Browse our range of reports and publications including performance and financial statement audit reports, assurance review reports, information reports and annual reports.
Expansion of Telehealth Services

Please direct enquiries through our contact page.
Audit snapshot
Why did we do this audit?
- In 2020 medical services delivered by phone and video (telehealth) were significantly expanded as a response to the COVID-19 pandemic.
- The expansion was described as ’10 years of reform in only 10 days’ and the ‘most significant structural reform to Medicare since it began’.
- The audit provides assurance over the rapid implementation of policy changes and transition from emergency to permanent settings
Key facts
- Telehealth expansion involved amending items listed on the Medicare Benefits Schedule (MBS).
- In March–May 2020, 281 temporary telehealth MBS items were created. The items were extended as the pandemic continued.
- In January 2022, 211 telehealth items were retained permanently.
What did we find?
- The Department of Health and Aged Care (Health) expanded telehealth to meet objectives, however there were shortfalls in governance, risk management and evaluation.
- The expansion of telehealth was informed by largely robust policy advice and planning.
- The expansion was partly supported by sound implementation arrangements.
- Health did not adequately monitor or evaluate the expansion.
What did we recommend?
- There were four recommendations relating to the governance of MBS changes, risk management and evaluation of the temporary and permanent telehealth expansion.
- Health agreed to three recommendations and agreed in-principle to one recommendation.
28
Days between activation of COVID-19 emergency plans and a decision to extend telehealth to the entire population.
16.5%
Proportion of MBS services provided via telehealth April–June 2020 (vs. 0.06% in April–June 2019)
31.0%
Proportion of general practice MBS services provided via telehealth April–June 2020 (vs. 0.04% in April–June 2019)
Summary and recommendations
Background
1. Medicare is Australia’s national health insurance scheme. Medicare rebates are payable for health services that are specified as items on the Medicare Benefits Schedule (MBS). In response to the COVID-19 pandemic, between March 2020 and May 2020 the Australian Government introduced 281 new telehealth items on the MBS to enable the entire Medicare-eligible population to access a broad range of health services via videoconferencing and phone rather than face-to-face with a provider. Although the temporary telehealth items introduced in response to COVID-19 were initially scheduled to expire on 30 September 2020, the Australian Government postponed their expiry on three occasions in 2020 and 2021.
2. On 13 December 2021 the Minister for Health and Aged Care announced that telehealth would become a permanent feature of Medicare, noting that since March 2020 over 86.3 million telehealth items introduced in response to COVID-19 had been billed for services delivered to 16.1 million patients by over 89,000 providers, totalling $4.4 billion in Medicare benefits. The 2022–23 Budget described the introduction of permanent telehealth as the ‘most significant structural reform to Medicare since it began.’
Rationale for undertaking the audit
3. The COVID-19 pandemic and the pace and scale of the Australian Government’s response impacts on the risk environment faced by the Australian public sector. This performance audit was conducted under phase two of the ANAO’s multi-year strategy that focuses on the effective, efficient, economical and ethical delivery of the Australian Government’s response to the COVID-19 pandemic.
4. The expansion of telehealth services in 2020 to provide whole of population access to health services during the COVID-19 pandemic has been described by the Department of Health and Aged Care (Health) as ‘10 years of reform in only 10 days’. Rapid implementation of policy changes can increase risks to effective and efficient delivery of public services. The audit was conducted to provide assurance to Parliament over the rapid implementation of health policy changes during a pandemic and the transition from emergency to permanent arrangements.
Audit objective and criteria
5. The objective of the audit was to assess whether the Department of Health and Aged Care has effectively managed the expansion of telehealth services during and post the COVID-19 pandemic.
6. To form a conclusion against the objective, the ANAO adopted the following high-level criteria.
- Was the expansion informed by robust planning and policy advice?
- Was the expansion supported by sound implementation arrangements?
- Has monitoring and evaluation of the expansion led to improvements?
7. The audit scope did not include Services Australia’s administration of telehealth benefit payments, or telehealth services outside of those listed on the MBS (such as those managed by the Department of Veterans’ Affairs). The audit examined the incorporation of telehealth integrity risks into Health’s provider compliance arrangements but did not evaluate the effectiveness of compliance activities.
Conclusion
8. The Department of Health and Aged Care expanded telehealth services during and post the COVID-19 pandemic to meet the Australian Government’s objectives of continued access to essential health services and flexible health care, however there were shortfalls in the governance, risk management and evaluation of the expansion.
9. The temporary and permanent expansion of MBS telehealth items was informed by largely robust policy advice and planning. Policy advice to government on temporary telehealth services introduced in response to COVID-19 considered stakeholder views, although it did not present a structured assessment of risks or options for decision. Policy advice on permanent telehealth maintained focus on objectives, largely considered stakeholder opinions, and assessed the costs and benefits of different options. The implementation of temporary and permanent telehealth was based on business as usual processes for changes to MBS items, and there was no implementation plan for temporary telehealth. There was a high-level implementation plan for the permanent expansion of telehealth, although this did not adequately address evaluation.
10. Health implemented significant changes to the MBS and in doing so provided largely appropriate support to delivery partners. However, the telehealth expansion was only partly supported by sound implementation arrangements. Although Health conducted risk-based post-payment compliance activities, the governance arrangements for the implementation of temporary telehealth involved inadequate assessment of the implementation and integrity risks.
11. Health did not plan for performance monitoring or evaluation of temporary or permanent telehealth. Performance monitoring of the temporary telehealth expansion was limited and lacked measures and targets that could inform judgements about performance, and there was no evaluation that could assist with the design and implementation of potential expansions to telehealth during future emergency conditions. Evaluation of permanent telehealth is developing.
Supporting findings
Planning and policy advice
12. Health provided policy advice that was consistent with the Australian Government’s evolving policy objectives for temporary and permanent telehealth. (See paragraphs 2.3 to 2.7)
13. In the urgent timeframe of the initial pandemic response, Health advised the Minister for Health on the costs but only some of the benefits and risks of temporary telehealth policy settings. Health presented one option for decision by the Australian Government concurrently with proposals for several other pandemic response measures. The assessment of temporary COVID-19 telehealth policy option risks between March 2020 and May 2021 was partly compliant with Australian Government budget policy. Health presented five policy options for permanent telehealth that articulated risks, benefits and costs. Assessment of permanent telehealth policy option risks was compliant with budget policy. (See paragraphs 2.8 to 2.26)
14. Health consulted with and incorporated the opinions of peak bodies into policy advice for temporary and permanent telehealth. Consultation on temporary telehealth occurred within short timeframes. For general practice and allied health permanent telehealth, consultation practices were largely aligned with a stakeholder engagement plan. For specialist permanent telehealth, there was no finalised stakeholder engagement plan, however consultations occurred, and views were reflected in policy advice. State and territory governments were involved in high level discussions but were largely not consulted on the details of changes to MBS items. A key Indigenous peak body was not involved in stakeholder meetings where the specifics of telehealth policy settings were discussed. Health used pre-pandemic experience with telehealth, and experience arising from the pandemic, to inform policy proposals. (See paragraphs 2.27 to 2.45)
15. In introducing temporary telehealth in response to COVID-19, Health followed existing processes associated with section 3C determinations under the Health Insurance Act 1973 without a documented implementation plan. Implementation stages and milestones for both temporary and permanent telehealth were described at a high level in advice to government. The high-level advice to government did not set out how the changes would be evaluated. Health aligned planning for permanent telehealth with other plans for primary health care reform. The implementation plan for permanent telehealth has been subject to multiple changes, including in response to the ongoing pandemic. (See paragraphs 2.46 to 2.58)
Implementation arrangements
16. Standard procedures used by Health to implement telehealth changes to the MBS did not require key implementation decisions and plans to be documented, implementation and integrity risks to be managed, or performance monitoring and evaluation plans to be considered. As a result, Health’s governance arrangements for the expansion of telehealth were not fit-for-purpose. Health’s project management framework provides suitable governance arrangements, but it was not used. (See paragraphs 3.2 to 3.20)
17. Health did not manage implementation risks associated with temporary or permanent telehealth changes in accordance with its risk management policy. (See paragraphs 3.21 to 3.33)
18. Although Health did not consistently adhere to the agreed process to govern the implementation of changes to the MBS by Services Australia, Health supported Services Australia to make rapid changes to MBS telehealth items during the initial expansion of temporary telehealth. While there was no communications plan, Health published a substantial amount of guidance material for health providers and maintained a facility for provider enquiries. Between 30 March 2020 and 12 June 2022, service standards for responding to telehealth-related inquiries were not consistently met. (See paragraphs 3.34 to 3.48)
19. Health did not conduct a risk assessment of integrity risks, such as provider fraud and non-compliance, prior to implementing the temporary and permanent MBS telehealth items. Treatments to prevent provider non-compliance with telehealth items were limited. There is a risk-based model for detecting and treating provider fraud and non-compliance. Corrective non-compliance treatments were applied to a subset of non-compliant providers in accordance with this model and focused on the most egregious non-compliance behaviours. (See paragraphs 3.49 to 3.59)
Monitoring and review
20. Health did not establish performance measures for the telehealth expansion. Health used MBS billing data to monitor telehealth usage patterns, on the assumption that telehealth usage and billing behaviours were sufficient indicators of successful telehealth implementation. There were no performance targets. (See paragraphs 4.4 to 4.17)
21. Health did not develop an evaluation plan for temporary telehealth or for permanent telehealth. Telehealth policy proposals did not address evaluation in detail. Health has not coherently evaluated the effectiveness of telehealth as a pandemic response, although some analysis of billing data and independent research has been undertaken. Health used some reviews and data analysis to inform decision making on permanent telehealth. Health’s plans to evaluate permanent telehealth were not settled as at September 2022. (See paragraphs 4.18 to 4.32)
Recommendations
22. This report makes four recommendations to Health.
Recommendation no. 1
Paragraph 3.18
The Department of Health and Aged Care strengthen its systems of control for the implementation of material changes to the Medicare Benefits Schedule, to embed elements of governance that are currently unaddressed including documentation of key implementation issues and decisions, and planning for performance monitoring and evaluation.
Department of Health and Aged Care response: Agreed.
Recommendation no. 2
Paragraph 3.32
The Department of Health and Aged Care develop procedures that ensure proposed material changes to the Medicare Benefits Schedule are subject to a structured and documented risk assessment that covers implementation, integrity and other risks.
Department of Health and Aged Care response: Agreed.
Recommendation no. 3
Paragraph 4.20
As a component of a broader review into the COVID-19 pandemic response required under the Australian Health Sector Emergency Response Plan for Novel Coronavirus, the Department of Health and Aged Care considers the lessons learned for future pandemic preparedness from the inclusion of temporary telehealth items as one of several COVID-19 pandemic response measures.
Department of Health and Aged Care response: Agreed in-principle.
Recommendation no. 4
Paragraph 4.31
The Department of Health and Aged Care finalise its plans to evaluate permanent telehealth.
Department of Health and Aged Care response: Agreed.
Summary of entity response
The Department of Health and Aged Care acknowledges the ANAO findings while also recognising the unique scenario of the COVID19 emergency health response. The Department delivered on its objectives to maintain patients’ access to essential health services throughout lockdowns as well as reducing risk of transmission for patients and providers. To date, over 132 million services have been provided via telehealth, with the Medical Benefits Schedule (MBS) items replicating the requirements of face-to-face items for clinical appropriateness and integrity. This was informed by regular consultation with stakeholders, expert advice, and available research forming the basis of advice to Government as part of the initial health crisis and beyond.
The rapid deployment of MBS telehealth measures, ensuring access to essential health care services and protecting the capacity of the health system, was in alignment with the ‘Australian Health Sector Emergency Response Plan for Novel Coronavirus’. The key messages for all Australian Government entities are also noted, emphasising the requirements despite urgent implementation deadlines.
The MBS, and the telehealth services within it, are demand driven services that respond to patient need and any assertion in relation to targets would run counterproductive to this. The suitability of telehealth, noting it mirrors face to face items to provide access to care, at any given time for a patient consultation is a clinical judgement by a practitioner with respect to their patient’s care, and outside the remit of the Department.
The alignment of MBS telehealth items with contemporary clinical practice is subject to ongoing refinement and evaluation through a post-implementation review. The Minister for Health and Aged Care, the Hon Mark Butler MP, has formally requested the MBS Review Advisory Committee undertake this work, with a report back to Government in late 2023.
Below is a summary of key messages, including instances of good practice, which have been identified in this audit and may be relevant for the operations of other Australian Government entities.
Governance and risk management
Policy design
Performance and impact measurement
1. Background
Introduction
1.1 Medicare is Australia’s national health insurance scheme. Under the scheme, patients may claim a rebate (referred to as a benefit) for specified health or medical services. Services covered by Medicare benefits are detailed in legislation and are collectively known as the Medicare Benefits Schedule (MBS). Each service listed in the MBS has an item number, a descriptor which outlines the type and scope of the service, the Medicare schedule fee1 and the Medicare benefit (rebate).2
1.2 As the administering department for the Health Insurance Act 1973, the Australian Government Department of Health and Aged Care (Health) is responsible for advising the Australian Government on proposals to add, amend or remove health services listed on the MBS, implementing changes to the MBS as directed by the Australian Government, and ensuring that health providers3 are claiming rebates in accordance with the MBS. Medicare claims and payments are administered by Services Australia, which is directly accountable to the Australian Government for service delivery of programs such as Medicare. Health and Services Australia maintain a program agreement for administration of the Medicare program, which forms part of a joint Statement of Intent between the two entities.
1.3 The MBS has featured a limited range of telehealth service items since 2002. In this report ‘telehealth’ refers to real time clinical consultations conducted via videoconferencing or phone rather than face-to-face. The MBS defines a service via videoconference as ‘telehealth attendance’ and a service via telephone as ‘phone attendance’.
1.4 In late 2019 coronavirus disease 2019 (COVID-19) emerged as a global pandemic and was declared to be a ‘public health emergency of international concern’ by the World Health Organization on 30 January 2020. From January 2020 the Australian Government commenced the introduction of a range of policies and measures in response to the COVID-19 pandemic. The Australian Government’s health and economic response has included:
- travel restrictions, international border controls and quarantine arrangements;
- delivery of substantial economic stimulus, including financial support for affected individuals, businesses and communities; and
- support for essential services and procurement and deployment of critical medical supplies (including the national vaccine rollout).
1.5 In response to the COVID-19 pandemic, between March and May 2020 the Australian Government introduced 281 new telehealth items on the MBS to enable the entire Medicare-eligible population to access a broad range of health services via videoconferencing and phone. Although the temporary telehealth items introduced in response to COVID-19 were initially scheduled to expire on 30 September 2020, the Australian Government postponed their expiry on three occasions in 2020 and 2021.
1.6 On 13 December 2021 the Minister for Health and Aged Care4 (the Minister) announced that telehealth would become a permanent feature of Medicare, noting that since March 2020 over 86.3 million telehealth items introduced in response to COVID-19 had been billed for services delivered to 16.1 million patients by over 89,000 providers, totalling $4.4 billion in Medicare benefits. The 2022–23 Budget described the introduction of permanent telehealth as:
the most significant structural reform to Medicare since it began, and has revolutionised the patient-doctor relationship. It is one of the most significant, long term benefits of the Government’s response to the COVID-19 pandemic, providing all Australians with improved access to health services.
Telehealth prior to February 2020
1.7 In 2002 the Australian Government added telehealth psychiatry items to the MBS. In the 2011–12 Budget telehealth services were expanded to a broader range of specialists. The telehealth items were primarily directed at patients in remote and regional areas, residents of aged care facilities in remote and regional locations, and patients of Aboriginal medical services5 regardless of location. The telehealth items were provided over videoconference, including ‘patient-end’ support services provided in general practice.6 Some of the telehealth items required the provider to have an existing clinical relationship with the patient (defined as three face-to-face consultations with that provider in the preceding 12 months).
1.8 Between 1 November 2018 and 30 June 2020 the MBS contained mental health services provided to patients in drought affected areas7 by videoconference. In January 2020 the Australian Government expanded these MBS telehealth services to patients who experienced an adverse change in mental health as a result of bushfires occurring in 2019–20.
1.9 None of the telehealth services listed in paragraphs 1.7 to 1.8 could be provided by phone, or were subject to a requirement that the service be bulk billed.
