of $1.61 which is the assumed price used by Human Services since 2011.
Source: ANAO analysis of Department of Human Services’ documentation.
3.37 The lower than expected take-up of CMBO was noted in Human Services’ internal project management reporting. Human Services identified that the projected uptake was impacted by limits deliberately placed on the number of eligible items that could be claimed through CMBO. The department noted that remedial action to address CMBO claiming rates would require promotion of the claiming option to the general public. This action was not considered a priority for the department however because it was focused on encouraging point of service claiming. The actual take-up of CMBO as a proportion of total patient claiming at 30 June 2017 was 0.2 per cent, the same as that projected in 2011–12.
3.38 To further strengthen controls to prevent fraud, the automatic payment of claims made using CMBO were ceased and from 31 January 2016 onwards, claims lodged using CMBO were processed manually rather than automatically. This channel has daily and monthly cash limits. Manual intervention allows Human Services to ensure the claiming limit has not been exceeded prior to releasing payment. This move from automatic processing to manual processing for CMBO claims means that the level of ongoing savings initially expected from shifting from manual claiming to electronic claiming through the implementation of the CMBO channel have not been realised.
Easyclaim
3.39 The objective of Easyclaim was to improve doctor and patient convenience by providing faster access to Medicare benefits, reducing paperwork and removing the need for patients to visit Medicare offices to claim benefits. Easyclaim was also intended to improve the administrative efficiency of the Medicare claiming and payment system generating cumulative gross savings of $76.88 million by June 2009 for the department. The savings were estimated based on an expected claiming take-up rate of 70 per cent, equating to an expected 250 million Easyclaim claims being achieved by June 2009. The actual take-up of Easyclaim was much lower than expected. In 2008–09 only six million Medicare claims (five per cent of total claims) were made using the Easyclaim channel. The lower than expected take-up resulted in a shortfall in projected savings for the period from 2006–07 to 2008–09 of $24.7 million. As shown in Table 3, the take-up of Easyclaim has remained significantly lower than the 70 per cent of total claims expected—with Easyclaim claims having plateaued at approximately eight per cent of total claims since 2014–15.
Table 3.9: Volume of Easyclaim claims as a proportion of total Medicare claims between 2007–08 and 2016–17
|
Financial Year |
Volume of Easyclaim claims (millions) |
Easyclaim claims as a percentage of total claims (%) |
|
2007–08 |
1.13 |
0.4 |
|
2008–09 |
6.00 |
2 |
|
2009–10 |
14.90 |
5 |
|
2010–11 |
20.70 |
6 |
|
2011–12 |
24.00 |
7 |
|
2012–13 |
25.00 |
7 |
|
2013–14 |
24.60 |
7 |
|
2014–15 |
29.10 |
8 |
|
2015–16 |
31.10 |
8 |
|
2016–17 |
31.9 |
8 |
Source: ANAO analysis of Department of Human Services’ Annual Reports (2007–08 to 2016–17).
3.40 Since inception a transaction fee of 23 cents has been paid by the government to financial institutions for each successfully delivered Easyclaim transaction, which currently equates to $6.6 million per year. The transaction fee was initially intended as an incentive to attract as many financial institutions as possible to participate in the channel, with the expectation that the Easyclaim channel would eventually replace the Medicare Online channel. The transaction fee was determined on the assumption that if the expected claim take-up was achieved within the first two years, the upfront development and testing costs incurred by acquiring financial institutions would be recovered. The lower than expected take-up of Easyclaim impacted on financial institutions’ ability to recover the cost of their investments.
3.41 Schedule one of the contracts between Human Services and the five financial institutions contracted to deliver Easyclaim services require the institutions to perform certain activities as part of the transmission of a successful transaction. The Human Services’ ICT Service Level Agreement (SLA) for Medicare Easyclaim covers arrangements between the ICT and Business branches for the provision of the Medicare Easyclaim ICT Business Service and sets the standards that financial institutions have to meet (for example, service availability targets and service response time targets). The department advised that ongoing maintenance costs were expected to be borne by the financial institutions.
3.42 Human Services was required, in accordance with the agreement between the department and financial institutions providing Easyclaim services, to review and make a decision on whether to continue or alter the transaction fees paid to financial institutions for the period beyond 1 July 2010 to 2015, and later for the period beyond July 2015. The result from both reviews was a decision to maintain the 23 cent fee.20
3.43 The 2014 Transaction Fee Review of Medicare Easyclaim found that in comparison to other electronic channels, Medicare Easyclaim was expensive and had no real development capacity for more complex claiming processes due to the limitations of the EFTPOS network. The review also identified that the department had planned to conduct an assessment of the Easyclaim channel to consider costs, convenience to users and the flexibility to respond to developments in health policy. The review recommended that both the decision as to whether to make changes to the 23 cent transaction fee and more broadly review Easyclaim should be deferred due to a 2014–15 Budget announcement that the market testing of a commercially integrated health payment system was to commence.
3.44 The proposed market testing of the new health payment system did not negate the need for a review of Human Services’ administration of the Medicare Easyclaim channel. The planned assessment to consider costs, convenience to users, and whether Easyclaim has the flexibility to respond to developments to health policy was still warranted. In any case, the proposed market testing announced as part of the 2014–15 Budget did not eventuate.
3.45 In May 2017, Human Services briefed its Minister on the department’s intention to commission an external review of the financial arrangements for the Easyclaim service. The brief identified that there was significant cost to the department from reconciling held payments lodged through Medicare Online. Payments are held when a provider or patient has failed to provide or update their bank account details. The brief identified that a benefit of Easyclaim over Medicare Online is that there are no held payments. The brief outlined that the review of the financial arrangements for Easyclaim would quantify the benefit of this channel, especially in relation to the issue of reconciling held payments.
3.46 The draft review focused on the Easyclaim financial arrangements and determining the impact of removing or changing the transaction fee. The review did not quantify the benefits of Easyclaim in relation to the issue identified in paragraph 3.45. Rather, it identified that the cost to the department in providing Medicare Online cannot currently be easily quantified as resources to deliver the channel are shared across multiple services, making accurate cost allocation difficult. The review concluded that while the transaction fee may be appropriate in the context of the department’s electronic claiming policy, the department’s alternative electronic claiming channels are provided at a lower cost to the department than Easyclaim and so Easyclaim does not represent the most efficient means by which the department can provide digital payment services in its current format.