Telehealth during the COVID-19 pandemic response
1.10 On 17 February 2020 the Australian Health Protection Principal Committee8 endorsed the Australian Health Sector Emergency Response Plan for Novel Coronavirus (COVID-19) (COVID-19 Plan). The COVID-19 Plan provided that the Australian Government and state and territory governments would work together to develop new models of care to manage patients during the COVID-19 pandemic and ensure that the provision of primary health care would be adapted to any changes in the needs of vulnerable groups during the outbreak. On 27 February 2020 the Prime Minister announced the activation of the ‘Targeted Action’ stage of the COVID-19 Plan. Health immediately commenced development of a National Primary Care Targeted Action Plan, which proposed six measures to be adopted as part of an overarching strategy for providing primary care during the pandemic. One of the six measures was the creation of temporary MBS items for medical, nursing and mental health attendances delivered via telehealth.
Telehealth for those vulnerable to COVID-19
1.11 On 11 March 2020 the Prime Minister announced that the Australian Government had allocated $100 million in funding for new Medicare telehealth services. The announcement noted that the new Medicare telehealth services would be available via phone or video; bulk billed; and available to people in home isolation or quarantine as a result of coronavirus, as well as specified vulnerable patient groups9 regardless of their home isolation or quarantine status.
1.12 Between 12 and 24 March 2020 the Minister and Health made nine determinations under section 3C of the Health Insurance Act 1973 (3C determinations) to implement this package.10 The 3C determinations specified that services should be provided by videoconference, or by phone where suitable videoconference capabilities were not available. The items could be claimed only if the service was bulk billed, the patient was not admitted to hospital; and there was an existing clinical relationship (defined as one face-to-face consultation in the preceding 12 months). Initially the telehealth items also could be used for any patient if the provider had been infected by COVID-19 or was required to self-isolate, to prevent the provider from transmitting COVID-19 to a patient. On 23 March 2020 Health expanded the eligibility for providers to align it with the definition for vulnerable patients.11
Whole of population telehealth in response to COVID-19
1.13 On 18 March 2020 the Governor-General of the Commonwealth of Australia declared that a human biosecurity emergency exists.12 Between 18 and 22 March 2020 the Australian Government announced restrictions on commercial and social gatherings, the closure of Australia’s international borders to non-residents and non-citizens, new measures aimed at preventing panic-buying of medicines, and economic stimulus and industry support packages.13
1.14 The Minister announced on 23 March 2020 that the Australian Government was examining the expansion of temporary telehealth to the whole population, and on 30 March 2020 that temporary telehealth services would be extended to all persons eligible for Medicare services. A new 3C determination expanded the range of medical services that could be provided by videoconference or phone; removed requirements for providers to have an existing clinical relationship with the patient; and inserted a restriction to prevent items being billed for services with multiple patients simultaneously.14
1.15 The requirement to bulk bill the new temporary telehealth services was retained for a further week before being limited to concessional and vulnerable patients from 6 April 2020 onwards. The bulk billing requirement was removed completely for specialists, allied health and other specified providers from 20 April 2020.
1.16 Between 3 April and 19 May 2020 the Minister and Health made seven further 3C determinations that expanded the range of services available and corrected errors with previous instruments. By 22 May 2020, 281 telehealth items had been created in response to COVID-19.
Maintenance of COVID-19 telehealth
1.17 As the new telehealth items were originally conceived as a six-month temporary measure, in May 2020 Health commenced planning for the expiry of these items by September 2020. However, due to the ongoing pandemic, the expiry date of the temporary telehealth items was extended in September 2020 (to 31 March 2021), March 2021 (to 30 June 2021) and June 2021 (to 31 December 2021).
1.18 During this period, Health made adjustments to temporary telehealth services, including:
- reintroduction of the requirement for providers of non-referred services to have a pre-existing clinical relationship with the patient15;
- removal of the requirement for providers in general practice to bulk bill telehealth services for concessional and vulnerable patients;
- curtailment of the range of services that could be delivered by phone (as opposed to videoconference);
- introduction of general practice phone items for patients located in a COVID-19 hotspot declared by the Australian Government Chief Medical Officer; and
- introduction of 40 new temporary MBS telehealth services for specialists providing services to private patients admitted to hospital, where the specialist was located in a COVID-19 hotspot or was in mandatory isolation due to COVID-19.
Permanent telehealth
1.19 In June 2020 the Prime Minister wrote to the Minister to advise:
Due to our success in suppressing the spread of the coronavirus and our commitment to transitioning to a COVID-safe economy and society…I consider there is a diminishing need for further [temporary COVID-19] telehealth items. I ask that you seek my agreement to any further changes ahead of a strategic discussion on the future of telehealth and post-COVID-19 primary health care reform…
1.20 Health planned for the incorporation of telehealth as a core initiative in the Australian Government’s primary health care reform package that had been announced in May 2019. The package included the finalisation of a Primary Health Care 10 Year Plan, which would provide a national roadmap for primary health care policy and planning.
1.21 In October 2021 Health released a consultation draft of the Primary Health Care 10 Year Plan, which proposed the continuation of whole of population telehealth on a permanent basis. The consultation draft expressed an intent to increase the uptake of video for telehealth service delivery, and proposed that the requirement for a general practice provider to have an existing clinical relationship with a telehealth patient would be replaced by voluntary patient registration.16
1.22 On 13 December 2021 the Minister announced that whole of population telehealth would become a permanent feature of Medicare. On 16 December 2021 Health made a 3C determination to permanently retain 211 telehealth items used during 2021.
1.23 Sixteen days after the permanent arrangements commenced, the Australian Government announced it would temporarily reinstate 75 temporary videoconference and phone services that had been permitted to expire on 31 December 2021, in response to a spike in Omicron-variant COVID-19 cases.
1.24 Figure 1.1 depicts the developments in telehealth between January 2020 and June 2022.
Figure 1.1: The expansion of telehealth, January 2020 to June 2022

Note: Stages refer to telehealth expansion implementation stages outlined in a Health fact sheet and other Health documentation (see paragraphs 2.50 to 2.51).
Source: ANAO analysis.
Usage of telehealth items
1.25 Figure 1.2 depicts the dollar value of benefits paid for telehealth services introduced in response to COVID-19.
Figure 1.2: Value of benefits paid for telehealth items introduced in response to COVID-19, January 2020 to June 2022
Source: ANAO analysis of Services Australia data.
1.26 Figure 1.3 depicts the billing of telehealth items introduced in response to COVID-19 by general practitioners, specialists, and allied health professionals between 1 March 2020 and 30 June 2022. The majority of GP and specialist telehealth services were delivered by phone during this period.
Figure 1.3: Medicare Benefits Schedule COVID-19 telehealth item billing, March 2020 to June 2022
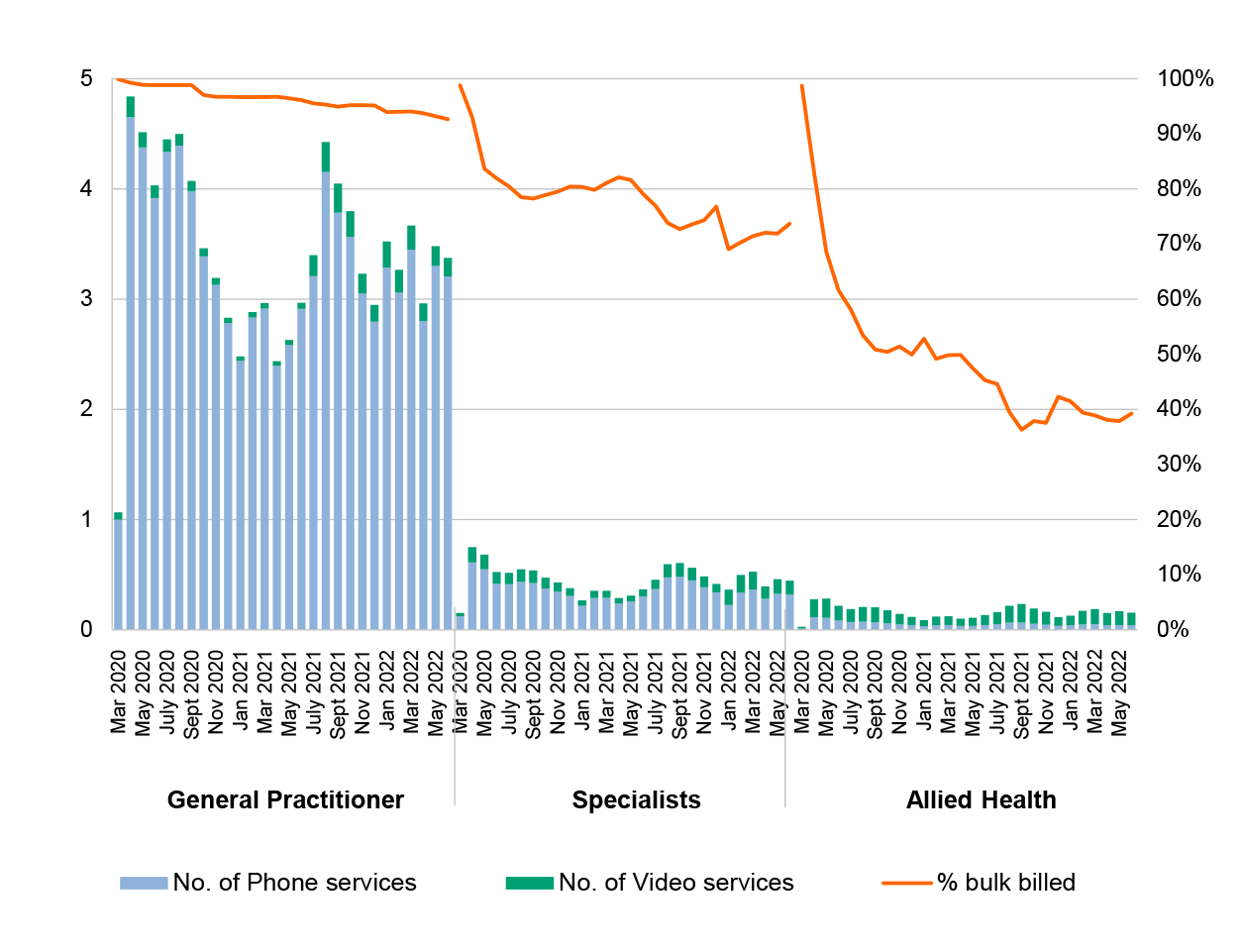
Source: ANAO analysis of Services Australia data.
1.27 As a proportion of all MBS services delivered by general practitioners between March 2020 and June 2022, telehealth represented approximately 20 to 30 per cent, depending on the quarter (Figure 1.4).
Figure 1.4: Mode of MBS service delivery, July 2019 to June 2022
Note: Telehealth services preceding 1 January 2020 are not visible in the chart as they comprised less than 0.1 per cent of total services for GPs and all practitioners.
Source: ANAO analysis of Services Australia data.
Rationale for undertaking the audit
1.28 The COVID-19 pandemic and the pace and scale of the Australian Government’s response impacts on the risk environment faced by the Australian public sector. This performance audit was conducted under phase two of the ANAO’s multi-year strategy that focuses on the effective, efficient, economical and ethical delivery of the Australian Government’s response to the COVID-19 pandemic.17
1.29 The expansion of telehealth services in 2020 to provide whole of population access to health services during the COVID-19 pandemic has been described by Health as ‘10 years of reform in only 10 days’. Rapid implementation of policy changes can increase risks to effective and efficient delivery of public services. The audit was conducted to provide assurance to Parliament over the rapid implementation of health policy changes during a pandemic and the transition from emergency to permanent arrangements.
Audit approach
Audit objective, criteria and scope
1.30 The audit objective was to assess whether the Department of Health and Aged Care has effectively managed the expansion of telehealth services during and post the COVID-19 pandemic.
1.31 To form a conclusion against the objective, the following high-level criteria were adopted.
- Was the expansion informed by robust planning and policy advice?
- Was the expansion supported by sound implementation arrangements?
- Has monitoring and evaluation of the expansion led to improvements?
1.32 The audit examined whether appropriate treatments were applied to telehealth-specific integrity risks, however did not examine the effectiveness of these treatments or the treatment of broader integrity risks that are generic to all MBS items. The audit did not examine Services Australia’s administration of benefit payments, or telehealth services or subsidies not listed on the MBS.
Audit methodology
1.33 The audit involved:
- reviewing submissions and briefings to government;
- reviewing other entity documentation, including meeting papers and minutes, policies and procedures, and correspondence;
- analysing administrative data held in entity systems, including Health’s case management system for provider integrity activities;
- meetings with officers from relevant business areas within Health and Services Australia;
- analysing de-identified MBS transactional data provided by Services Australia;
- meetings with representatives of state and territory health departments with responsibilities relating to telehealth; and
- reviewing 31 submissions received by the ANAO from organisations and individuals.
1.34 The audit was conducted in accordance with ANAO Auditing Standards at a cost to the ANAO of approximately $637,000.
1.35 The team members for this audit were Michael McGillion, Kai Swoboda, Sam Jones, Dr Jennifer Canfield, Bezza Wolba, Alicia Vaughan, Daniel Whyte and Christine Chalmers.
2. Policy advice and planning
Areas examined
This chapter examines whether the temporary and permanent expansion of Medicare Benefits Schedule telehealth services was informed by robust policy advice and planning.
Conclusion
The temporary and permanent expansion of Medicare Benefits Schedule telehealth items was informed by largely robust policy advice and planning. Policy advice to government on temporary telehealth services introduced in response to COVID-19 considered stakeholder views, although it did not present a structured assessment of risks or options for decision. Policy advice on permanent telehealth maintained focus on objectives, largely considered stakeholder opinions, and assessed the costs and benefits of different options. The implementation of temporary and permanent telehealth was based on business as usual processes for changes to Medicare Benefits Schedule items, and there was no implementation plan for temporary telehealth. There was a high-level implementation plan for the permanent expansion of telehealth, although this did not adequately address evaluation.
Areas for improvement
The ANAO made two suggestions to the Department of Health and Aged Care regarding compliance with Australian Government budget policy requirements to assess the risk of new policy proposals, and stakeholder consultation for co-designed initiatives.
2.1 The Australian Government’s Delivering Great Policy model18 specifies that when providing policy advice, agencies should clearly define the objectives of a proposed policy; provide options that identify the key risks and benefits; collaborate with people affected by the policy; incorporate lessons from past experience; and provide a practical plan for implementation. Implementation plans should identify deliverables and milestones and embed evaluation at the outset.
2.2 A 2015 independent review of Australian Government processes for the development and implementation of large public programmes and projects noted that ‘informed decision making requires assessment of the specific risks being accepted and the broader context’.19
Was policy advice consistent with the Australian Government’s objectives?
The Department of Health and Aged Care provided policy advice that was consistent with the Australian Government’s evolving policy objectives for temporary and permanent telehealth.
2.3 To assess whether the Department of Health and Aged Care’s (Health’s) policy advice was consistent with policy objectives, the ANAO reviewed how Health described the purpose of proposed changes to telehealth in advice given to the Australian Government in policy briefings and ministerial submissions, as well as in government announcements, approval minutes, portfolio budget statements and explanatory statements for determinations made under section 3C of the Health Insurance Act 1973 (3C determinations).20
Temporary telehealth
2.4 Between March 2020 and February 2022 the government had several policy objectives for temporary telehealth.
- Late February to early March 2020 — the objective was to enable continued access to essential health services for vulnerable populations, while mitigating the risks of vulnerable patients being exposed to COVID-19 and patients who are required to self-isolate or quarantine exposing others to COVID-19.
- Late March to May 2020 — the objective was to enable continued access to essential health services for the whole population, while controlling the spread of COVID-19.
- June 2020 to December 2021 — the objective was to continue to control the spread of COVID-19. This would involve making limited changes to temporary telehealth settings including extensions to temporary telehealth, as informed by advice from the Australian Health Protection Principal Committee. Any telehealth proposals that were not necessary to suppress COVID-19 were to be incorporated into future policy advice on permanent telehealth as part of long-term health reform plans.
2.5 Health’s policy advice and communications between 9 March 2020 and 14 September 2021 contained statements of purpose that aligned with these objectives and followed the Australian Government’s evolving priorities for temporary telehealth.
Permanent telehealth
2.6 Between late 2021 and February 2022 the Australian Government’s policy objective for permanent telehealth was to improve flexible access to health services for all Australians.
2.7 Health’s policy advice and communications between November 2021 and February 2022 contained statements of purpose that aligned with this objective. Advice and communications after 18 December 2021 noted that this objective remained in place despite the Australian Government’s decision to reinstitute certain temporary telehealth items in response to the Omicron outbreak and delay the introduction of some permanent telehealth measures (such as the introduction of new compliance measures).
Were the costs, benefits and risks of different policy options considered?
In the urgent timeframe of the initial pandemic response, the Department of Health and Aged Care advised the Minister for Health on the costs but only some of the benefits and risks of temporary telehealth policy settings. Health presented one option for decision by the Australian Government concurrently with proposals for several other pandemic response measures. The assessment of temporary COVID-19 telehealth policy option risks between March 2020 and May 2021 was partly compliant with Australian Government budget policy. Health presented five policy options for permanent telehealth that articulated risks, benefits and costs. Assessment of permanent telehealth policy option risks was compliant with budget policy.
Telehealth as part of the COVID-19 pandemic response
2.8 Health considered several options before developing a proposal to expand telehealth services as a pandemic response measure. On 28 February 2020 the Chief Medical Officer for the Australian Government asked Health officials to consider how telehealth services could be used as a response for the pandemic. Health identified an initial four options involving the Medicare Benefits Schedule (MBS) (two introducing new telehealth MBS items to substitute for face-to-face services and two introducing new items for home visits for isolating patients), and two options that did not involve the MBS. Initial briefs to Health senior executives contained a short, high-level analysis of issues associated with these options, covering eligible populations, compliance risks, implementation considerations and cost impacts.
2.9 On 3 March 2020 the Minister through his office instructed Health to include ‘time-limited MBS items for telehealth in pandemic response planning’. Within seven days Health developed a policy proposal for expanded telehealth services alongside 17 other response measures. Advice on the proposed policy was presented to the Australian Government on 9–10 March 2020.
- Issues discussed included the requirement for patients to have a pre-existing face-to-face relationship with the provider and mandatory bulk billing.
- The advice covered the one option of telehealth delivered via videoconferencing. Health expressed a preference for videoconferencing over phone telehealth due to clinical risks associated with the latter.
- The advice did not explain the benefits of the proposed policy settings.
- The advice highlighted one risk specific to telehealth (that providers and patients may lack experience with videoconferencing) and noted that services could be delivered through widely-available video calling applications.
- The advice made a generic statement that compliance risks of the proposal would be adequately addressed by existing Medicare compliance procedures and audit protocols.
2.10 The Department of Finance agreed with Health’s view that the proposed policy would be cost-neutral on the basis that telehealth services would substitute for existing face-to-face services. Health advised the Australian Government that, as there was an element of uncertainty about how telehealth services would be taken up, a provision of $100 million should be set aside for a potential increase in MBS costs.
2.11 Health received approval to implement telehealth services in line with its policy advice on 10 March 2020.
2.12 On 11 March 2020 the Prime Minister announced that telehealth services would include both videoconferencing and phone services. The requirement to include phone services was unanticipated by Health. In response to the Prime Minister’s announcement, Health rapidly introduced phone telehealth items to the MBS with a requirement that these services could only be billed where providers and patients did not have the capability to undertake the service via videoconference. Health officials advised the ANAO that this requirement was largely unenforceable.
2.13 Following discussions with the Australian Medical Association and the Royal Australian College of General Practitioners, on 23 March 2020 the Minister announced that eligibility for telehealth was expected to be expanded to the whole Medicare-eligible population. Working with the Minister’s office, Health prepared formal advice for the Australian Government in line with the Minister’s announced approach.
- Similar to the previous advice, the advice examined one policy option and stated that integrity risks would be adequately addressed through existing compliance arrangements.
- Compared to previous advice, the advice contained greater detail on the benefits and risks of certain proposed policy settings such as removing the requirement for the provider and patient to have an existing clinical relationship.
- The advice identified as a risk that progressive implementation of telehealth MBS items might be required due to capacity constraints within Services Australia.
- The advice indicated that whole of population telehealth would be cost-neutral.
- The advice noted that further policy advice regarding additional specialist items would be provided at a later date.
2.14 Health provided advice to the Minister regarding additional specialist items in April and May 2020, in three tranches. The Minister approved the addition of specialist items as advised.
- The first tranche identified 11 priority face-to-face specialist services that would be offered also as telehealth services. It contained little discussion of the risks and benefits of the dual offering of the services via face-to-face and telehealth methods.
- The second tranche advised that an internal triaging process including clinical advice had been followed to evaluate all suggestions obtained through stakeholder consultation for mirroring existing face-to-face services as telehealth services. The advice proposed 28 face-to-face specialist services to be offered also as telehealth services. Again, it did not discuss risks or benefits of offering these dual services.
- The third tranche provided advice on the benefits and drawbacks of each of the remaining suggestions from stakeholders, including those not supported by Health, and from these suggestions proposed five additional face-to-face services that could be offered also via telehealth.
Maintenance of temporary telehealth
2.15 In July 2020 Health adopted an approach to modelling telehealth costs that did not assume cost-neutrality and was based on observed trends during the early pandemic. The costs of subsequent material changes to telehealth policy were advised to government based on Health modelling.
2.16 Australian Government budget policy requires entities to complete a Risk Potential Assessment Tool for new policy proposals with an estimated financial implication of $30 million or more.21 Between September 2020 and April 2021 Health presented three new policy proposals to extend temporary telehealth settings. Each proposal had an estimated financial implication exceeding $30 million. Health did not prepare Risk Potential Assessment Tools for these three proposals.
|
Opportunity for improvement |
|
2.17 Health should ensure that a Risk Potential Assessment Tool is completed for all new policy proposals with a financial impact of $30 million, in accordance with Australian Government budget policy, and could promote the use of the Risk Potential Assessment Tool as a better practice for new policy proposals of less than $30 million. |
2.18 New policy proposals to change the MBS may require the completion of a Regulation Impact Statement (RIS) in accordance with the Australian Government Regulatory Impact Analysis Framework.22 RISs must include the policy options being considered, the likely net benefit of each option, an implementation plan for the recommended option and an evaluation plan. The Office of Best Practice Regulation, which administers the framework, describes regulatory impact analysis as helping policymakers develop the evidence base for well-informed decision-making.23
2.19 Health was not required to prepare a RIS for the introduction of temporary telehealth services and extensions of these services in September 2020 and February 2021 due to an exemption granted by the Prime Minister on 31 March 2020 for urgent and unforeseen Australian Government measures made in response to COVID-19.24
2.20 For the third extension of temporary telehealth in May 2021, Health prepared a draft RIS that also included analysis of voluntary patient registration proposals.25 The RIS proposed two policy options. The first option considered a reversion to pre-COVID-19 MBS settings by permitting the temporary telehealth items to lapse and abandoning work on voluntary patient registration. The second option, nominated as the preferred option, proposed a further extension to temporary telehealth, the introduction of new temporary telehealth services, a redesign of telephone telehealth services for general practitioners (GPs), the introduction of new compliance arrangements, and continued development of voluntary patient registration. Under the heading of a third option, Health advised ‘at this stage, there is no other viable option’.
2.21 The draft RIS was informally reviewed by the Office of Best Practice Regulation, which provided feedback that the analysis of policy options ‘pre-empted’ the preferred solution because the definition of the problem and the description of the options alerted the reader to which of the options was preferred before the analysis of the impacts was stated. The Office of Best Practice Regulation review indicated that the draft RIS ‘would need significant further development’ to be able to support a final decision by the Australian Government regarding permanent telehealth and voluntary patient registration (see paragraph 2.24). The draft RIS was the form of regulatory impact analysis that supported a final decision on the third extension of temporary telehealth in May 2021.
Permanent telehealth
2.22 Between 2 June 2020 and 6 August 2021 Health officials provided seven ‘deep dive’ briefs to the Minister to discuss the benefits, risks and costs of permanent telehealth policy options. The briefs covered pre-pandemic utilisation of telehealth; lessons from temporary telehealth; potential policy options for GP and specialist post-pandemic telehealth including compliance arrangements; extensions of temporary telehealth arrangements; and the potential timing of new measures.
2.23 Advice on permanent telehealth was provided to the Australian Government in December 2021. The advice identified that permanent telehealth offered economic and productivity benefits, improved patient access, and was able to provide sufficient quality of care when offered in conjunction with face-to-face services. The advice discussed the evidence base that supported Health’s preference for videoconferencing rather than phone telehealth and noted that some stakeholders had raised concerns that this preference could affect equality of access for patients.
2.24 The advice included a RIS which evaluated five policy options (Table 2.1). The RIS recommended option five.
Table 2.1: Policy options for permanent telehealth presented in a December 2021 Regulation Impact Statement
|
Options |
Summary of the proposed policy |
|
|
1 |
Status quo — do nothing |
Reversion to pre-pandemic settings after temporary telehealth items lapse on 31 December 2021 |
|
2 |
Extend current COVID telehealth items to allow for a transition to living with COVID, without MyGPa |
Extend temporary settings to a nominated date in the future |
|
3 |
Retain telehealth services, without MyGP |
Telehealth items would be placed on the MBS in the same manner as other ongoing items |
|
4 |
MyGP, no telehealth |
Implement MyGP separately to telehealth — telehealth items would revert to pre-COVID-19 settings after temporary items lapse on 31 December 2021 |
|
5 |
MyGP and telehealth |
Telehealth items would be placed on the MBS in the same manner as other ongoing items, and subsequently restricted to patients registered under MyGP |
Note a: MyGP is the brand name for voluntary patient registration. Voluntary patient registration is a system whereby patients register with their usual general practice and nominate their usual doctor.
Source: Health records.
2.25 The recommended option was costed using a detailed methodology that compared a hypothetical scenario in which COVID-19 had not happened with actual telehealth data for the same period, to estimate the extent to which telehealth services substituted for face-to-face services during the pandemic. This approach aimed to control for other factors potentially influencing MBS costs. The analysis supporting the RIS was assessed as ‘adequate’ by the Office of Best Practice Regulation, the second lowest rating on a four-tier rating scale.26
2.26 Although the RIS examined the proposal for MyGP and permanent telehealth collectively, two separate Risk Potential Assessment Tools (RPATs) were prepared. The first RPAT examined the risks associated with MyGP, which included consideration of the impact of restricting GP telehealth to patients registered under MyGP. A second RPAT examined the risks of permanent telehealth for GPs, specialists, nursing, midwifery and allied health providers. The RPATs assigned a low risk rating to both MyGP and permanent telehealth.
Did policy advice consider stakeholder opinion and previous experience?
Health consulted with and incorporated the opinions of peak bodies into policy advice for temporary and permanent telehealth. Consultation on temporary telehealth occurred within short timeframes. For general practice and allied health permanent telehealth, consultation practices were largely aligned with a stakeholder engagement plan. For specialist permanent telehealth, there was no finalised stakeholder engagement plan, however consultations occurred, and views were reflected in policy advice. State and territory governments were involved in high level discussions but were largely not consulted on the details of changes to MBS items. A key Indigenous peak body was not involved in stakeholder meetings where the specifics of telehealth policy settings were discussed. Health used pre-pandemic experience with telehealth, and experience arising from the pandemic, to inform policy proposals.
Consultation on temporary telehealth
2.27 The introduction of temporary telehealth services in response to COVID-19 during March 2020 was not subject to a formal or structured consultation process, reflecting the short period in which rapid changes were required. However, during the 28-day period in which the fundamental policy options for temporary telehealth were developed and implemented, Health discussed telehealth proposals with primary health care stakeholders at ad hoc and standing meetings used to share broader information on the COVID-19 pandemic response.
- On 6 March 2020 Health hosted a pandemic preparedness forum (at which it discussed telehealth as a possible response measure) with representatives from peak bodies in general practice, allied health, practice management, nursing, rural and Indigenous health, pharmacy and pathology; primary health networks; state and territory governments; and National Disability Insurance Scheme representatives.
- Between 18 March and 16 December 2020 Health hosted 44 meetings of the GP Peak Body COVID-19 Response Teleconference. Participants included the Australian College of Rural and Remote Medicine (ACRRM), Royal Australian College of General Practitioners (RACGP), Royal Australasian College of Physicians (RACP), Rural Doctors Association of Australia (RDAA), Australian Medical Association (AMA), National Aboriginal Community Controlled Health Organisation (NACCHO), Council of Presidents of Medical Colleges, and Medical Indemnity Industry Association of Australia. Telehealth was discussed at 24 of these meetings.
- Between 25 March and 16 December 2020 Health hosted 35 meetings of a broader ‘Primary Health Care COVID-19 Response Teleconference’. Participants included organisations representing allied health and specialist professions, nursing, practice managers, universities, and rural and regional health services. Telehealth was discussed at 21 of these meetings.
- Between 31 March and 9 April 2020 Health approached 148 specialist and allied health peak bodies and interest groups, requesting that respondents complete a feedback form to suggest existing face-to-face specialist services that would be suitable to also be offered as telehealth services. The ANAO observed that Health provided tailored feedback to at least six respondents on whether their suggestions were progressed or not supported.27
2.28 Between 2020 and 2022 Health provided policy advice regarding further adjustments to temporary settings that originated from peak body feedback and opinion received by the department or Minister.
2.29 In accordance with a direction from the Australian Government, Health sought advice from the Australian Health Protection Principal Committee (AHPPC) on 10 August 2020 about extending temporary telehealth past September 2020 and briefed the Australian Government on this advice. The Australian Government directed that consideration of further extensions of telehealth and other pandemic response measures should also be informed by AHPPC advice. In December 2020 Health asked AHPPC to endorse advice that, while not specifically referencing telehealth, indicated that emergency response measures would be required until 31 December 2021. The AHPPC endorsed the advice on 23 December 2020. Advice on subsequent extensions of temporary telehealth settings in 2021 noted that the extensions were in accordance with AHPPC advice.
Consultation on permanent telehealth
2.30 From June 2020 onwards, responsibility for stakeholder consultation in relation to telehealth was divided between two divisions within Health. One division examined GP and allied health provider telehealth, and the second division examined telehealth for specialists.
Consultation on GP and allied health provider telehealth
2.31 Health consulted on GP and allied health provider telehealth under a stakeholder engagement strategy developed for the Primary Health Care 10 Year Plan (the 10 Year Plan).28 The strategy listed six mechanisms for consultation, of which four materially contributed to the formulation of policy for permanent telehealth: the Primary Health Reform Steering Group29, a series of roundtable discussions on specific issues in the primary health care system, and two rounds of formal public consultation on the draft 10 Year Plan.
- Primary Health Reform Steering Group — Meeting records show that telehealth was discussed substantively at six out of 20 meetings between 20 March and 11 December 2020.
- Roundtable discussions — Between 16 July and 11 December 2020 Health convened 12 roundtable discussions that included discussion on telehealth.
- Public consultation — Health published a Primary Health Reform Steering Group discussion paper and draft recommendations for the 10 Year Plan on its Consultation Hub30 between 15 June and 27 July 2021. A report that summarised the 201 submissions (including six relating to telehealth) was considered by the Steering Group on 13 August 2021. Health published the draft 10 Year Plan on its Consultation Hub between 13 October to 9 November 2021. Health received 185 submissions (including 142 referring to telehealth) from peak bodies, health service delivery organisations, businesses, not-for-profit organisations, primary health networks, individuals, state and territory governments, universities and research institutes and other respondents.
2.32 The remaining two mechanisms listed in the stakeholder engagement strategy were: convening meetings of a Primary Health Reform Consultation Group (which had a broader membership than the Steering Group), and targeted consultation meetings with states and territories. Neither of these mechanisms was used after June 2020 and they did not inform permanent telehealth policy.
2.33 In July 2020 Health commenced negotiations with four peak bodies (RACGP, AMA, ACRRM and RDAA) to request suggestions for policy settings and seek the support of these bodies for the Australian Government’s primary health care reform package. Between November 2020 and March 2021 Health and the four peak bodies met six times to discuss GP telehealth. At a meeting on 3 March 2021, Health presented a brief that summarised a proposal for permanent GP telehealth based on input from the peak bodies and the Primary Health Reform Steering Group Co-Chairs. Health shared preliminary costings of the proposed option with the four peak bodies. Policy advice to the Australian Government for the 2021–22 Budget noted the policy parameters were subject to ongoing discussion with RACGP, ACRRM, RDAA and AMA.