3.47 Given that Easyclaim has not met original expectations in terms of take-up rates and the department has previously identified that the channel is expensive, understanding the relative benefits of this claiming channel in comparison to others would be useful in order to support decisions about future directions for electronic claiming.
Costs of electronic claiming channels
3.48 The ongoing administrative costs to the department for maintaining electronic claiming channels and to providers are not tracked. The administrative budget for the branch responsible for the delivery of Medicare electronic claiming channels was around $12 million in 2016–17. Other administrative costs include ICT business maintenance and eBusiness costs. Recent electronic claiming channels have been introduced as projects but continue to be funded as Business As Usual (BAU). The department’s reporting requirements for BAU activities do not require the monitoring of ongoing costs and Human Services was unable to provide the ANAO with information regarding these costs to the department.
3.49 The current processing costs of individual claiming channels are not known by Human Services.21 The department has assessed the difference in the cost of processing a manual claim as compared to a digital claim to be $1.61 cents, regardless of the claim type. This assumption has been used since at least 2011 to estimate savings expected from the implementation of some claiming channels.
3.50 In 2004, Human Services developed an Activity Based Costing model designed to use multiple data sources to determine program and channel expenses for Medicare. This model was developed in response to a need identified both in an internal review and by Government that the department should undertake regular activity costing to provide further transparency for channel costs. The main report produced using the costing model was a Program and Channel Expenses Report. This report provided a range of cost information about Medicare Australia’s services including the costs involved in delivering Medicare claims. The report included data showing service delivery full time equivalent (FTE) staffing levels, service volumes, fixed and variable expenses and expenses per service by claim type and lodgement. The reporting of service and channel costs was discontinued after the integration of Medicare, Centrelink and the Child Support Agency into Human Services in 2011. The final program and channel expenses report was prepared using 2010–11 data.
3.51 Table 3.10 contains data presented in the 2010–11 Program and Channel Expenses Report22 which shows how the relative costs of claiming by channel have changed over time.
Table 3.10: Cost per service of Medicare claiming channels between 2006–07 and 2010–11
|
Claim Type and Lodgement Channel |
|
Expense per service ($) |
||||
|
|
|
2006–07 |
2007–08 |
2008–09 |
2009–10 |
2010–11 |
|
Patient claim |
Manual |
|
|
|
|
|
|
4.37 |
3.81 |
4.39 |
5.18 |
5.45 |
|
|
4.60 |
5.17 |
7.70 |
9.68 |
10.21 |
|
|
- |
- |
|
2.87 |
3.33 |
|
|
- |
- |
- |
3.57 |
6.54 |
|
|
Easyclaim |
- |
12.63 |
1.71 |
0.68 |
0.27 |
|
|
Medicare online |
0.52 |
0.73 |
0.29 |
0.53 |
0.71 |
|
|
Bulk bill |
Manual |
1.36 |
1.52 |
5.05 |
5.12 |
5.52 |
|
Electronic Claim (EDI) |
0.31 |
0.41 |
0.40 |
5.72 |
0.66 |
|
|
Scan |
0.31 |
0.35 |
0.43 |
0.29 |
0.42 |
|
|
Easyclaim |
- |
9.50 |
0.18 |
0.30 |
0.29 |
|
|
Medicare Online |
0.28 |
0.31 |
0.18 |
0.16 |
0.18 |
|
Source: Medicare Master Program—Program and Channel Expenses Report 2010–11 p. 17.
3.52 The data showed that the two main electronic claiming channels, Medicare Online and Easyclaim, had significantly lower costs per service than the cost per service for processing a claim manually. The data also identified changes in comparative costs of Easyclaim and Medicare Online over time. In 2009–10, Medicare Online cost 14–15 cents less per service than the Easyclaim channel. In 2010–11, Medicare Online for bulk bill services cost 11 cents less than Easyclaim per service but for patient claims, Easyclaim was 44 cents less per service than Medicare Online. It was unclear in departmental reports whether the costs attributed to Easyclaim included the 23 cent transaction fee paid to financial institutions. The relative differences between Medicare Online and Easyclaim processing costs are considered by Human Services to have been a point in time issue that has been addressed through enhancements made to Medicare Online over time.
3.53 In late 2014 Human Services developed an eClaiming and Payments strategy, which outlined a way for the department to transform the way it services the community and the health care sector, while creating efficiencies and allowing for a more automated approach to service delivery. This strategy acknowledged that decommissioning some claiming channels would create efficiencies for the department and reduce the choices that health professionals are faced with when trying to take-up electronic patient claiming. The strategy made five recommendations including conducting a full review of claiming and payment channels to determine what systems should continue to be supported into the future and to undertake cost analysis into savings were the department to decommission particular claiming channels. Human Services has advised that this strategy was not endorsed and that the recommendations were not implemented.
3.54 More recently in July 2016, the business unit responsible for Medicare electronic channel management again identified there would be benefit in developing the capability to obtain separate prices per claim type such as bulk bill, patient claims and simplified billing, and per claim channel such as Medicare Online, ECLIPSE, Easyclaim and Manual. However to date, this analysis has not been undertaken. Human Services’ finance area further advised that it is currently developing cost modelling to better attribute costs at the service level. This modelling may incorporate the channel level in the future.
Has electronic claiming improved processing and payment timeliness?
Electronic claiming allows for increased automation of processing and payment of Medicare benefits and has improved timeliness. Not all electronic claims are able to be processed automatically. Human Services continues to make system enhancements to reduce the amount of manual intervention required.
3.55 One of the intended benefits of introducing electronic claiming was to improve the speed of claims processing (see paragraph 2.3). Electronic claiming improves claim processing time because claims are automatically assessed against system business rules. Electronic bulk bill and patient claims that meet the relevant business rules are paid in the next available payment run, usually overnight or early the next day. When claims are processed manually, they require a Human Services’ officer to make an assessment of the claim against the business rules. The time required to manually process a claim varies depending on the complexity of the claim.
3.56 The introduction of electronic claiming has led to a reduction in the volume of claims for services that require manual processing and consequently departmental costs associated with manual claiming are likely to have been reduced. When patient claims are lodged at point of service, the patient’s time is saved because they are not required to lodge their claim themselves, either at a Medicare office, over the phone or online. In 2016–17, around 86 per cent of patient claims for services were made at the point of service. The proportion of patient claims lodged at point of service has increased 30 per cent since 2012–13 when only 56 per cent of patient claims were lodged at point of service.
3.57 Human Services’ Key Performance Indicator (KPI) for measuring achievement in processing service levels for the Medicare program is for 82 per cent or more of health claims to be processed within standard time frames. This indicator was introduced in 2014–15, and Human Services reported achieving this KPI in both 2014–15 and 2015–16 with results of 98.7 per cent and 99.3 per cent respectively. This KPI combines the results of processing the timeliness of electronically lodged claims and manually lodged claims into a single indicator. Human Services has advised that the standard used to measure this KPI is for 90 per cent of relevant claims to be processed within a minimum number of days. The target for the number of days is different depending on the way the claim is received and the way the claim is paid.
3.58 Data on the number of days it takes to process claims lodged by different claiming channels shows that the majority of claims lodged at point of service are processed within one day of lodgement. In 2016–17, 99 per cent of patient claims lodged electronically at point of service and 67 per cent of bulk bill claims lodged at point of service were processed within one day of lodgement, results that outperform manual processing (see Table 3.11). In comparison only 48 per cent of patient claims and 2 per cent of bulk bill claims for services lodged manually were processed within one day of lodgement. Additional analysis conducted by the ANAO showed that the median processing time between lodgement and payment for one category of manual bulk bill claims (Direct Bill Manually lodged) ranged from five to eight days between 2013–14 and 2015–16. In 2016–17 this timeframe had tripled to 24 days. The timeframe between lodgement and payment of manual patient claims also increased from one day to three days from 2015–16 to 2016–17. The department should monitor manual processing timeframes to determine whether the 2016–17 results indicate an exception or emerging issue. Human Services advised that early indications are that there has been a reduction in average handling times for manual bulk bill claims in the first quarter of 2017–18.
Table 3.11: Proportion of total services processed within one day by claiming channel
|
Patient Claims |
Total services |
Total services processed within one day |
Percentage of total services processed within one day (%) |
|
Bulk bill claims |
|||
|
Total lodged at point of service |
309 520 798 |
207 274 016 |
67 |
|
20 145 587 |
20 060 563 |
100 |
|
820 897 |
820 150 |
100 |
|
288 554 314 |
186 393 303 |
65 |
|
Total lodged manually |
4 055 254 |
73 905 |
2 |
|
Patient claims |
|||
|
Total services lodged at point of service |
45 632 259 |
45 174 192 |
99 |
|
11 816 688 |
11 827 828 |
100 |
|
43 725 |
43 710 |
100 |
|
33 771 846 |
33 302 654 |
99 |
|
Total services lodged electronically by customerb |
130 527 |
42 912 |
33 |
|
Total services lodged manuallyc |
7 206 182 |
3 443 611 |
48 |
Note a: There are a number of factors that are likely to have contributed to the proportion of Medicare Online claims processed within one day of lodgement being lower than other point of service claim types. The majority of bulk bill claims for services (92 per cent) are lodged using this channel. In addition, multiple services can form one claim. If one of the services is unable to be automatically processed then all the services lodged within the claim will pend until the service is manually assessed.
Note b: These services were lodged using Claiming Medicare Benefits Online.
Note c: Services lodged manually include services lodged using the Express Plus Medicare Mobile App.
Source: ANAO analysis of Department of Human Services’ data.
3.59 Not all claims that are lodged electronically are automatically processed. The complexity of business rules for receiving Medicare services can mean that some claims that have been lodged at point of service are flagged in the system and require a Human Services officer to verify the claim information. In addition all claims lodged using two of the electronic patient claiming channels are manually processed. These aspects of timeliness are discussed further in the remaining sections of this chapter.
Claims electronically lodged and manually processed
3.60 Claiming Medicare Benefits Online (CMBO) and the Express Plus Medicare Mobile App are claiming channels which allow patients to electronically lodge their patient claims. These claims are lodged by the patient after they have received a service rather than at the medical practice at point of service. While these claims are lodged electronically, the processing of these claims is completed manually by a Human Services processing officer.
3.61 Claims made using the CMBO channel were both lodged and processed electronically when the channel was introduced however, from 31 January 2016, Human Services implemented system changes to the CMBO channel which mean that these claims are now manually processed (see also paragraph 3.35). As further discussed in paragraph 4.28, this change was initiated by Human Services to help mitigate a fraud risk identified by the department for this channel. As shown in Table 3.12, this change has impacted on the average time taken to process CMBO claims, which has increased from zero days between 2012–2013 and 2014–15 to 2.6 days in 2016–17.
Table 3.12: Average time in days between lodging and processing a claim using the Claiming Medicare Benefits Online channel
|
|
2012–13 |
2013–14 |
2014–15 |
2015–16 |
2016–17 |
|
Claiming Medicare Benefits Online |
0 |
0 |
0 |
0.97 |
2.6 |
Source: ANAO analysis of Department of Human Services’ data.
3.62 Manual processing has always been required for claims lodged using the Express Plus Medicare Mobile App channel. Human Services advised that the Express Plus Medicare Mobile App requires patients to key information into the App about the claim. However, Human Services is unable to use this information to assess the claim. Processing a claim lodged through the App requires a Human Services Officer to rekey information contained in the image of the receipt for the service submitted with the claim.
Pended claims
3.63 A ‘pended’ claim is an electronically lodged claim that requires manual intervention by a Human Services’ Officer to be processed. All claims made using the Claiming Benefits Online channel are ‘pended’. In addition, some claims lodged using the electronic point of service channels are also pended. Some of the reasons these claims are ‘pended’ are due to the complexity of the relevant business rules that relate to the claim type, in particular for pathology claims, or because the system is not configured to process the claim automatically. Examples of common causes of pended claims include:
- Medicare Benefits Schedule item rule requirements not met;
- duplicate claims being received;
- registration or eligibility issues (for example the provider’s eligibility may have lapsed); and
- reaching the maximum number of services within a specified time frame.
3.64 Human Services has implemented a range of projects to address the high percentage of pended claims. In January 2012, Human Services established the Reduction in Manual Intervention (RIMI) Project to identify opportunities to streamline the processing of digital claims by reducing the amount of manual intervention required in digital claiming. The RIMI project has been conducted over a number of phases which have sought to identify opportunities to reduce the need for manual intervention and improve the accuracy of processing through automation through both IT enhancements and educational opportunities. Human Services has identified that the number of claims that pend impacts on the department’s capacity to meet internal key performance indicators for processing digital claims. The objectives of the current RIMI strategy are to:
- reduce pended claims;
- deliver cost savings to the government;
- increase the consistency in processing across the eClaiming channels;
- improve digital Medicare claiming workflow process; and
- create greater capacity to meet KPIs by reducing staff effort required to process pended digital claims.