Consultation on specialist telehealth
2.34 In July 2020 Health prepared a brief for the Minister summarising unsolicited feedback from Australian Association of Consultant Physicians (AACP), Royal Australian and New Zealand College of Psychiatrists (RANZCP), and RACP on extending specialist telehealth.
2.35 In anticipation that temporary specialist telehealth would continue past 30 September 2020, Health commenced drafting a stakeholder engagement and communication strategy to inform the development of policy options for permanent specialist telehealth before the 2021–22 Budget. The draft strategy was not finalised.
2.36 The draft strategy identified four peak bodies (AMA, RACP, RANZCP and the Royal Australasian College of Surgeons (RACS)) as priority stakeholders. Between October 2020 and September 2021 Health held meetings with and sought feedback from the four peak bodies identified in the strategy and three other peak bodies, including the AACP (which had requested to be involved). Policy advice provided to the Australian Government for the 2021–22 Budget and in November 2021 conveyed the views of the AMA, RACP, RANZCP and RACS on the proposed policy options.
Reported difficulties with consultation
2.37 The ANAO received 31 submissions to the audit. Eight submissions from peak bodies representing providers and one state government provided positive feedback on the ability to discuss telehealth policy matters with Health between 2020 and 2022. Three submissions from organisations other than peak bodies (a state government, a patient advocacy group, and a private company) stated that it was difficult to contribute to the formulation of telehealth policy.
2.38 In a meeting with the ANAO, representatives from three states and territories advised that in their view, while the Australian Government consults with providers on changes to the MBS it largely does not consult with states and territories. The representatives noted the following.
- While state and territory health departments are represented at a high level in fora such as AHPPC and its sub-committees, these committees do not generally discuss the details of proposed changes to the MBS.
- The details of MBS telehealth items affect state and territory health departments. Where state and territory health providers offer virtual care services (health services that are equivalent or analogous to MBS telehealth) to a hospital outpatient, the practicalities of dealing with or choosing between two differently designed systems may impact on overall patient experience and the course of clinical treatment chosen.
- Some state and territory health departments are progressing virtual care strategies that are trying to promote cultural change in Medicare-eligible populations regarding how health services are accessed. States and territories have relevant experience to share with the Australian Government including the evaluation of virtual care initiatives.
2.39 The ANAO asked senior Health officials whether state and territories are a stakeholder for changes to the MBS. Health officials advised the following.
- Consultation and coordination via AHPPC and National Cabinet was substantial throughout the pandemic and involved senior decision-makers from each jurisdiction.
- State and territory authorities were not worried about the Australian Government’s regulatory approach to telehealth during the pandemic, other than requiring assurance that continuity of service would be maintained.
- Health would not normally consult with states and territories on the detail of MBS changes as the bulk of MBS funding is directed towards private providers and the amount of MBS funding provided under an intergovernmental agreement that permits state and territory health workers in remote locations to submit MBS claims is considered negligible. Peak bodies are the experts on the detail of MBS changes.
- Two states (New South Wales and Tasmania) were represented on the Primary Health Reform Steering Group (discussed in paragraph 2.31).
- The nature of consultation with state and territory health departments regarding changes to the MBS should be considered in the context of the consultation that is meant to occur under the National Health Reform Agreement.31
2.40 A submission to the audit from the National Aboriginal Community Controlled Health Organisation (NACCHO)32 stated that the 1 July 2021 removal of telephone MBS items was made without consultation with the Aboriginal Community Controlled Health Sector. As noted in paragraph 2.27, NACCHO met regularly with Health in the GP Peak Body COVID-19 Response Teleconference meetings and had representation on the Primary Health Reform Steering Group, however it was not represented in the meetings described in paragraph 2.33, where the specifics of telehealth policy settings were negotiated. The Minister received correspondence from NACCHO that noted the Australian Government’s commitment under the National Agreement on Closing the Gap to provide Aboriginal and Torres Strait Islander people with a greater say in policy making that affects them. Internal Health correspondence also noted that the interests of NACCHO were significant and different to those of other peak bodies.
|
Opportunity for improvement |
|
2.41 When co-designing policy settings, Health could assess whether the parties invited to co-design collectively represent all relevant interests, and if not consider whether additional targeted consultation is required to complement the co-design process. |
Incorporation of lessons from past experience
2.42 In December 2019 the MBS Review Taskforce33 convened a working group to examine telehealth as a concept, develop a set of MBS ‘Telehealth Principles’ to guide future telehealth policy, and provide recommendations to the Australian Government through the MBS Review Taskforce regarding telehealth. The MBS Review Taskforce endorsed the final report of the working group on 30 June 2020.34 The findings of the MBS Review Taskforce relating to telehealth, which included an emphasis on video rather than telephone as a telehealth medium, were referenced by Health in advice to the Australian Government in April 2021 and November 2021.
2.43 In June 2020 the Australian Government directed that proposals for permanent telehealth items should be assessed by and receive a recommendation from either the Medical Services Advisory Committee (MSAC)35 or the MBS Review Taskforce. Health did not implement this direction.
- Health determined that MSAC would be unlikely to be able to provide advice of the nature requested before August 2021, which did not meet Health’s intended timeframe to provide advice in April 2021 to the Australian Government for the 2021–22 Budget.
- The MBS Review Taskforce held its final meeting to complete its review of existing MBS items on 30 June 2020, and in May 2020 had already commenced drafting its final report, which was submitted to the Australian Government on 14 December 2020.
2.44 In November 2020 Health commissioned a Bond University research institute36 to provide a systematic literature review of the efficacy and value of telehealth services within primary care. The final report of the literature review was presented to the Australian Government and considered at a meeting of the Primary Health Reform Steering Group in April 2021.
2.45 Policy advice presented to the Australian Government in support of extensions of telehealth or proposals for permanent telehealth progressively contained greater analysis of telehealth billing trends during the pandemic.
Was an appropriate implementation plan developed?
In introducing temporary telehealth in response to COVID-19, Health followed existing processes associated with section 3C determinations under the Health Insurance Act 1973 without a documented implementation plan. Implementation stages and milestones for both temporary and permanent telehealth were described at a high level in advice to government. The high-level advice to government did not set out how the changes would be evaluated. Health aligned planning for permanent telehealth with other plans for primary health care reform. The implementation plan for permanent telehealth has been subject to multiple changes, including in response to the ongoing pandemic.
Implementation plan for temporary telehealth
2.46 In the period of rapid implementation of the initial temporary telehealth expansion, there was no documented implementation strategy or plan that outlined in advance deliverables and milestones. Consistent with the Australian Health Sector Emergency Response Plan for Novel Coronavirus, which states that ‘it will be important to commence measures as quickly as possible’ and before there is likely to be a good understanding of the disease, Health prioritised rapid implementation of telehealth changes over documented planning in March 2020.
2.47 Initial policy advice to government on 10 March 2020 sought only high-level approval to implement changes to the MBS to enable telehealth to be accessible for nominated classes of patients, with further details to be worked out with the Department of Finance. The advice did not identify specific health services as deliverables or nominate milestones for implementing these as MBS items. The advice did not specify the mechanism by which the changes would be made. The advice nominated an expiry date for the new services and the conditions under which an extension might be recommended to government, but did not otherwise discuss how the changes might be evaluated.
2.48 The Minister may add a health service to the MBS by making a 3C determination. The power to make a 3C determination has been delegated to specified senior executives within Health. 3C determinations were used as the mechanism to implement the expansion of telehealth in response to the COVID-19 pandemic.
2.49 Health advised the ANAO that making a 3C determination is an established process that is suited to implementing changes to the MBS that are temporary or urgent. Although only partly documented, the ANAO found that the roles and responsibilities, and steps in the process of implementing a 3C determination, were well understood.
2.50 The further expansion of telehealth between March and July 2020 was implemented incrementally, with Health adopting the terminology of ‘staged implementation’ to describe changes made in this period. On 23 March 2020 Health issued a fact sheet that categorised actions taken since 13 March 2020 into three stages, and stated that a fourth stage would be conducted (Figure 2.1).
Figure 2.1: Telehealth expansion implementation stages 1–4 outlined in Health fact sheet, 23 March 2020
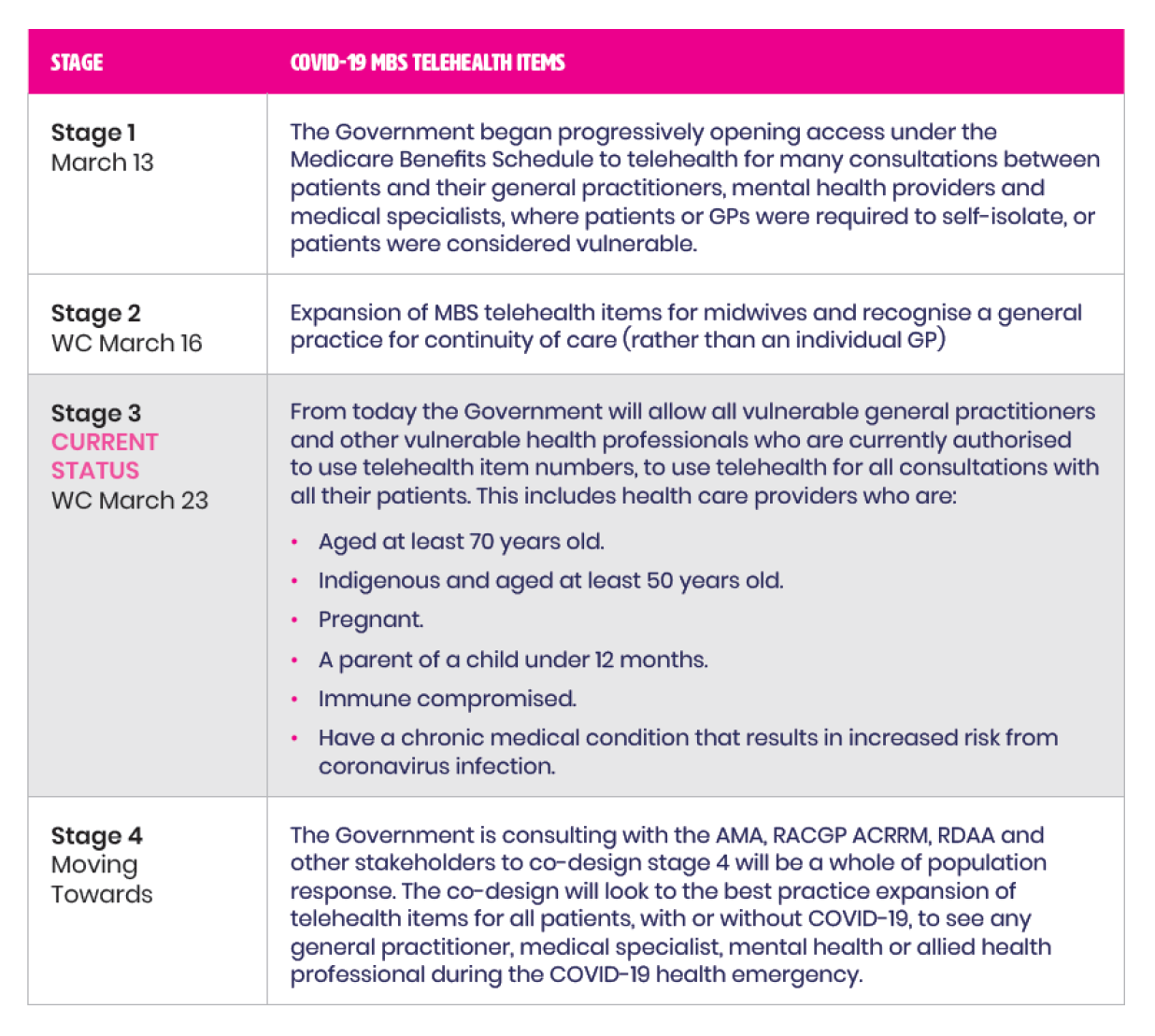
Note: On 30 March 2020 Health provided further policy advice to the government regarding Stage 4. Health advised that approximately 70 new telehealth items would be implemented via a 3C determination, but due to operational limitations might not be implemented in one tranche. Health advised that it had already solicited stakeholder advice on implementation priorities in the event progressive implementation of the items would be necessary.
Source: Health records.
2.51 Two further implementation stages are outlined in Health documentation.
- Stage 5 — Policy advice on 30 March 2020 foreshadowed that further advice would be provided regarding a future Stage 5, which would consider a range of specialist items for expansion. On 3 April 2020 Health requested the Minister approve a ‘stepped approach to implement stage 5 of the Government’s response to COVID-19’, and subsequently progressed this stage in three tranches.
- Stage 7 — On 10 July 2020 the Minister announced the reintroduction of the requirement for telehealth patients to have an existing clinical relationship with the provider, and referred to this change as Stage 7 of the telehealth reforms.
2.52 ANAO identified inconsistent usage of the term ‘Stage 6’ in departmental records to refer to the second and third tranches of Stage 5. The ANAO also identified records that referred to the first tranche of Stage 5 changes as part of Stage 4. These inconsistencies illustrate that Health did not maintain a reliable reference that tracked what implementation activities occurred in each stage and how these stages related to one another. Health advised the ANAO that the discrepancies are a reflection of the operational pressures of the COVID-19 response at that time.
Implementation plan for transition to permanent telehealth
2.53 In April 2021 Health provided advice to the Australian Government that set out its implementation plan at a high level for a transition from temporary to permanent telehealth settings. The plan clearly outlined deliverables and timeframes for delivery up to 31 December 2021, and proposed that permanent telehealth items would commence on 1 January 2022 with the exact settings to be determined closer to that date. Health noted that the permanent telehealth implementation plan and 10 Year Plan were interdependent and the permanent telehealth implementation plan addressed the interaction between the two plans.
2.54 The permanent telehealth implementation plan discussed including GP telehealth items in the ‘80/20 rule’.37 At the time the advice was provided to the Australian Government, the proposed implementation date for this deliverable could not be met due to resourcing constraints in business areas within Health responsible for preparing the necessary legislative changes.
2.55 The permanent telehealth implementation plan was updated in December 2021 advice to government. The updated plan clearly outlined deliverables and timeframes in 2022 and 2023 (including the introduction of a new ‘30/20 rule’ from 1 January 2022)38 and addressed the interaction between permanent telehealth and the implementation of voluntary patient registration.
2.56 Neither the April 2021 or December 2021 advice contained detailed plans for performance monitoring or evaluation for permanent telehealth.39
2.57 Shortly after the Minister announced the Australian Government’s plan to implement permanent telehealth on 13 December 2021, there was an outbreak of the Omicron variant of COVID-19. Implementation activities deviated from the permanent telehealth implementation plan in response to the outbreak. Deviations included:
- on 17 January 2022, reinstating temporary telehealth items that had expired on 31 December 2021, with a new expiry date of 30 June 2022; and
- on 20 January 2022, removing telehealth items from the 80/20 rule and repealing the 30/20 rule.40
2.58 Submissions to the audit relating to the implementation approach adopted by Health are summarised in Table 2.2. A consistent theme was that the number, frequency and speed of changes to telehealth arrangements was problematic for some stakeholders.
Table 2.2: Feedback on the implementation approach in submissions to the audit
|
Nature of feedback |
Number (%) of submissions providing feedback on the implementation approach |
|
Stated that changes to telehealth settings were made abruptly or without sufficient notice |
9 (29%) |
|
Accepted that rapid and flexible implementation was necessary to respond to the pandemic |
8 (25%) |
|
Stated the frequency of changes to telehealth settings created confusion |
6 (19%) |
|
Expressed appreciation for the personal implementation efforts of Health officials |
4 (13%) |
|
Stated the expiry, extension and/or reinstatement of temporary items over short timeframes prevented long-term decision making by businessesa |
3 (10%) |
|
Stated the frequency of changes to telehealth settings increased costs to businessesb |
2 (6%) |
Note a: For example, investing in hardware, software, or staff training to provide telehealth via videoconference.
Note b: For example, by necessitating updates to billing systems, education and training of staff, and communications to patients on service options and costs.
Source: ANAO analysis of 31 submissions to the audit.
3. Implementation arrangements
Areas examined
This chapter examines whether the telehealth expansion was supported by sound implementation arrangements.
Conclusion
The Department of Health and Aged Care implemented significant changes to the Medicare Benefits Schedule and in doing so provided largely appropriate support to delivery partners. However, the telehealth expansion was only partly supported by sound implementation arrangements. Although the Department conducted risk-based post-payment compliance activities, the governance arrangements for the implementation of temporary telehealth involved inadequate assessment of the implementation and integrity risks.