3.65 Currently, Human Services is only able to report pend data at a claim level rather than a service level. As noted at paragraph 1.5, one claim may be made up of multiple services, meaning that the total volume of claims is lower than the total volume of services provided. Data collected by Human Services shows that, over time, the volume of pended claims has been reducing (see Table 3.13).
Table 3.13: Volume and percentage of pended claims as a proportion of total claims
|
|
2013–14 |
2014–15 |
2015–16 |
2016–17 |
|
Pended claims |
10 219 554 |
9 074 424 |
6 738 647 |
7 310 329 |
|
Total Claims |
67 558 260 |
74 942 701 |
73 674 789 |
85 005 893 |
|
Claims pended as a percentage of total claims |
15.1 |
12.1 |
9.1 |
8.6 |
Source: Department of Human Services’ documentation.
3.66 Human Services currently reports on the volume and percentage of digital claims that have been pended during the month, broken down by claim processing type. The data shows that the rate of claims pending is also impacted by the type of service being provided. Table 3.14 shows the volume and percentage of pended claims received by claim type for the month of June 2017.
Table 3.14: Volume and percentage of pended claims by claim type for June 2017
|
|
Volume of claims received |
Volume of claims pended |
Claims pended as a percentage of claims received (%) |
|
Bulk billing Pathology |
65 621 |
45 934 |
70 |
|
Bulk billing Other |
2 730 278 |
323 209 |
12 |
|
Patient claiming |
3 556 589 |
105 570 |
3 |
|
Simplified billing |
1 041 846 |
95 541 |
9 |
|
Online Claims Total |
7 394 334 |
570 254 |
8 |
Source: Department of Human Services’ documentation.
3.67 In total, 70 per cent of all bulk bill pathology claims made were pended in June 2017. In addition, while bulk bill pathology claims made up less than one per cent of total online claims, eight per cent of all claims that pended were bulk bill pathology claims. Bulk bill pathology claims are complex to process as the system has not been enhanced to automate many of their complex business rules. Human Services is engaging with the Department of Health to look for opportunities to reduce the high pend rate for pathology.
Average handling time for processing claims manually
3.68 The average time it takes to process a claim requiring manual intervention (referred to as the average handling time) varies depending upon the number and complexity of errors in the claim. Human Services does not currently know the average handing times for processing different types of manual claims. In 2014, Human Services undertook a small time and motion study that indicated that the time taken to process an Express Plus Medicare Mobile App claim with an electronic receipt is 4.45 minutes compared to 3.33 minutes to handle the claim manually. This additional time was due to the often poor quality of the receipt image from which the information needs to be entered. There are no more recent comparisons between the app, Claiming Medicare Benefits Online and straight manual claim handling times.
3.69 Human Services advised that the department has commenced benchmarking activity for some work types, however as it is in its early stages there is no documentation yet available. Human Services advised that this activity:
could at some point in the future feed into a review to determine the average handling times for Medicare processing, including Claiming Medicare Benefits Online, manual claims and Medicare Express Mobile App claims.
4. Monitoring and reporting
Areas examined
This chapter examines the monitoring and reporting mechanisms used by Human Services to inform channel delivery, how risks and issues are managed and identifies the department’s role in the development of the ‘Modernising Health and Aged Care Payments Services Program’.
Conclusion
Human Services’ monitoring and reporting includes business analytics used to inform channel delivery, and departmental management of risks and issues are supported by a range of plans. The department’s delivery of claiming channels is not supported by either: benchmarking of expected achievements; or a full understanding of the costs and benefits of individual claiming channels. There is a lack of information on whether the development of individual channels has delivered the intended administrative savings; and whether the savings achieved have outweighed the costs of introducing new channels. As such the department has not established a sufficiently strong information base to inform its business decisions.
Area for improvement
The ANAO made one recommendation aimed at improving the department’s understanding of the administrative costs and benefits of individual electronic claiming channels and at improving the department’s ability to deliver electronic claiming efficiently.
Has Human Services established relevant regular monitoring and reporting mechanisms to inform channel delivery?
Human Services has established relevant monitoring and reporting against its objective of attaining as close as possible to 100 per cent electronic claiming at the point of service. These reporting mechanisms inform the department’s electronic claiming strategy. The department also monitors user satisfaction and service availability—information that can be used to highlight areas of improvement.
The department’s monitoring and reporting on channel delivery does not cover all relevant aspects of electronic claiming service delivery. The department does not monitor the ongoing administrative costs and benefits of individual channels and therefore has an incomplete understanding of the performance of each channel against their respective business objectives.
Management information and reporting
4.1 Human Services monitors and reports on claiming trends including a range of information that informs an understanding of provider and patient take-up of electronic claiming. This activity includes recording:
- monthly use of electronic claiming overall and broken down by claim type, provider group and channel (see from paragraph 3.3);
- monthly processing timeliness (see from paragraph 3.55);
- monthly channel usage by individual providers and practices; and
- daily system disruptions/outages affecting channel availability (see paragraphs 4.30–4.32).
4.2 This reporting is used to measure performance against the department’s overall objective of attaining as close as possible to 100 per cent electronic claiming rates and to develop the engagement models to be used by Business Development Officers that target practices to increase the take-up of electronic claiming.
4.3 Management information on each of these four categories of information is reported to the department’s Executive through a number of Committees. Information is generally presented to these Committees in the form of dashboards which provide at-a-glance visualisation of data relevant to performance. Management information is also used in briefings to both the department’s Executive and Minister as required.
4.4 In 2014, the department introduced a Benefits Realisation Framework intended to identify financial benefits as well as elements of efficiency and effectiveness. The department advised that reporting is conducted quarterly to Senior Executive Committees, including the Finance and Investment Committee. The department further advised that this framework ‘continues to gain maturity.’
4.5 The Medicare Programme and Related Programmes Agreement 2015–2018 between Human Services and the Department of Health (Health) sets out the governance arrangements between the two entities as well as reportable performance information for the Medicare Program and data to be provided to each of the entities by the other. Governance arrangements between Human Services and Health include participation in regular Operational and Management Committee meetings. There is evidence of regular interaction between the two entities, with decisions made by one Committee put forward for action or consideration by the other Committee. The ANAO did not undertake an assessment of the data and information provided to Health.
Public performance reporting
4.6 Human Services’ Portfolio Budget Statement identifies 14 Key Performance Indicators (KPI) under Programme 1.2 Services to the Community–Health. Broadly these KPIs relate to:
- user satisfaction levels (assessed through surveys);
- the number of electronic interactions completed relative to the previous year;
- service availability (including phone response times); and
- processing timeframes.
4.7 One of these KPIs, introduced in 2015–16, applies exclusively to electronic claiming (Medicare Benefits Schedule digital claiming rate), and most of the remaining 13 KPIs are likely to be influenced directly by increases in electronic claiming. The current KPIs, relevant targets and results for 2015–16 and 2016–17 are set out in Table 4.1.
Table 4.1: Key Performance Indicators
|
Indicator |
Description and target |
Result |
|
|
|
|
2015–16 |
2016–17 |
|
Exclusive to electronic claiming |
|||
|
Medicare Benefits Schedule digital claiming rate |
The percentage of Medicare claimed services lodged electronically across all digital Medicare services channels (≥ 96%). |
Met—96.1% |
met—97.1% |
|
Indicators that electronic claiming contributes to |
|||
|
Satisfaction with Medicare Provider service delivery: Practitioners |
The percentage of General Practitioners who are satisfied or neutral with the service they receive from the department (≥ 70%). |
Met—91% |
met—89% |
|
Satisfaction with Medicare Provider service delivery: Practice managers |
The percentage of practice managers who are satisfied or neutral with the service they receive from the department (≥ 70%). |
Met—87% |
met—82% |
|
Satisfaction with Medicare Provider service delivery: Pharmacists |
The percentage of pharmacists who are satisfied or neutral with the service they receive from the department (≥70%). |
Met—99% |
met—94% |
|
Achievement of customer satisfaction standards |
The percentage of customers who are satisfied overall with their most recent interaction (≥ 85%). |
Not met—77.6% |
not met—81.6% |
|
Departmental interactions completed via digital channelsa |
The increase in the total number of interactions completed by customers and third parties via digital channels compared to previous year (≥ 5%). |
Met—5.3% |
met—6.2% |
|
Availability of ICT systems that support 24/7 customer access |
The availability of 24/7 customer access channels including online services and mobile applications (≥ 98%). |
Met—99.4% |
met—99.4% |
|
Achievement of payment quality standards: Medicare: Delivery of accurate medical benefits and services |
The percentage of sampled payment transactions that have been processed accurately (≥ 98%). |
Met—98% |
met—99% |
|
Average wait time (face-to-face) |
The average length of time a customer waits to access face-to-face services in the department’s service centres (≤ 15 minutes). |
Met—8 minutes and 8 seconds |
met—10 minutes and 31 seconds |
|
Average speed of answer: Pharmaceutical Benefits Scheme Authorities and My Health Record Providers (telephony) |
The average length of time a health provider waits to have a call answered through the department’s telephony services (≤ 30 seconds). |
Not met—40 seconds |
not met—40 seconds |
|
Average speed of answer: Providers (telephony) |
The average length of time a health provider waits to have a call answered through the department’s telephony services (≤ 2 minutes). |
Met—1 minute 27 seconds |
met—1 minute 56 seconds |
|
Average speed of answer: Customers (telephony) |
The average length of time a customer waits to have a call answered through the department’s telephony services (≤ 7 minutes). |
Met—6 minutes and 51 seconds |
met—6 minutes and 34 seconds |
|
Achievement of processing service level standards |
The percentage of claims processed within standard (≥ 82%). |
Met—99.3% |
met—95.4% |
|
Achievement of payment integrity standards: Medicare: Completed interventions with customers for compliance purposes |
The number of Medicare customer compliance cases completed (≥ 300). |
Met—1557 cases |
met—499 cases |
Note a: Department of Human Services’ Corporate Plan 2016–17 and Annual Report 2015–16 indicate this performance measure is reaching maturity and is under review.
Source: Department of Human Services’ Corporate Plan 2016–17 and Annual Reports (2015–16 and 2016–17).
Human Services monitoring of channel benefits and achievements
4.8 The ANAO’s examination of departmental documentation found that information on the planning and development of electronic claiming channels was limited. In addition, under Human Services’ project management framework once channels are introduced the ongoing management is considered business as usual and the achievement of anticipated savings and benefits, other than usage of the channels, are no longer tracked. Although Human Services has adequate reporting to track claiming trends, reporting on other channel achievements and benefits beyond an increase in take-up rates is limited. As already noted (see from paragraph 3.25), expected take-up rates for individual channels during the planning and implementation stage have generally not been met contributing to the anticipated savings for those channels not being realised within expected timeframes. A lack of ongoing tracking of benefits and costs means that the department is unable to determine when or if individual channels begin to represent value against the initial and ongoing investment required (see Case Study 1).
|
Case study 1. Introduction of Easyclaim and take-up of Medicare Online |
|
In 2007, the department introduced Easyclaim anticipating that this channel would eventually replace Medicare Online. The department invested $12 million to implement the channel (including project initiation and infrastructure, design, building and testing) and anticipated that around 70 per cent of electronic claiming would be lodged from this channel. In the first two years, Easyclaim was used to lodge only two per cent of claims and take-up has plateaued at around eight per cent since 2011. While the forecasted uptake of the Easyclaim channel did not materialise as originally envisaged, the Medicare Online channel has increased substantially and now accounts for 83 per cent of all electronically claimed Medicare services. A 2009 departmental review of Medicare electronic claiming channels found that growth in the take-up rate for Easyclaim was the result of new electronic transactions (two-thirds) and ‘channel shift’ (one-third). To the extent that growth in a channel occurs as a result of transfer from another, rather than as a result of practices moving from manual to electronic claiming, any potential savings are reduced. |
4.9 While it can be assumed that savings have been generated from introducing electronic claiming; increases in the take-up of electronic claiming have not necessarily occurred where originally anticipated. As the department does not have current data on the impacts of shifts between channels it is not able to determine whether the introduction of each new channel has represented a good investment decision.
4.10 The department was unable to provide evidence that benchmarks to monitor channel delivery and benefits against, including from channel improvements, have been established, with the exception of increases in overall electronic claiming rates.23 This lack of benchmarking affects Human Services’ ability to comparatively assess the achievements of individual channels.
4.11 Business cases and project plans reviewed by the ANAO note some expected benefits from the introduction of electronic claiming aside from savings but these benefits are unquantified. Broadly these benefits can be characterised as increased flexibility for patients, reductions in administrative costs for providers and freeing up Human Services resources to prioritise complex claims/tasks. For those channels that have not achieved expected take-up rates (Easyclaim and CMBO) it is unlikely that these ‘intangible’ benefits would have been met, however given that electronic claiming is over 97 per cent it is expected that the benefits have been met to some degree in the overall channel take-up.