Areas for improvement
The ANAO made two recommendations to the Department of Health and Aged Care. The first was to strengthen its systems of control for the implementation of material changes to the Medical Benefits Schedule, to embed elements of governance that are currently unaddressed. The second recommendation was that implementation, integrity and other risks to proposed material changes to the Medicare Benefits Schedule are subject to a structured and documented risk assessment.
The ANAO also suggested that Health could work with Services Australia to improve practices for the consideration, approval and record keeping of External Costing Requests.
3.1 The delivery of Medicare Benefits Schedule (MBS) changes relating to telehealth needed fit-for-purpose governance arrangements; collaboration with and support to delivery partners; a structured approach to managing risks to successful implementation; and an assessment of how integrity risks associated with new telehealth items could be mitigated.41
Were governance arrangements fit-for-purpose?
Standard procedures used by Health to implement telehealth changes to the MBS did not require key implementation decisions and plans to be documented, implementation and integrity risks to be managed, or performance monitoring and evaluation plans to be considered. As a result, Health’s governance arrangements for the expansion of telehealth were not fit-for-purpose. Health’s project management framework provides suitable governance arrangements, but it was not used.
Senior management oversight
3.2 Accountability for the MBS rests with the Secretary of the Department of Health and Aged Care (Health) and the Services Australia Chief Executive Officer (who is also the Chief Executive of Medicare).
3.3 The Secretary of Health is assisted by two standing advisory committees (the Program Assurance Committee and the Digital, Data and Implementation Board) with mandates that include providing oversight of new measures affecting the MBS. The committees report to the Executive Board. Neither committee provided material oversight of the expansion of telehealth in 2020 and 2021.
3.4 In February 2020 Health suspended the operation of the Program Assurance Committee and the Digital, Data and Implementation Board. A temporary COVID-19 Working Group was established in March 2020 to oversee the department’s primary and aged care pandemic response measures. Similar to the standing committees, the working group was co-chaired by two Deputy Secretaries, and intended to coordinate and report to the Executive Board on the status of the pandemic response measures. The COVID-19 Working Group was wound up in May 2020 at which time the operation of the two standing committees was resumed.
Operational governance
3.5 Within Health, two divisions within the Health Resourcing Group have primary responsibility for the MBS (Figure 3.1). These are:
- Medical Benefits Division, which is responsible for policy proposals to change the MBS, implementing changes to the MBS, and Medicare program outcomes; and
- Benefits Integrity and Digital Health Division, which is responsible for protecting the integrity of Medicare payments and supporting healthcare providers with education and information on the appropriate use of Medicare.42
3.6 The COVID-19 Working Group understood that the Medical Benefits Division was accountable for the COVID-19 expansion of telehealth. Other divisions within Health (such as Primary Care Division) may be responsible for policy initiatives that require consequential changes to the MBS. Where this occurs, Medical Benefits Division implements the required changes to the MBS following direction from the policy division.
Figure 3.1: Main business units involved with telehealth changes, 2020 to 2022

Source: ANAO analysis of Health records.
Standard procedures for implementing Medicare Benefits Schedule changes
3.7 Health has a documented standard process that outlines functional responsibilities for developing new policy proposals for consideration by the Australian Government.
3.8 Health’s internal standard procedures for implementing changes to the MBS are largely undocumented. Documented processes focus primarily on providing guidance to staff within Medical Benefits Division on the process of drafting legislative instruments to give new MBS items legal effect. These procedures are not controlled documents, meaning there is no record that the content has been approved by a Senior Responsible Officer and there are no controls to ensure staff follow the most current version of the procedure. The standard procedures do not require key decisions or implementation issues to be recorded; require implementation and integrity risks to be managed; provide mechanisms for senior responsible officers in separate divisions to share oversight and management of shared risks; require performance monitoring or evaluation of new items to be considered; or key activities such as stakeholder consultation and implementation planning to be documented.
3.9 In 2019 Health and Services Australia developed the ‘New and Changed Work Protocol’ (the Protocol), which forms part of a bilateral agreement between the organisations (discussed further in paragraph 3.35). The Protocol outlines a generic process and checklist for developing and implementing changes to Services Australia systems at the request of Health (as would be required when MBS billing systems are updated to reflect new and changed MBS items). The process provides for:
- the use of co-design sessions to discuss elements of a change proposal;
- developing documentation to support the change process (see paragraph 3.37);
- ensuring appropriate approvals are made at specific points in the development process; and
- quality assurance of the proposed solution and validation as appropriate.
3.10 The generic process and checklist outlined in the Protocol are not supported by documented specific procedures or guidance that could assist staff in the Medical Benefits Division to apply the process to changes to the MBS.
3.11 Between May and July 2020 Health conducted a live assurance review of the telehealth expansion, which examined governance arrangements specific to the telehealth response measure. The review found issues with documentation and data collection; and the application of the new policy proposal process (Box 1). The ANAO found that the issues identified by the review were authorised by senior Health officials in March 2020 in order to meet rapid implementation deadlines.
|
Box 1: Live assurance review of early telehealth expansion |
|
A live assurance review of the initial telehealth expansion was undertaken by EY with the objective to ‘assess the appropriateness of the department’s governance and control arrangements in place to support the rapid implementation of the telehealth program’. In a report provided in July 2020, EY observed that:
On 20 October 2020 a summary of the report and Health’s response to it was presented to the Audit and Risk Committee, with proposed actions including updating policy and procedural guidance for future emergency response; reviewing procedures to update and maintain the risk register to ensure process is followed; and investigating how to best improve data collection to evaluate financial risk and usage trends. Health advised the ANAO in December 2022 that since that time it has continued to engage with stakeholders, adapt and enhance its reporting and data analytics capability and compliance tools; and that it is still considering other suggestions in the report. |
Project management framework
3.12 The COVID-19 Working Group and standing oversight committees used a reporting tool called ‘Health Tracker’ to assign responsibility for COVID-19 response measures to a Senior Responsible Officer and to monitor progress towards outcomes. The tool comprises two parts.
- ‘Health Tracker — Planner’ is used to prioritise, monitor and report to stakeholders on the department’s progress in implementing initiatives such as election commitments, budget measures and ministerial announcements. Initiatives tracked as items in ‘Health Tracker – Planner’ are not required to be managed as projects in accordance with Health’s project management framework.43
- ‘Health Tracker — Implementation’ is used for tracking and reporting on projects. Projects in ‘Health Tracker – Implementation’ must follow Health’s project management framework and templates.44
3.13 The ANAO identified four ‘Health Tracker – Planner’ items covering the expansion of telehealth services to March 2022.
- The first item concerned the expansion of telehealth in March and April 2020, and was reused for further telehealth changes between April to December 2021.
- Two items were created to track the extension of GP and allied health telehealth, and specialist telehealth, from October 2020 to April 2021.
- The fourth item tracked the transition to permanent telehealth in January to March 2022.
3.14 Two ‘Health Tracker – Implementation’ items were created in September 2020 covering: an expansion of mental health services with consequential changes to telehealth items on the MBS; and the extension of temporary specialist telehealth services.
3.15 Despite the existence of some ‘Health Tracker – Implementation’ items, the telehealth expansion was not managed as a project in accordance with Health’s project management framework.
- Although Health’s project management framework gives Senior Responsible Officers the discretion to decide that initiatives in ‘Health Tracker – Planner’ do not need to be managed in accordance with the project management framework, the project management framework also states that new policy proposals and budget initiatives will ‘typically be run as a project, as they are discreet packages of work that will deliver a change’.
- Documentation required under Health’s project management framework for the two relevant ‘Health Tracker – Implementation’ items was incomplete or not developed.
- Health retrospectively drafted project management documentation in May 2020 for the initial telehealth extension commencing in March 2020. These documents were provided to the live assurance review undertaken in May to July 2020 (discussed in Box 1). There is no record that the documents were formally approved or materially governed expansion of telehealth items on the MBS.
3.16 In April 2022 Health introduced a new rapid implementation framework. The rapid implementation framework, which operates in conjunction with the project management framework, permits projects to be managed with abbreviated project governance arrangements in exceptional circumstances if approved to do so by Health senior management. This includes scenarios where compliance with the usual processes set out in the project management framework is not feasible due to the urgency of implementation. The rapid implementation framework does not apply to initiatives that the senior responsible officer decides should not be managed as a project.
3.17 Administering initiatives that involve material changes to the MBS in accordance with Health’s project management or rapid implementation frameworks would strengthen the controls over those changes.
Recommendation no.1
3.18 The Department of Health and Aged Care strengthen its systems of control for the implementation of material changes to the Medicare Benefits Schedule, to embed elements of governance that are currently unaddressed including documentation of key implementation issues and decisions, and planning for performance monitoring and evaluation.
Department of Health and Aged Care response: Agreed.
3.19 The ANAO noted that implementation of expanded MBS telehealth items prioritised rapid deployment and the normal Department of Health and Aged Care program management framework was not adhered to, nor was there exemption from this requirement. Whilst noting this, routine business and governance processes that were followed include obtaining relevant policy authority, drafting regulations through normal processes, communication to stakeholders and post implementation review processes.
3.20 The Department’s framework for implementation planning and tracking may be appropriate for measures of significance, though it is optimised for programs other than the MBS which undergoes many amendments annually. For reference between March 2020 and September 2022 there were 1,117 new MBS items created; 1,276 items ceased; and 3,889 item descriptor amendments. The Department is taking steps to formalise, at the policy development stage, consideration of whether MBS amendments are ‘material’ and therefore should be managed as a project, whether additional specific post-implementation evaluation is required; and if so, identification of relevant resources required and suitable timing.
Were implementation risks effectively managed?
Health did not manage implementation risks associated with temporary or permanent telehealth changes in accordance with its risk management policy.
3.21 Successful implementation of a new initiative relies on the identification and management of risks that may hamper the introduction and administration of the change. The risks of a change need to be managed until the initiative has successfully transitioned to business-as-usual. Rapid implementation may alter risk appetite and tolerance but does not alter the need for effective risk management.
Health’s risk management framework
3.22 Throughout the period of the telehealth expansion, Health maintained a risk management policy as required by the Commonwealth Risk Management Policy. Health’s risk management policy:
- nominated the Commonwealth Risk Management Policy and AS/NZS ISO 31000:2009 Risk Management – Principles and Guidelines as standards of reference for risk management at Health;
- defined Health’s risk management approach, risk appetite and risk tolerance; and
- set out the key accountabilities and responsibilities for managing and implementing Health’s risk management framework.
3.23 At the time of the initial telehealth expansion in March 2020, Health’s risk tolerance as expressed in its risk appetite statement was permissive of policy, delivery and governance risks and restrictive for regulation, use of information and mismanagement of administered funding risks.
3.24 Health’s risk management policy allocated specific responsibilities to senior officials for managing program and project risks. First Assistant Secretaries were responsible for identifying, managing and reporting new and emerging risks; updating divisional risk registers either quarterly or more often if required; and embedding risk management into all key business processes.
Divisional risk management
3.25 In its 2019–20 Annual Report, Health described the rapid introduction of temporary telehealth in response to COVID-19 as ’10 years of reform in only 10 days’, and the 2022–23 Budget described the introduction of permanent telehealth as ‘the most significant structural reform to Medicare since it began’. The expansion of telehealth posed risks for multiple divisions within Health, including new shared risks.
3.26 Medical Benefits Division, Benefits Integrity and Digital Health Division, and Primary Care Division risk registers for 2019–20 and 2020–21 did not contain any telehealth-specific risks. The registers were not reviewed on a quarterly basis as required under the risk management policy and the events of 2020 did not prompt an out-of-cycle review of divisional risk registers to ensure their currency.
3.27 The ANAO reviewed business and risk planning documents aligned to the annual corporate planning cycle for these three divisions.
- Neither the Primary Care Division nor the Benefits Integrity and Digital Health Division identified or assessed risks relating to the implementation of telehealth within these documents.45
- In 2020–21 Medical Benefits Division identified three divisional-level risks relating to telehealth (Table 3.1). The risks were not evaluated to determine whether the risks were within tolerance or required further treatment.
Table 3.1: Telehealth risks identified in Medical Benefits Division 2020–21 divisional business plan
|
Target |
Risks to achieving our target |
|
The department funded a significant expansion of MBS telehealth services from March 2020 to ensure the community could continue to access [general practitioner] and Allied Health services whist maintaining COVID Safe practices, including physical distancing. |
Government offsetting rule means that new services need to be funded through identified offsets.a Increased priority of Medicare within Government is driving increased data requests and media interest up. Insufficient dedicated resources may compromise target and timeframes being met. |
Note a: The offsetting rule requires entities to identify savings within the existing portfolio budget commensurate with the additional spending proposed in a new policy proposal.
Source: ANAO reproduced from Health records.
- In 2021–22, Medical Benefits Division identified one divisional-level risk relating to telehealth (Table 3.2). Two existing controls were identified for this risk. The plan did not document an assessment of the effectiveness of the controls. No further treatments for the risk were specified in the plan.
Table 3.2: Telehealth risks identified in Medical Benefits Division 2021–22 divisional business plan
|
Priority |
What are the risks that would stop us from achieving our priorities? |
What are we currently doing to manage those risks? |
How could areas of risk be better managed, resources permitting? |
|
Supporting the health response to COVID-19 including providing access to telehealth services, vaccination assessment services and pathology testing through the MBS. |
Transition to permanent MBS telehealth arrangements following expiry of current arrangements on 31 December 2021, including need for sector support, Ministerial and Government agreement, timely transition from current arrangements. |
Ongoing internal and external key stakeholder engagement to ensure appropriate policy settings, including with peak stakeholders and other relevant policy areas in the Department. |
[No entry recorded]a |
|
Ongoing cost modelling and engagement with Department of Finance. |
[No entry recorded]a |
||
Note a: Health advised the ANAO that these fields were left blank as the existing controls listed in the preceding column were considered sufficient to manage the risk.
Source: ANAO reproduced from Health records.
Operational risk management
3.28 Health maintains standard operating procedures for amending the MBS through a 3C determination (see paragraph 3.8). Although Health’s Risk Management Policy requires risk management to be embedded into key business processes, the standard operating procedures included no requirement to conduct a structured assessment of the risks of material changes to the MBS before implementation, or to monitor and manage implementation risks for a period after the introduction of the material change.
3.29 As discussed in paragraph 3.15, the expansion of telehealth was not governed as a project and accordingly did not require the preparation and use of a risk register using the template provided under Health’s project management framework. Despite this, in May 2020 staff from Medical Benefits Division supported by Health’s Corporate Assurance Branch developed a draft risk management plan and draft risk register. The draft plan and register were not finalised and were not used in practice to inform decision making and implementation activities.
3.30 The draft risk register identified 14 operational risks associated with the expansion of telehealth between March and May 2020, of which six were assessed and assigned a risk rating. The first risk identified was ‘failure to appropriately implement risk management into the project’, which was assessed as ‘acceptable’.
3.31 The ANAO identified two significant implementation risks for the expansion of telehealth services that were not managed by Health (Box 2 and Box 3).
|
Box 2: Identification of risk after it had materialised |
|
On 23 March 2020 the Minister for Health (the Minister) announced that as part of the introduction of whole of population telehealth, the bulk billing incentive for providers would be temporarily doubled for both face-to-face and telehealth services from 30 March 2020 onwards.a Costings were prepared for the Australian Government on the basis that the doubling would only apply to services on the General Medical Services MBS table.b To speed implementation, Health decided to draft regulations for the changes in parallel with seeking policy authority. On 3 April 2020 the Department of Finance notified Health that factsheets on MBS Onlinec suggested the incentive had also been doubled for Pathology and Diagnostic Services, outside of the approved policy. Health advised the Minister through his office about the error, and prepared revised costings for these additional incentives, which estimated a cost of $1.594 million. The May 2020 draft operational risk register identified as a risk ‘execution of the planned changes exceeds what was initially approved by the Minister.’ A possible cause of the risk was listed as rapid changes to the scope of proposed legislative amendments not captured through normal mechanisms. |
Note a: The bulk billing incentive is a set of MBS items that can be billed at the same time as a bulk billed health service. The incentives are intended to promote the provision of bulk billed services to vulnerable patient groups. The incentives can be billed in conjunction with face-to-face or telehealth services.