4.12 The ANAO’s examination of available documentation reveals that a significant amount of work was undertaken by departmental officers over several years to identify challenges impacting on electronic claiming and ways forward. Several of these documents identified that decision-making is hampered by a lack of current data on the cost of processing claims through the various channels. This lack of information has impacted on Human Services’ capacity to assess whether the cost associated with strategies to drive take-up and reduce manual claiming are warranted.
4.13 Performance monitoring of electronic claiming should capture:
- the key assumptions and objectives regarding the costs and benefits underpinning the business case for these investments in electronic claiming channels;
- whether these original performance parameters have been achieved; and
- whether the planned efficiencies and administrative savings have been realised.
4.14 The eClaiming and Payments strategy (referred to also at paragraph 3.53) was drafted around the end of 2014 and articulated the work necessary to achieve 100 per cent electronic claiming, including the possibility of mandating electronic claiming. Human Services advised that the strategy was not endorsed by the Executive who decided instead to progress a strategy of as close as possible to 100 per cent electronic claiming. The department was unable to provide evidence of this decision.
4.15 Human Services’ eClaiming and Payments strategy identified scope to consolidate and enhance claiming channels in particular:
Decommissioning some claiming channels would create efficiencies for the department and reduce the choices that health professionals are faced with when trying to take-up electronic patient claiming. Moving forward, conducting a detailed cost analysis of each system would no doubt reveal that less [sic] claiming channels would create efficiencies for the department in many ways.
4.16 The department has not conducted any reviews of electronic claiming as a whole since 2009, although previous reviews have been undertaken of ECLIPSE and the Easyclaim transaction fee. While the department does not have a current strategy to review and rationalise claiming channels they have advised that it is expected that work being undertaken to support the Modernising Health and Aged Care Payments Services Program will include a review and possible rationalisation. Since providers have multiple options for submitting claims at point of service the potential for ‘channel shift’ remains high; however the cost impact of any shift, either from manual to electronic or between electronic channels, cannot accurately be estimated as current costs are not tracked.
4.17 The department is currently unable to demonstrate that the introduction of individual electronic claiming channels has achieved the objectives of the business case, or whether they have realised anticipated administrative efficiencies. As such the department should undertake a review of the relative costs and impacts of individual electronic claiming channels to assess whether changes need to be made and ensure any changes made represent value for money.
4.18 Following on from this review into the relative costs and impacts of individual electronic claiming channels, and during the planning stage of the Modernising Health and Aged Care Payments Services Program, the department should consider whether efficiencies and savings would be best achieved by mandating electronic claiming at the point of service.
Recommendation no.1
4.19 To better inform its ongoing business decisions, the Department of Human Services should ensure its electronic claiming channel delivery strategy is supported by clear analysis of the costs and benefits of:
- establishing and maintaining electronic claiming channels; and
- maintaining manual Medicare claiming options.
Entity response: Agreed.
4.20 The department will ensure that future decisions on its electronic claiming channel delivery strategy are supported by clear analysis of the costs and benefits.
Have risks and issues been monitored and managed effectively?
Risks to the administration of Medicare electronic claiming channels have been managed effectively. The key risks to Medicare payment integrity and system functionality are addressed in a range of plans.
4.21 Responsibility for aspects of electronic claiming is shared across a number of areas within Human Services. Risk management plans24 identify existing controls (including an assessment of the effectiveness of these controls) as well as proposed treatments for risks to Medicare programs, including those risks related to the administration of electronic claiming.
4.22 In 2015–16 the branch with primary responsibility for the management of electronic claiming channels had a business plan and individual risk assessment plans for electronic claiming channels.25 While these plans have not been kept up-to-date, the key risks relevant to electronic claiming are addressed in other departmental plans as described later in this section. These risks are: payment integrity (the risk of patient and provider non-compliance with eligibility and other requirements), and system functionality (for example, ICT outages and data transfer).
4.23 In 2016, Human Services introduced the Health Services Design Authority, a forum for staff from the Health and Aged Care Group to consider proposals and process improvement initiatives for prioritisation according to costs, expected savings and ICT capability. The forum provides an opportunity for proposed channel enhancements to be considered alongside any other related initiatives that are being delivered.
Payment integrity
4.24 Human Services has established Payment Integrity Risk Management (PIRM) plans for the purpose of identifying the risks to payment integrity for a range of Human Services programs. The Medicare Benefits Schedule PIRM plan identifies 27 risks associated with the MBS across six categories: claim; Medicare card; customer record; staff; ICT/System; and provider.26 Of direct relevance to Human Services’ administration of electronic claiming channels are those risks that relate to the claim process itself (lodgement of false patient claims by individuals or syndicates through electronic claiming channels) and ICT/system issues (application of MBS rules and incorrect system calculation).
4.25 The PIRM plan identifies existing controls (including the effectiveness of these controls) as well as proposed treatments. Beyond this, the plan recommends departmental actions to effectively manage the potential risk to Medicare payment integrity. Individual risk owners were identified as required under the department’s Enterprise Risk Management policy.
4.26 Human Services conducts Payment Accuracy Reviews (PARs) through phone surveys with patients to provide some assurance that correct payments were made to individuals across both the Medicare and Pharmaceutical Benefits programs. In 2016–17, 1277 interviews were undertaken related to Medicare benefits payments showing 100 per cent accuracy. PAR results have not been publicly reported by Human Services, but previous annual reporting by Medicare Australia indicates that PAR results from 2007 through 2011 were consistently above 99 per cent. Since 2012, Human Services has had a KPI for their achievement of payment quality standards for the delivery of accurate medical benefits and services and has consistently met the target of 98 per cent.
4.27 A 2007–08 ANAO audit (Accuracy of Medicare Claims Processing) 27 found that the relevant system controls are generally adequate to support reliable processing of Medicare. Business rules have been developed to mitigate risks and these business rules supplement the payment integrity risk management controls included in the PIRM plans.
4.28 This audit did not examine compliance arrangements however, as noted in Chapter 3, following the implementation of Claiming Medicare Benefits Online (CMBO), compliance and fraud were identified as a risk for the channel due to the lack of controls required to make a claim. Throughout 2015, the department introduced a number of restrictions on claiming processes for CMBO in order to reduce the risk of fraud. On 30 January 2016, to further strengthen controls to prevent fraud, the automatic payment of claims made using CMBO ceased. Changes were implemented that require manual verification of receipts/invoices before payments are processed.
System functionality
4.29 Human Services’ current health, aged care and related veterans’ payments systems have evolved over more than 30 years and currently comprise more than 200 applications and 90 databases. These systems have some inefficiencies due to the age of the underlying technology, the complexity of the modern claiming and payment requirements, and the large transaction volumes, and are also at risk of systems failure. The 2014 Claiming and Payment Strategy for Health Programmes delivered by Human Services notes that ‘current system limitations and performance issues caused by operating on an old technology platform cannot be addressed without a move to a new technology solution’.
4.30 System incidents, including outages and technical problems that prevent providers from lodging claims, and potential security risks have increased over the past 12 months as a result of current systems degradation. These incidents highlight a number of system limitations from the old Mainframe technology that underpins the current Medicare payment system. Human Services are aware of the need for departmental claims and payments systems remediation, and are currently undertaking a range of activities to maintain minimum standards of compliance, operational stability, and system availability consistent with existing performance measures. Development and implementation associated with the Modernising Health and Aged Care Payments Services Program will reflect the current electronic service model—as compared to the in-person service model that the original payments system was designed to work with—and this is expected to lead to significant benefits for providers, the public and government, including improved system performance.
4.31 At an individual channel level, system disruptions are monitored regularly by Human Services. Monthly channel dashboards indicate when system degradations have affected Human Services’ ability to achieve service availability, service reliability, and response time targets. Channel dashboards (ECLIPSE and Medicare Easyclaim) from May 2017 record three outages with channels performing below expectations for the month. Channel dashboards (ECLIPSE, Easyclaim and Express Plus Medicare Mobile App) from June 2017 record no outages. Identified risks are being progressively addressed through an ICT Health Remediation program. Human Services has planned remediation actions to the end of the 2021 financial year.
4.32 Business Continuity Plans for Easyclaim, CMBO and Medicare Online detail the critical program ICT dependencies and incorporate Human Services’ actions required to recover and continue Medicare payment and claiming programs in the event of a significant disruption. Similarities between the three existent BCP plans indicate that these controls are relevant across all Medicare claiming channels.
Has the experience gained by Human Services through its delivery of electronic claiming informed the development of the Modernising Health and Aged Care Payments Services Program?
The Modernising Health and Aged Care Payments Services Program is in its early stages. Human Services is supporting the lead agency, the Department of Health, to understand the current state of service delivery and technology. Human Services’ principal role comprises remediation activities to allow existing systems to continue to operate reliably and effectively.
4.33 On 19 October 2016, the Government announced it will replace the current systems used by Human Services to deliver health, aged care and related veterans’ payments as they are ‘old, complex and at risk of failure’.28 These systems support more than 600 million payments to individuals and providers each year, worth around $50 billion.29 In March 2017, a Request for Information (RFI) was released to the market to obtain information on: how the new payment platform should be designed and delivered; the capabilities that exist within the market to deliver it; and potential procurement approaches. In July 2017, a market update was provided to keep interested parties informed about the program’s progress.
4.34 While the program of work is being led by the Department of Health and supported by the Departments of Human Services and Veterans’ Affairs, and the Digital Transformation Agency, the long-term governance and allocation of key responsibilities are unclear. Providing visibility and oversight of key responsibilities at an early stage is fundamental to good governance and accountability for and the delivery of effective and efficient programs and services.
4.35 The Government provided $31.5 million in 2016–17 to commence the RFI process. A further $67.3 million was allocated in 2017–18—$50.7 million for the Department of Health to progress market engagement, procurement and design and $16.6 million to Human Services for essential maintenance of current ICT systems. No further funding has been allocated in the forward estimates.
4.36 To support the program the Department of Health has established an Inter-departmental Committee to provide strategic advice and a Program Sponsoring Group to guide strategic direction and agree significant decisions. Human Services is a member of both of these Committees.30
4.37 Human Services subject-matter experts have been embedded in the program to develop a comprehensive view of current state service delivery and technology. Human Services has been involved in developing the understanding of:
- technical and data architecture;
- business processes and management; and
- system performance characteristics31.
4.38 In addition to continuing to provide advice and subject matter expertise to the Department of Health in relation to the current state and evaluation of RFI responses, Human Services’ main role will comprise remediation activities to allow existing systems to continue to operate reliably and effectively.
4.39 Over several years Human Services has managed risks of system failure through an ICT Health Remediation Strategy. The scope of remediation work comprises ICT operational improvements, upgrades to current software and database versions, decommissioning platforms, workforce capability and capital investments. Much of this work has been limited to basic maintenance and managing the risk of failure of critical systems.
4.40 With the $16.6 million allocated to Human Services in the 2017–18 Budget an enhanced program of remediation was developed. The Health and Aged Care Remediation Project is supported by the department’s Portfolio Project Office and will be subject to the project compliance and reporting requirements set out in the department’s project management framework.
Appendices
Appendix 1 Entity responses

Appendix 2 Medicare bulk bill and patient claim process

Appendix 3 Initiatives to support Medicare electronic claiming
|
Date |
Initiative |
|
May 1997 |
The Government committed $28.1 million over four years to introduce a new option to allow the electronic lodgement of Medicare claims directly from doctor’s surgeries. |
|
May 1999 |
Government commits $3.1 million in funding provided to encourage greater private health care usage by promoting simplified billing. |
|
May 2000 |
Government commits $16.4 million over four years to promote the widespread take-up of simplified billing throughout the private health industry. |
|
May 2001 |
Government provides funding of $4.7 million over four years provided to continue the development of systems to enable the electronic lodgement of Medicare claims directly from doctors’ surgeries. |
|
April 2003 |
Prime Minister announces continuation of a range of reforms designed to boost Australia’s medical workforce, and to provide bulk billing incentives for doctors. |
|
May 2003 |
Government commits to provided $9 million over five years to assist GPs to adopt Medicare Online and to provide $9.2 million over two years to assist GPs in areas of need to access broadband technology necessary for them to adopt Medicare Online. |
|
February 2004 |
The introduction of increased technology to lodge Medicare claims electronically at Point of Service. |
|
September 2007 |
The introduction of the Transitional Support Package, a financial assistance package providing $73.5 million over four years to encourage general practitioners and specialists to adopt Medicare electronic claiming. |
|
2007–2008 |
Medicare begins to collect bank account details from members of the public when they visit a Medicare office. |
|
May 2008 |
The Government committed to provide $8.6 million over four years to increase the take-up of electronic Medicare claiming. |
|
April 2009 |
Human Services Minister announces a $6 million Medicare Easyclaim Practice Management System Integration Solution Subsidy “for the development by software developers of solutions that support the integration of the Medicare Online and Medicare Easyclaim systems”. |
|
May 2009 |
Electronic patient claiming campaign (17 May – 30 June). |
|
July 2011 |
Medicare Australia, Centrelink, Child Support and CRS Australia integrated to form Human Services. |
Footnotes
1 These channels are used for bulk bill claiming by providers where the provider receives the benefit, patient claiming where the patient receives the benefit and simplified billing where Human Services pays the private health insurer or billing agent.