Note b: MBS items are listed in one of three tables (general medical services, pathology services, or diagnostic imaging services) that are ordinarily prescribed in regulations made under the Health Insurance Act 1973.
Note c: MBS Online [www.mbsonline.gov.au] is a webpage used to publish the MBS and accompanying guidance.
|
Box 3: Failure to identify and manage legal risk |
|
Under the Health Insurance Act 1973, a patient may agree to assign a Medicare benefit so that it is paid directly to the provider (known as ‘bulk billing’). The agreement must be made in accordance with the approved form, which requires the patient’s signature. Guidance for pre-pandemic telehealth provided that the signature could be obtained via email, fax or mail. The guidance stated that writing ‘telehealth’, ‘verbal consent’ or ‘patient unable to sign’ on the form to overcome administrative difficulties would not meet the requirement.a On 16 March 2020 Services Australia contacted Health requesting clarification of signature requirements for temporary telehealth items introduced in response to COVID-19. On 24 March 2020 Health advised that due to the ‘exceptional and temporary circumstances’ of the pandemic, providers could document in the provider’s clinical notes that the patient had provided verbal consent. Health decided on several occasions between 2020 and 2022 to extend these temporary arrangements. Health did not assess the legal risk associated with this temporary policy, consider whether the risk could be mitigated through additional controls, or formally assign responsibility for monitoring the risk, as required by its risk management framework. Health senior officials did not seek legal advice about the temporary arrangements, despite senior Health executives receiving notice of concerns held by departmental officers in March 2020 about potential legal and fraud risks associated with the policy. Public-facing guidance on the temporary policy did not clarify that notating verbal consent in provider records alone could not address other statutory requirements requiring a signed copy of the agreement to be provided to the patient. The legal consequences of failing to observe such requirements can be severe. Where a provider does not provide a copy of the signed agreement in approved form to the patient, there is no legal basis for Services Australia to pay the benefit to the provider. Additionally, providers can be criminally liable for failing to complete the agreement form properly.b |
Note a: The guidance stated that the provider writing ‘patient unable to sign’ is an acceptable substitute for the patient’s signature in limited circumstances, such as where the patient does not have a guardian or relative who may sign on their behalf and is unconscious or has an injured hand.
Note b: Subsection 20B(3) and section 127 of the Health Insurance Act 1973 respectively.
Recommendation no.2
3.32 The Department of Health and Aged Care develop procedures that ensure proposed material changes to the Medicare Benefits Schedule are subject to a structured and documented risk assessment that covers implementation, integrity and other risks.
Department of Health and Aged Care response: Agreed.
3.33 The ANAO noted the heightened focus on post-payment compliance for telehealth services, employing standard MBS methodologies for payment compliance risks and associated treatments. These are based on requirements for all 5,800 plus MBS items including the telehealth items that mirror or replicate the face-to-face items. Though the Department identified relevant risks in its advice to Government, including in policy proposals, the ANAO is of the view that risk identification and treatment strategies in relation to policy development and monitoring were incomplete. In responding to this recommendation, the Department will assess how to best identify which of the many thousands of MBS changes are ‘material’, whether use of the standard Risk Potential Assessment Tool is suitable for material MBS changes and ensure that legal risks are identified and mitigated.
Was support to delivery partners appropriate and timely?
Although Health did not consistently adhere to the agreed process to govern the implementation of changes to the MBS by Services Australia, Health supported Services Australia to make rapid changes to MBS telehealth items during the initial expansion of temporary telehealth. While there was no communications plan, Health published a substantial amount of guidance material for health providers and maintained a facility for provider enquiries. Between 30 March 2020 and 12 June 2022, service standards for responding to telehealth-related inquiries were not consistently met.
3.34 Successful delivery of material changes to the MBS requires Health to provide timely, relevant and accurate information to delivery partners, including Services Australia (which administers the MBS payments system and provides billing support to providers); providers and associated business participants such as practice managers (who deliver health services and bill the MBS); and industry groups (which advise and support providers to implement new business practices).
Services Australia
3.35 Since 2018 Health has maintained a bilateral agreement with Services Australia (the Statement of Intent between the Secretary, Department of Health and the Chief Executive Officer, Services Australia (Statement of Intent)) that sets out objectives, principles and governance arrangements for joint work undertaken by the entities.46
3.36 Pursuant to the Statement of Intent, in December 2019 Health and Services Australia established the ‘New and Changed Work Protocol’ (the Protocol) that provides agreed processes, frameworks and guidelines to design, cost and implement Australian Government health policies and services. Although the Protocol provides that it will be reviewed every 12 months or more frequently if necessary, the Protocol was last updated in August 2020. Health advised the ANAO that this was because of competing operational priorities.
3.37 In accordance with the Protocol, policies that require Services Australia to deliver new services or change existing services under Health’s direction must be supported by a service delivery costing document called an External Costing Request (ECR). The ECR is intended to specify the details of the change so that Services Australia’s business and ICT teams have an agreed reference point to plan for and implement the change. The ECR must be approved by a Senior Executive Service Band 1 officer from both entities.
3.38 During the initial implementation of temporary telehealth, Health and Services Australia did not prepare ECRs to support policy changes as required by the Protocol. Services Australia advised that for this was ‘under agreement from [senior executives] for both Services Australia and Health’.
3.39 Instead of ECRs, during the initial implementation of temporary telehealth, Health used informal information sharing and liaison to inform Services Australia of likely telehealth changes that were yet to be finalised, so that Services Australia could commence preliminary work on systems changes as soon as possible (see case study 1). Services Australia staff advised the ANAO that while short lead times were provided to implement changes, Services Australia was largely comfortable with the amount of information provided informally by Health and the timeliness of this information.47
|
Case study 1. Parallel development of legislation and systems for the early telehealth policy changes |
|
Between 8 and 11 March 2020 Health advised Services Australia of the introduction of new temporary telehealth MBS items to be implemented on 13 March 2020, and provided copies of the draft 3C determinations that would give these items legal effect. On 12 March 2020 at 11:17am, following an announcement by the Prime Minister the previous day that the new telehealth services would be available by phone or videoa, Health advised Services Australia of changes to the determination to include phone services within the definition of telehealth for general practitioners. At 5:08pm Health emailed Services Australia with a workbook of MBS item numbers that was the basis for drafting the revised 3C determination before the signed 3C determination was provided at 7:34pm. Services Australia implemented the systems changes overnight so that the items could be billed by the implementation date. On 13 March 2020 Health provided the details of further phone items to Services Australia by email while simultaneously drafting an amending 3C determination to enact them. The 3C determinations were registered on 13 March 2020 with immediate effect. Services Australia implemented the further systems changes overnight, meaning that the items could be billed one day after the implementation date. |
Note a: See paragraph 2.12.
3.40 Upon request for the ECRs that supported the 16 major telehealth changes implemented between 30 March 2020 and 19 July 2022, Health provided the ANAO with seven. The ANAO also identified a further seven ECRs in Health’s records relating to these major changes. In summary, an ECR could not be found for two of the 16 major telehealth changes.
3.41 Of the 14 ECRs for which Health maintained a record, 12 were provided to Services Australia in advance of the changes being implemented, and the date of provision for the remaining two was not recorded.
|
Opportunity for improvement |
|
3.42 To ensure compliance with Health and Services Australia’s New and Changed Work Protocol and to better support the governance of MBS and other policy changes, Health could work with Services Australia to improve practices for the consideration, approval and record keeping of External Costing Requests. |
Providers and peak organisations
Communications plan
3.43 Health did not establish a communications plan for the implementation of new telehealth MBS items that forecasted the information needs of providers and peak organisations, identified the communications channels that would be used to reach these entities, or scheduled the release of change messaging and guidance materials to providers in advance of changes being made to the MBS. The absence of a communications plan resulted in issues such as the duplication of content creation between Services Australia and Health, the risk of inconsistent messaging and a lack of clarity regarding which area of Health was responsible for removing obsolete guidance. Health advised the ANAO that changes to temporary telehealth followed normal processes for communicating changes to items on the MBS and that these processes were supplemented by a broader COVID-19 communications strategy.
Communications, guidance material and other support
3.44 Health developed communications materials and engaged in communications activities to support the telehealth changes.
- Health created or updated fact sheets relating to new and amended telehealth items and published these on MBS Online. The first set of fact sheets with detailed information on the telehealth changes were published on 17 March 2020, with further fact sheets between April to June 2020 published on the dates the changes were implemented.
- AskMBS is an email-only advice service for providers for queries related to services listed on the MBS. In May 2020 Health published an ‘AskMBS Advisory’ concerning telehealth services introduced in response to COVID-19, which contained similar content to the August 2020 ‘Telehealth Items Guide’ (see sub-paragraph 3.44(f)). Health published and maintained two other ‘AskMBS Advisories’ on MBS Online containing guidance on temporary specialist telehealth items introduced in response to COVID-19 (August 2020) and the requirement for providers in general practice to have a pre-existing clinical relationship with temporary telehealth patients (December 2020).
- In March 2020 the Australian Information Commissioner requested that Health prepare a Privacy Impact Assessment (PIA) on the new temporary telehealth MBS items.48 In the course of developing the PIA, Health published a privacy ‘checklist’ for providers on 4 May 2020. Based on Health internal reporting, by this date at least 7.6 million temporary telehealth services had already been provided to a total of 4.7 million patients by nearly 69,000 providers. Health submitted the PIA to the Office of the Australian Information Commissioner on 10 June 2020.
- Health worked directly with peak organisations to assist them to provide tailored guidance to their members on issues such as assignment of benefit in the absence of a patient’s signature, telehealth-related compliance activity and clarification of compliance requirements. Health officials attended webinars hosted by Health or by key peak bodies such as the Australian Association of Practice Management and the Australian College of Rural and Remote Medicine in March and early April 2020 to answer questions about the introduction of new telehealth items.
- To support telehealth provision, between 17 April 2020 and 31 December 2022 Health offered licences to ‘healthdirect video call’, a secure video conferencing platform, at no cost to general practices, Aboriginal Medical Services and Aboriginal Community Controlled Health Organisations.
- In August 2020 Health emailed around 121,000 medical practitioners and nine peak bodies a link to a ‘Telehealth Items Guide’ which was produced to ‘support health professionals in understanding the requirements associated with telehealth items and their appropriate use’. Two submissions to the ANAO provided feedback that the guide was a good initiative, however its usefulness was limited by delays in its distribution and a failure to update the guide to reflect policy changes on a timely basis.
Responding to provider enquiries
3.45 In the 12 months to March 2020, AskMBS received and closed an average of 579 and 549 inquiries per month, respectively. In March 2020 AskMBS received 1603 inquiries, 2.8 times the monthly average in the preceding 12 months. The increase in AskMBS inquiries coincided with the implementation of telehealth on 13 March 2020, and there was a substantial spike in telehealth-related inquiries with the introduction of whole of population telehealth on 30 March 2020 (Appendix 3). Over 5000 telehealth-related inquiries were received between 1 January 2020 to 14 June 2022.
3.46 Prior to August 2021 Health had an internal target to respond to AskMBS queries within 10 working days (except for complex questions requiring input from policy areas). The target was changed to 15 working days in August 2021 due to consistently high volumes of inquiries. The average response time for telehealth-related inquiries (measured as the average time taken by Health to respond to inquiries received in a specified week) ranged from nine working days in the week commencing 9 March 2020 to 25 working days in the weeks commencing 8 June 2020 and 26 October 2020. The average response time for telehealth-related inquiries exceeded service standards for 66 of the 115 weeks between 30 March 2020 and 12 June 2022.
3.47 Although AskMBS was an established channel for provider enquiries, between 30 March and 19 April 2020 Health included a dedicated email address for telehealth-related inquiries as part of some of the initial telehealth factsheets published on MBS Online, with telehealth inquiries being directed to a different email address and queries for all other MBS items being directed to AskMBS. Internal reporting recorded 414 telehealth-related inquiries being received at this email address, with around 90 per cent of these received by 30 April 2020.
Reported difficulties with support to providers
3.48 Of the 31 submissions to the audit, 15 provided feedback on the support provided by Health for the implementation of telehealth (Table 3.3). Feedback about the quality and timeliness of services and communications included comments about fact sheets being regularly updated but delays in information being provided on specific issues.
Table 3.3: Feedback on Health support to providers in submissions to the audit
|
Nature of feedback |
Number (%) of submissions providing feedback about support to providers |
|
The quality and timeliness of policy guidance was variable |
6 (19%) |
|
Policy guidance provided limited support |
4 (13%) |
|
Technology guidance provided limited support |
3 (10%) |
|
The quality of advice was adequate |
2 (7%) |
Source: ANAO analysis of 31 submissions to the audit.
Were integrity risks for the new arrangements effectively managed?
Health did not conduct a risk assessment of integrity risks, such as provider fraud and non-compliance, prior to implementing the temporary and permanent MBS telehealth items. Treatments to prevent provider non-compliance with telehealth items were limited. There is a risk-based model for detecting and treating provider fraud and non-compliance. Corrective non-compliance treatments were applied to a subset of non-compliant providers in accordance with this model and focused on the most egregious non-compliance behaviours.
3.49 Two divisions in Health have responsibilities related to managing the risk of fraudulent and non-compliant MBS claiming by providers. Health’s risk management policy provides that risks shared between different areas of Health require shared oversight and cooperation to understand and effectively manage the risk.
Compliance risk assessment
3.50 Between 2020 and 2022 Health’s procedures for changing the MBS did not require a structured assessment of integrity risks. A structured assessment prior to implementation might include:
- the identification of potential integrity risks for proposed telehealth MBS items;
- an assessment of whether identified risks associated with specific MBS items could be prevented or mitigated through preventative (pre-payment) treatments such as legislative design (such as the item descriptor or claiming restrictions), implementation strategies, or automated controls within MBS billing systems49;
- a documented decision on whether the risks fell within risk tolerances, and for shared risks, which risk tolerance was applicable if tolerances were different50; and
- the assignment of responsibility for implementing any necessary risk treatments.
3.51 In the absence of a structured assessment of integrity risks for new telehealth items, officials from Medical Benefits Division and Benefits Integrity and Digital Health Division used standing interdivisional meetings and other informal means to discuss the compliance implications of the items.
Pre-payment treatment of integrity risks
3.52 Although it did not conduct a structured assessment of integrity risks of new telehealth items, or the sufficiency of existing controls, Health advised the Australian Government that integrity risks specific to the temporary telehealth items would be adequately managed by post-payment (corrective) regulatory activity.
3.53 In relation to potential preventative treatments during the temporary telehealth expansion, Health officials advised the ANAO that automated pre-payment controls over eligibility criteria for telehealth MBS items would have been impractical in the context of the initial pandemic response. Moreover, Health advised the ANAO that few practical options were available with the IT systems at the time for implementing such treatments.
Post-payment treatment of integrity risks
3.54 Health uses several treatments for health provider fraud and non-compliance (Table 3.4). With the exception of education, the treatments are corrective and apply after an MBS service has already been billed.
Table 3.4: Treatment types for health provider non-compliance
|
Treatment type |
Description |
|
Education |
Awareness raising and other activities to support providers whose compliance does not warrant individualised compliance activity. |
|
Targeted Letter |
Low-cost treatment to encourage voluntary compliance. Health sends a schedule of services claimed by the provider requesting the provider review and correct any non-compliant claims through a voluntary acknowledgement of debt. |
|
Audit |
Audits to assess and verify claims that do not comply with the requirements of the MBS. Compliance officers are able to exercise statutory information gathering powers, raise a debt to recover non-compliant payments and apply an administrative penalty. |
|
Practitioner Review Program |
Clinical review of billing practices, used to address potential inappropriate practice by a provider (for example, conduct in connection with rendering or initiating MBS services that would be considered unacceptable to the general body of the provider’s peers). |
|
Investigation |
A criminal investigation of fraudulent Medicare claims by a provider, such as claiming a rebate where no medical service has been provided. |
Source: Adapted from Auditor-General Report No. 17 2020–21 Managing Health Provider Compliance.
3.55 In 2020 Health adopted a new compliance operating model known as 1CAB to improve its post-payment prioritisation and treatment of potentially non-compliant billing behaviour (Figure 3.2).51
Figure 3.2: Treatment of non-compliance through 1CAB model
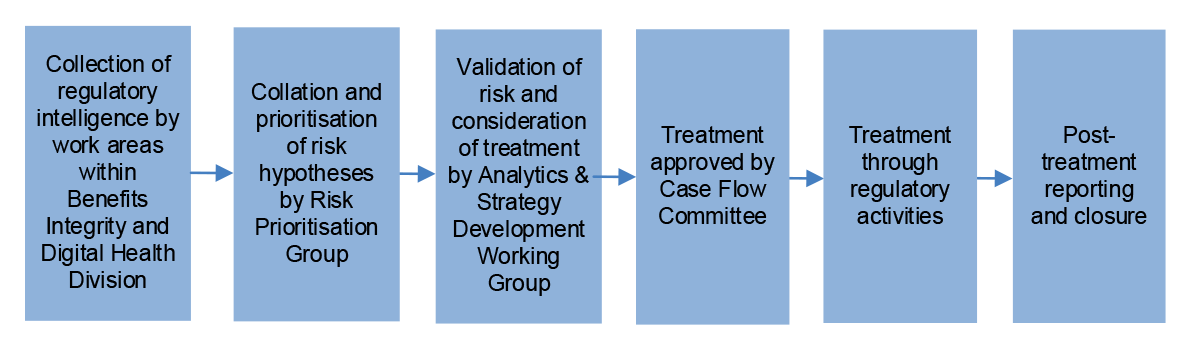
Source: ANAO analysis of Health records.
3.56 Health incorporated telehealth risks into the 1CAB model, and completed telehealth compliance activities largely in line with the model. Between March 2020 and July 2022, Health identified 600 potentially non-compliant or fraudulent claiming behaviours, of which 23 related to misuse of telehealth MBS items. Seven of the 23 behaviours relating to telehealth were chosen for formal risk assessment and four were ultimately approved for treatment (Table 3.5). Health advised the ANAO that the decision to assess the risk of a potentially non-compliant or fraudulent behaviour is informed by several considerations such as the capacity of analytical and operational teams, the significance and urgency of the issue, and whether there has been recent compliance activity in that area.
3.57 The treatment strategies applied compliance treatments that aimed to be proportionate to identified compliance risk. Providers were selected for treatment based on outlier behaviour that exceeded criteria expressed in absolute terms (such as exceeding a threshold number of potentially non-compliant services) or based on a peer-comparison (such as the top 90th percentile of providers displaying the identified behaviour).
Table 3.5: Telehealth risks considered for treatment by Health, March 2020 to July 2022
|
Potentially non-compliant behaviour approved for treatment |
Estimate of population of providers potentially exhibiting non-compliant behavioura |
Initial number of providers approved for compliance action |
Endorsed treatment strategy for the risk |
|
Providers submitting claims for multiple family members on the same Medicare card without providing a service to each person (‘family servicing’) |
40 |
11 |
Referred for investigation, or alternative audit action if it is determined the case is not suitable for investigation |
|
Co-claiming multiple telehealth and/or face-to-face attendances for the same service |
17 |
7 |
Phase A: To be evaluated for possible referral to the Professional Services Review |
|
13 |
Phase B: Referred for alternative audit action |
||
|
Potential non-compliance with COVID-19 telehealth continuous care requirementsb |
23,149 |
17 |
Stage 1: Referred for audit |
|
28 |
Stage 2: Referred for audit |
||
|
730 |
Stage 2: To receive a targeted letter |
||
|
9465 |
Stage 2: To receive a generic (non-targeted) education and awareness raising letterc |
||
|
Claiming a more expensive COVID-19 telehealth item than the actual service provided (‘up-coding’) |
349 |
6 |
Stage A: To be evaluated for possible referral to the Professional Services Review |
|
7 |
Stage B: To be evaluated for possible referral to the Professional Services Review |
||
Note a: This column shows the number of providers exhibiting a pattern of claiming considered under the risk at a point-in-time. They do not represent a confirmed assessment of the prevalence of a non-compliant pattern of claiming. Health advised the ANAO that the final threshold for intervention considers analysis and research, medical advice and stakeholder input. This then results in the number of providers recommended to be approved for compliance action.
Note b: The continuous care requirement refers to the requirement for a telehealth provider in general practice to have a pre-existing clinical relationship with a patient. On 20 July 2020 Health reintroduced a requirement that providers must have a pre-existing clinical relationship with a telehealth patient, defined as one face-to-face service in the preceding 12 months.
Note c: The approved strategy was subsequently revised; no awareness raising letters were sent, 457 providers were selected for a targeted letter and 37 providers were audited.
Source: ANAO analysis of Health records.
3.58 Three of the four telehealth risks approved for treatment were executed as planned. The treatment approach to the remaining risk (potential non-compliance with continuous care requirements) was revised following further consultation with peak bodies52 and new targeting data. Health discontinued plans to send generic awareness letters to over 9000 providers following consultation with peak bodies. Shortly before sending the targeted letters, Health identified that its targeting methodology was affected by a data issue that produced false positive results. Health discontinued plans to audit or send targeted letters to 77 providers, transitioned seven providers to less invasive treatments, and discontinued action against one provider.
3.59 In addition to non-compliance identified through the 1CAB model, Health may also identify and treat potential non-compliance in response to tip-offs received from the public. The ANAO examined a manually collated spreadsheet of 456 tip-offs received between 13 March 2020 and 30 June 2021 that contained allegations of non-compliant or inappropriate MBS claiming in relation to telehealth. The spreadsheet identified 137 tip-offs that were sufficiently substantiated to warrant further examination.53 As of August 2022, 76 of these cases had been treated with regulatory activity, 59 had been evaluated and closed without treatment, and two remained under evaluation for potential treatment.
4. Monitoring and review
Areas examined
This chapter examines whether monitoring and evaluation of the telehealth expansion led to improvements.
Conclusion
The Department of Health and Aged Care (Health) did not plan for performance monitoring or evaluation of temporary or permanent telehealth. Performance monitoring of the temporary telehealth expansion was limited and lacked measures and targets that could inform judgements about performance, and there was no evaluation that could assist with the design and implementation of potential expansions to telehealth during future emergency conditions. Evaluation of permanent telehealth is developing.
Areas for improvement
The ANAO made two recommendations aimed at capturing the lessons of COVID-19 telehealth as a pandemic response and settling plans for the evaluation of permanent telehealth.
4.1 Australian Government guidance such as the Delivering Great Policy Model and the Australian Government Guide to Regulatory Impact Analysis provide that entities should plan at the outset for how performance against intended policy outcomes will be measured, monitored, and evaluated.
4.2 Monitoring and evaluation of material changes to the Medicare Benefits Schedule (MBS) could examine whether the changes support:
- affordable and universal access to health care;
- the provision of contemporary best practice health services;
- the delivery of services that are appropriate to the patient’s needs and that do not expose patients to unnecessary risk or expense; and
- improved value for the health system by preventing or reducing funding for health services with little or no clinical value.
4.3 The Australian Health Sector Emergency Response Plan for Novel Coronavirus (COVID-19 Plan) provided that measures under the COVID-19 Plan (such as temporary telehealth arrangements) should be regularly reviewed and tailored to ensure they remain effective and proportionate to risk. The COVID-19 Plan further provides that after measures under the COVID-19 Plan have transitioned to normal business, an evaluation of the response should rapidly occur so that lessons from the pandemic can be applied to subsequent waves of COVID-19 or future pandemics.
Were performance measures established and monitored?
Health did not establish performance measures for the telehealth expansion. Health used Medicare Benefits Schedule billing data to monitor telehealth usage patterns, on the assumption that telehealth usage and billing behaviours were sufficient indicators of successful telehealth implementation. There were no performance targets.
Planning for monitoring performance
4.4 Health did not establish a plan to monitor the expansion of telehealth in 2020 and 2021 against expected results. In the initial telehealth expansion between March and May 2020, and in planning further changes after this time, Health did not nominate criteria against which the achievement of policy objectives would be measured, or what data would be necessary to accurately and sufficiently measure performance. Health did not document the allocation of roles and responsibilities for monitoring performance, the frequency and format of performance reporting, or the approval of these arrangements by senior officials. Advice provided to the Australian Government in December 2021 stated it was ‘critical’ that ‘telehealth services are patient-focussed, based on patient need and do not undermine the role of face-to-face care, consistent with the principles outlined by the MBS Review Taskforce Telehealth Recommendations 2020’ but did not identify how Health would obtain assurance that these critical requirements were met.
4.5 Health officials advised the ANAO that to the extent compliance with the MBS was an indicator of telehealth performance, Health’s provider compliance framework provided an existing mechanism for monitoring performance.54 Moreover, Health officials advised the ANAO that because every telehealth service provided is by nature a socially-distanced health service that would reduce the risk of COVID-19 transmission between provider and patient, usage of telehealth services was an indicator of success. The uptake of telehealth services was measurable in MBS billing records.
4.6 Health’s decision to design most telehealth MBS service items as a mirror of equivalent face-to-face service items was informed by advice from the Department of Finance on 7 March 2020 that this approach would facilitate performance monitoring. Although most items were mirrored individually, two submissions to the audit provided feedback that the consolidation of multiple allied health chronic disease management services from individual face-to-face MBS items into a single telehealth and phone item55 negatively affected the ability of stakeholders to monitor and evaluate the usage of these services. One submission asserted that Health had advised this was done for ease of implementation.
Performance monitoring activities
4.7 Health monitored telehealth MBS billing through MBS billing records maintained by Services Australia. A June 2020 live assurance review commissioned by Health found that performance monitoring to that date had been limited to reporting on MBS telehealth item usage.
Figure 4.1: Example of Health internal reporting of billing patterns in Victoria, 13 April 2021

Note: Based on the context in which this figure appeared, a ‘COVID Flag’ of ‘Yes’ refers to telehealth items, a ‘COVID Flag’ of ‘No’ refers to face-to-face items.
Source: Health.
4.8 Recent performance audits by the ANAO have identified weaknesses in Health’s controls to ensure the integrity and quality of third-party data sources used to monitor and report on performance.56 In response to a recommendation in Auditor-General Report No. 3 2022–23 Australia’s COVID-19 Vaccine Rollout that Health establish processes to ensure it regularly obtains assurance over the data quality and IT controls for externally managed systems, Health advised that it will undertake an independent review of its IT controls and application of its internal quality assurance framework, although it did not indicate when this would be done.57 This audit did not test the effectiveness of Health’s system-level controls over the integrity and quality of telehealth billing data.
4.9 The ANAO tested the accuracy of selected departmental reporting on telehealth MBS item usage against billing data that was sourced directly from Services Australia by the ANAO. The analysis found that the reporting was accurate when compared to this data.
Regular reporting on telehealth usage data
4.10 Two data analytics teams in Health were independently tasked with collating MBS telehealth billing data for reporting to senior officials on billing patterns. From 16 March 2020 Health generated and disseminated reporting of billing patterns for temporary telehealth items on at least weekly basis to senior officials and on a monthly basis to the Minister for Health (the Minister).
4.11 The first team was within Medical Benefits Division. Activities comprised:
- from 19 March 2020, an interactive application that allowed users within Medical Benefits Division to generate on-demand reporting on billing data for temporary telehealth items introduced in response to COVID-19;
- between 9 February and 31 March 2021, a weekly update on MBS items provided to the First Assistant Secretary of Medical Benefits Division comparing telehealth and face-to-face service uptake and bulk billing trends;
- between May 2020 and March 2021, monthly reporting on COVID-19 telehealth items (comparing the number of MBS services provided and the benefits paid against the year prior to demonstrate the impact of COVID-19 on different categories of healthcare) at the request of the Minister through the Minister’s office; and
- adaptation of these reports in response to requests from senior Health officials and, over the course of the pandemic, ad hoc reporting at the request of senior Health officials.
Figure 4.2: Example of Medical Benefits Division reporting on billing patterns, 21 March 2021

Source: Health.
4.12 The second team, within Benefits Integrity and Digital Health Division, developed three automated reports that monitored telehealth usage patterns over time, in part to assist in the identification of potential non-compliance (Table 4.1). Production of these reports ceased upon the transition to permanent telehealth.
Table 4.1: Reporting on temporary telehealth items by Benefits Integrity and Digital Health Division
|
Name of report |
Date of reporting |
Number of reports |
Contents |
Recipients |
|
COVID-19 MBS Items Daily Report |
31 March 2020 to 4 September 2020 |
105 |
|
Senior officials from Health Resourcing Group and the departmental COVID-19 Response Taskforce |
|
COVID-19 MBS Items Weekly Report |
17 September 2020 to 16 December 2021 |
63 |
|
Senior officials in Benefits Integrity and Digital Health Division |
|
COVID-19 MBS Items Assurance Report |
58 |
High-level summary of billing behaviours that could indicate potential non-compliance in relation to telehealth items. |
Senior officials in Benefits Integrity and Digital Health Division |
|
Source: ANAO analysis of Health records.
|
Case study 2. Performance monitoring — mandatory isolation in Victoria |
|
On 9 July 2020 the Victorian Government reinstated ‘stay at home’ restrictions across Melbourne. On 20 July 2020 Health reintroduced a requirement that telehealth providers must have a pre-existing clinical relationship with the patient but provided an exemption for patients in COVID-19 impacted areas. The Victorian restrictions were expanded to cover the entire state on 6 August 2020. On 11 August 2020 the COVID-19 MBS Items Daily Report was circulated to senior officials responsible for the expansion of telehealth drawing attention to a ‘key insight’ that telehealth servicing in Victoria had increased by 5.7 per cent over the preceding week and had been rising for the preceding eight weeks. |
4.13 In 2020 and 2021, the two data analytics teams conducted analysis of telehealth MBS data largely to service the specific needs of their respective divisions (policy or compliance respectively). However, the absence of defined roles for separate teams analysing the same dataset caused some confusion between March and June 2020 over how information requirements on the performance of telehealth measures could be best met and how duplication of effort could be avoided.
Receipt of performance information from other sources
4.14 Senior officials responsible for the expansion of telehealth received or identified research conducted by peak bodies and other third parties. This research was based on surveys of providers and patients about their experiences of the early stages of implementation. Health did not maintain a formal process to assess the implications of this research, and the extent to which the reporting was considered by responsible officials is undocumented. A list of third-party reporting received by Health is provided in Appendix 4.
4.15 Health officials advised the ANAO that informal liaison with key stakeholders was another mechanism by which implementation issues were identified. Peak bodies, the Director of the Professional Services Review58, members of the Primary Health Reform Steering Group, medical professionals, and academics contacted Health to raise issues.
4.16 The ANAO identified evidence of implementation issues through complaints and inquiries from members of the public to Services Australia, and provider inquiries to AskMBS. The theme of complaints and inquiries received by Health included:
- perceived lack of clarity or gaps in policy guidance on telehealth use;
- suggestions on health services to be added to telehealth; and
- the distribution of inaccurate information about telehealth by third-parties.
4.17 Health did not use these complaints and inquiries in a systematic way to analyse and monitor performance.
Has the effectiveness of the expansion of telehealth been evaluated?
Health did not develop an evaluation plan for temporary telehealth or for permanent telehealth. Telehealth policy proposals did not address evaluation in detail. Health has not coherently evaluated the effectiveness of telehealth as a pandemic response, although some analysis of billing data and independent research has been undertaken. Health used some reviews and data analysis to inform decision making on permanent telehealth. Health’s plans to evaluate permanent telehealth were not settled as at September 2022.
Planning for evaluation
4.18 Health did not make plans at the time of the initial telehealth expansion in March 2020 to conduct an evaluation of temporary telehealth settings. While this reflected the focus on rapid implementation in the initial response, extensions of temporary telehealth in September 2020 and February 2021 also did not include evaluation plans.
4.19 Advice provided to the Australian Government for the third telehealth extension in May 2021 contained three short statements that proposed future evaluation arrangements.
- A review of temporary telehealth items would be conducted prior to 31 December 2021 to inform the Australian Government.59
- Health would undertake a review of certain new temporary telehealth items (relating to blood borne viruses and sexual and reproductive health) via the Medical Services Advisory Committee60 before 30 June 2023; the review would consider the appropriateness of making these items permanent.
- An ongoing review of telehealth services would be conducted under a proposed ‘MBS Continuous Review’.61
Recommendation no.3
4.20 As a component of a broader review into the COVID-19 pandemic response required under the Australian Health Sector Emergency Response Plan for Novel Coronavirus, the Department of Health and Aged Care considers the lessons learned for future pandemic preparedness from the inclusion of temporary telehealth items as one of several COVID-19 pandemic response measures.a
Department of Health and Aged Care response: Agreed in-principle, noting telehealth has been a significant contributor to the pandemic response, and the parameters and approach for the broader review are yet to be determined by the Government.