2 Prior to July 2011, Medicare payments were administered by Medicare Australia which, prior to October 2005, was known as the Health Insurance Commission.
3 Department of Health, Guaranteeing Medicare–modernising the health and aged care payments systems, Budget announcement, 2017.
4 The Medicare Safety Net provides benefits to eligible individuals, couples and families who have high out-of-hospital medical expenses.
5 Human Services is responsible for customer compliance only. The Administrative Arrangements Order made on 30 September 2015 transferred responsibility for Medicare Provider compliance to the Department of Health.
6 See ANAO Audit Report No.20 2007–08 Accuracy of Medicare Claims Processing; ANAO Audit Report No.26 2013–14 Medicare Compliance Audits; ANAO Audit Report No.27 2013–14 Integrity of Medicare Customer Data.
7 These commitments include a policy statement Investing for Growth (1997); Government Online-The Commonwealth Government’s Strategy (2000); Better Services, Better Government—The Federal Government’s E-government Strategy (2002); Australia’s Strategic Framework for the Information Economy (2004); the ICT Reform Program (2008); and The Coalition’s Policy for E-Government and the Digital Economy (2013).
8 Department of Human Services, Better Dealings with Government: Innovation in Payments and Information Services, Discussion Paper for Industry Consultation, September 2009.
9 The extent to which these objectives have been realised is discussed in Chapter 3.
10 Key features of this strategy are discussed further in Chapter 3.
11 A patient can also partially pay for a service and they will receive a cheque payable to the provider for the amount for the benefit. The patient is then required to pass this cheque on to the provider as payment along with any outstanding amount under the Pay Doctor Via Claimant scheme.
12 Authentication and security requirements include Public Key Infrastructure and Information Security Registered Assessors Program certification.
13 Human Services provides additional mechanisms to gather service user feedback including complaints, compliments and suggestions. The department also conducts two surveys: the Provider Satisfaction Survey which seeks input from practitioners, practice managers and pharmacists about their levels of satisfaction with Medicare services; and a customer-focussed survey which asks Medicare online account users to respond to questions about their experience with the site at the end of their session. The survey results are broadly used to measure departmental performance for the Medicare program as a whole and can make only a limited contribution to understanding the needs of electronic claiming users due to the response sample sizes and nature of the questions.
14 In 2017 the Stakeholder Consultative Group members represented Allied Health Professional Australia; Australian Association of Practice Managers; Australian Medical Association; Royal Australian College of General Practitioners; Rural Doctors Association of Australia; Australian Private Hospitals Association; Committee of Presidents of Medical Colleges; Medical Software Industry Association; Pharmaceutical Society of Australia; Pharmacy Guild of Australia; Society of Hospital Pharmacists of Australia; Consumers’ Health Forum; Private HealthCare Australia; and Services for Australian Rural and Remote Allied Health.
15 BDOs are employed at an APS5 level. As at April 2015, Human Services’ Outreach Service Section had 62 staff, including BDOs.
16 These enhancements include Client Adaptor Enhancements and software versions that apply changes to installation package software specifications and supporting material.
17 The Express Plus Medicare Mobile App has been excluded from this analysis as it is counted as ‘manual’ within Human Services’ administrative reporting because all claims lodged are manually entered by Human Services staff.
18 Although there are some regulations that limit the ability of pathologists to lodge claims at point of service. For example patient claims are not able to be itemised until all required blood work has been completed.
19 Australian Statistical Geography Standard Remoteness Structure classifications are ‘major cities, ‘inner regional’, ‘outer regional’, ‘remote’ and ‘very remote’. ANAO analysis was based on practice postcode. A total of 637 865 (0.16 per cent) of postcodes could not be matched.
20 The department’s decision to wait to understand the impact of pending budget measures, announced as part of the 2008–09 and 2014–15 Budgets (Medicare Easyclaim—increasing take-up and Market testing of the payment of health services by commercial payment service providers respectively) were contributing factors for maintaining the fee in both 2010 and 2015. The maintenance of this fee was determined on the basis of a range of factors, including the current status of Medicare Easyclaim (which Human Services had made the decision not to review). Since 2007–08 Human Services has paid financial institutions around $42.6 million in transaction fees.
21 Following the integration of Human Services and other agencies in 2011, existing unit prices no longer reflected efficiencies gained from customer service changes (including the increase in digital or online transactions when compared to telephonic or in-person transactions). Changes to the funding model were made to reflect updated measures and costs associated with Human Services’ workload.
22 Human Services advised that the 2010 Program and Channel Expenses Report was not cleared internally.
23 The expected take-up rates following Business Development Officer engagement with providers/practices targeted through point of service strategies are recorded in strategy plans and reported against (and, as noted from paragraph 3.17, the targets are generally achieved).
24 These are the Health and Information Group Risk Plan 2016-17, the Health Service Delivery Division Risk Management Plan 2016-17, and the Health Programmes Division Risk Management Plan 2016-17.
25 Under Human Services’ Enterprise Risk Management policy any group, program, division or branch with a business plan must also have a risk management plan.
26 Human Services is responsible for customer compliance only. The Administrative Arrangements Order made on 30 September 2015 transferred responsibility for Medicare Provider compliance to the Department of Health.
27 ANAO Audit Report No.20 2007–08 Accuracy of Medicare Claims Processing.
28 See footnote 3.
29 Ibid.
30 The other members of these Committees are representatives from the Digital Transformation Agency and the Department of Veterans’ Affairs (Program Sponsoring Group and Inter-departmental Committee) as well as the Department of the Prime Minister and Cabinet and the Departments of Finance and the Treasury (Inter-departmental Committee).
31 Human Services draws on internal expertise as well as two previous reviews of the operations of Medicare systems completed 2013 and 2014.