4.21 The concerns raised by ANAO in relation to the Department’s implementation approach for MBS amendments in a national emergency context are interpreted as the bases for ANAO recommendations 1 and 2, to which the Department agrees.
4.22 The Department also notes the transition to permanent telehealth items from 1 January 2022 adopted lessons learned from past and COVID-19 telehealth measures. A wide range of permanent telehealth items, as a significant legacy from the pandemic, include specific provisions for improved patient access in response to COVID-19 infection (including additional temporary measures) and emergencies such as natural disasters. These arrangements supersede the bespoke and one-off temporary telehealth items previously implemented in response to specific droughts, floods and bushfires. The Department’s planned post-implementation review of permanent telehealth items (to which Recommendation 4 refers) will consider the clinical appropriateness of the range of these services. Relevant research and evaluations of telehealth by external or independent sources will inform any future telehealth considerations.
Note a: See previous advice from Health regarding a broader review into the COVID-19 pandemic in Auditor-General Report No. 3 2022–23 Australia’s COVID-19 Vaccine Rollout, paragraph 23.
4.23 Advice provided to the Australian Government proposing permanent telehealth arrangements in December 2021 did not discuss arrangements for an evaluation of permanent telehealth and noted the absence of a formal evaluation framework. ‘Ongoing monitoring for fiscal impacts in the context of Budget and [Mid-Year Economic and Fiscal Outlook] processes’ and compliance activity were identified as sources of performance information.
4.24 From May 2020 planning for permanent telehealth was conducted concurrently with extensions of temporary settings. Policy advice for all three extensions noted that a review of telehealth experience during the COVID-19 pandemic would be used to inform policy settings for permanent telehealth. No specific criteria against which the success of temporary telehealth as a pandemic response or as a prototype for permanent telehealth were identified, however the advice articulated specific sources of temporary telehealth evidence that would be used to inform permanent telehealth policy proposals (Table 4.2).
Table 4.2: Evidence sources nominated by Health as a means to capture temporary telehealth experience to inform future policy
|
|
Date of temporary telehealth extension |
||
|
Source of evidence |
Sep 2020 |
Feb 2021 |
May 2021 |
|
MBS data — utilisation of telehealth items |
✔ |
✔ |
✔ |
|
MBS data — analysis of compliance |
✔ |
✔ |
|
|
Independent expert advicea |
✔ |
✔ |
✔ |
|
Tertiary analysisb of patient indicators (outcomes and experience) |
✔ |
✔ |
|
|
Consultation with stakeholders (not further defined) |
✔ |
✔ |
|
|
Consultation with industry |
|
|
✔ |
|
Consultation with consumers |
|
|
✔ |
Note a: The appointment of expert advisors in the Primary Health Reform Steering Group is discussed in footnote 29.
Note b: Tertiary analysis refers to interpretative analysis of empirical studies of patient outcomes and experiences.
Source: ANAO analysis based on Health records.
Use of evidence to inform permanent telehealth policy
4.25 Nine of the 31 submissions to the audit (29 per cent) provided feedback on a perceived lack of evaluation by the department or insufficient evidence to support the policy decisions for permanent telehealth. The ANAO examined whether the sources of evidence cited in policy advice (MBS data analysis, independent expert advice and tertiary analysis, see Table 4.2) were used in practice to inform policy development for permanent telehealth. Stakeholder consultation undertaken on permanent telehealth is discussed in paragraphs 2.30 to 2.36.
Analysis of MBS data
4.26 In 2020 and 2021 Health periodically collated insights drawn from MBS billing data about how telehealth was being used during the pandemic and briefed decision makers on how this analysis should inform the design of permanent telehealth. Analyses conducted by Health considered the volume and cost of services billed; comparisons between telehealth and equivalent face-to-face items; the use of videoconferencing compared to phone only items; the impact of telehealth on access to health care in rural and regional areas; and the prevalence of bulk billing. Analysis of MBS data was featured in six of seven ‘deep dive’ briefs provided to the Minister between 2 June 2020 and 6 August 2021 to discuss potential policy settings for permanent telehealth.62
Independent expert advice and tertiary analysis
4.27 During 2020 and 2021 Health commissioned primary and tertiary research from independent experts to contribute to an evidence base for permanent telehealth. The research focussed on the benefits and clinical suitability of telehealth services. Two of the three research projects either collected evidence from consumers who had experience with telehealth during the pandemic, or considered academic studies that had been conducted in relation to telehealth in Australia during the pandemic. The remaining project largely examined research conducted prior to the pandemic. None of the projects evaluated the administrative aspects of the expansion of telehealth services during COVID-19.
4.28 The Australian Institute for Health and Welfare (AIHW)63 released seven reports relevant to telehealth across 2020 and 2021. The ANAO observed one instance of senior Health officials using AIHW reporting in April 2021 to inform decision making around telehealth.
Future evaluation of permanent telehealth
4.29 On 12 April 2021 a Medical Research Future Fund grant was awarded to the Australian National University to conduct research between 1 May 2021 to 30 April 2024 on the effect of telehealth on the uptake and quality of primary health care.64 Two senior Health officials are members of the steering committee for this research project. The research plans to consider the impact of telehealth on primary health care uptake and quality (including safety, accessibility, continuity and acceptability), and the management of safety in telehealth consultations.
4.30 The terms of reference for the MBS Review Advisory Committee are confined to examining the effectiveness of health services on the MBS and do not include consideration of whether the administrative experience of implementing MBS changes such as the expansion of telehealth holds lessons for the administration of the Medicare program.65 Health undertook preliminary work in August 2022 to prepare tasking for the MBS Review Advisory Committee to conduct an evaluation of telehealth under the auspices of the MBS Continuous Review.
Recommendation no.4
4.31 The Department of Health and Aged Care finalise its plans to evaluate permanent telehealth.
Department of Health and Aged Care response: Agreed.
4.32 The Minister for Health and Aged Care, the Hon Mark Butler MP, has already requested the MBS Review Advisory Committee (MRAC) to undertake this work, which will be complemented by an independent updated review of recently published research to inform sector wide understanding of telehealth and the regular analysis and publishing of data on usage.
Appendices
Appendix 1 Entity response
Appendix 2 Improvements observed by the ANAO
1. The existence of independent external audit, and the accompanying potential for scrutiny improves performance. Improvements in administrative and management practices usually occur: in anticipation of ANAO audit activity; during an audit engagement; as interim findings are made; and/or after the audit has been completed and formal findings are communicated.
2. The Joint Committee of Public Accounts and Audit (JCPAA) has encouraged the ANAO to consider ways in which the ANAO could capture and describe some of these impacts. The ANAO’s 2021–22 Corporate Plan states that the ANAO’s annual performance statements will provide a narrative that will consider, amongst other matters, analysis of key improvements made by entities during a performance audit process based on information included in tabled performance audit reports.
3. Performance audits involve close engagement between the ANAO and the audited entity as well as other stakeholders involved in the program or activity being audited. Throughout the audit engagement, the ANAO outlines to the entity the preliminary audit findings, conclusions and potential audit recommendations. This ensures that final recommendations are appropriately targeted and encourages entities to take early remedial action on any identified matters during the course of an audit. Remedial actions entities may take during the audit include:
- strengthening governance arrangements;
- introducing or revising policies, strategies, guidelines or administrative processes; and
- initiating reviews or investigations.
4. In this context, the below actions were observed by the ANAO during the course of the audit. It is not clear whether these actions and/or the timing of these actions were planned in response to proposed or actual audit activity. The ANAO has not sought to obtain assurance over the source of these actions or whether they have been appropriately implemented.
- Following information requests from ANAO for copies of approved External Costing Request (ECR) forms, additional ECR forms that had not been placed on file in Health’s records management system were added to the file.
Appendix 3 Weekly queries received and timeliness of responses through Health’s AskMBS email advice service
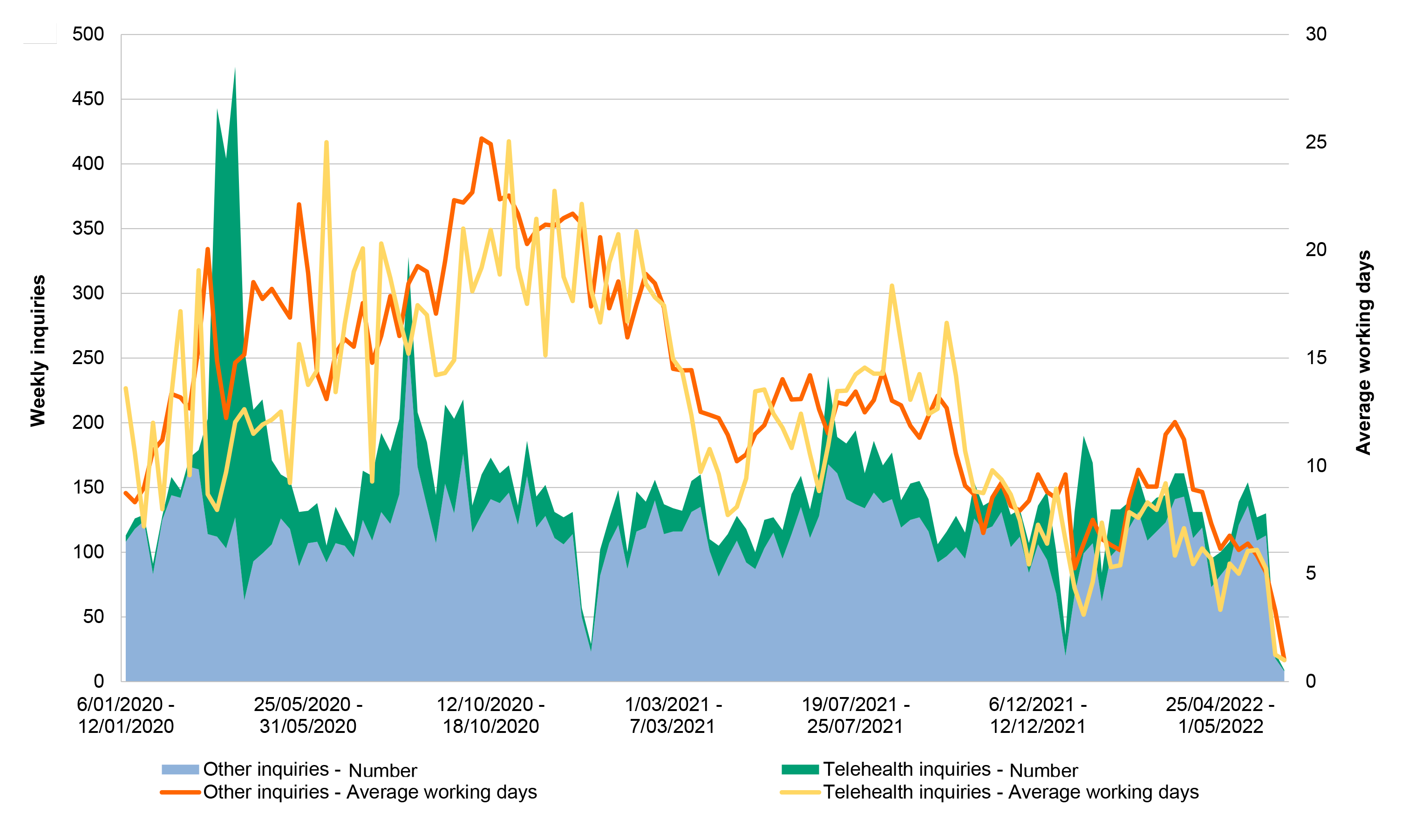
Source: ANAO analysis of data provided by Health on AskMBS inquiries.
Appendix 4 Third-party research on temporary telehealth received by Department of Health and Aged Care
|
Report owner |
Date of survey |
Date report received by Health |
Survey sample |
Survey content |
|
Medical Director |
March 2020 |
20 March 2020 |
30 medical practices |
Practice intentions and responses to first week of COVID-19 telehealth |
|
Consumer Health Forum |
March-April 2020 |
5 June 2020 |
95 health consumers |
Patient sentiment about telehealth |
|
Medical Republic |
May 2020 |
17 June 2020 |
174 general practitioners and general practice owners |
Reported changes to revenue and opinions on causes |
|
Effect of telehealth on revenue |
||||
|
Australian Psychological Society |
Unknown |
30 June 2020 |
255 public sector psychologists and 1343 psychologists working in private practice |
Reported utilisation of telehealth |
|
Provider sentiment about telehealth |
||||
|
Perceived barriers and facilitators to face-to-face and telehealth services during COVID-19 |
||||
|
Global Centre for Modern Aging |
May 2020 |
1 July 2020 |
1242 Australian adults |
Perceived quality of care provided via telehealth |
|
Royal Australian and New Zealand College of Psychiatrists |
July 2020 |
11 September 2020 |
1079 psychiatrists |
Reported utilisation of telehealth |
|
Provider sentiment about telehealth |
||||
|
Perceived advantages for patients |
||||
|
Perceived barriers and facilitators to telehealth |
||||
|
Royal Australasian College of Physicians |
May 2020 |
14 October 2020 |
950 specialists |
Reported utilisation of telehealth |
|
Provider sentiment about telehealth |
||||
|
Provider suggestions on how to measures clinical outcomes for telehealth |
||||
|
Perceived barriers to telehealth |
||||
|
Provider opinions on future of telehealth |
||||
|
Royal Australasian College of Surgeons |
August 2020 |
30 October 2020 |
698 surgeons and 1125 patients of surgeons surveyed |
Reported utilisation of telehealth |
|
Provider sentiment about telehealth |
||||
|
Perceived barriers and facilitators to telehealth |
||||
|
Perceived quality of care provided via telehealth |
||||
|
CommBank |
June-July 2020 |
9 November 2020 |
201 key decision makers at general practices and 1032 patients of general practice |
Reported utilisation rates |
|
Patient sentiment about telehealth |
||||
|
Provider sentiment about telehealth |
||||
|
Reported GP practice business priorities |
||||
|
Royal Australian College of General Practitioners |
May 2020 |
11 May 2021 |
1782 general practitioners |
Reported utilisation |
|
Provider sentiment about telehealth |
||||
|
Provider opinions on future of telehealth |
||||
Source: ANAO analysis of Health records.
Footnotes
1 The Medicare schedule fee is the amount payable by the patient that the government considers appropriate for one of these services.
2 The Medicare benefit is calculated as a percentage of the schedule fee and depends on the circumstances of the service. Patients can claim 100 per cent of the schedule fee as a rebate for general practice services and 85 per cent of the schedule fee as a rebate for non-general practice services provided out of hospital. A provider may choose to ‘bulk bill’ a service, in which case the rebate is assigned by the patient to be paid directly by the government to the provider on the condition that the patient pays no further amount for that service to the provider.
For further background, see Australian Parliamentary Library, Medicare: a quick guide [Internet], 12 July 2016, available from https://www.aph.gov.au/About_Parliament/Parliamentary_Departments/Parliamentary_Library/pubs/rp/rp1 617/Quick_Guides/Medicare [accessed 8 September 2022].
3 In this report ‘provider’ refers to general practitioners, specialists, allied health professionals, and other health professionals eligible to provide Medicare services.
4 In this report, references to the Minister refer to the Hon Greg Hunt MP unless otherwise stated.
5 An Aboriginal medical service provider is a provider funded principally to provide services to Aboriginal and Torres Strait Islander patients, and is similar to an Aboriginal Community Controlled Health Organisation, which is a provider governed by an Aboriginal body that is elected by the local Aboriginal community.
6 An example of a ‘patient-end’ service is where a general practitioner assists the patient to access a videoconference with a specialist, from the GP’s consulting room.
7 These were defined as Modified Monash Areas 3 to 7 in New South Wales, Queensland or Victoria.
A factsheet explaining the Modified Monash Model geographical classification scheme can be found at Department of Health and Aged Care, Modified Monash Model – fact sheet [Internet], available from https://www.health.gov.au/resources/publications/modified-monash-model-fact-sheet [accessed 8 September 2022].
8 The Australian Health Protection Principal Committee is the key decision-making committee for health emergencies. It is comprised of all state and territory Chief Health Officers and is chaired by the Australian Chief Medical Officer.
For further background, see Department of Health and Aged Care, Australian Health Protection Principal Committee (AHPPC) [Internet], available at https://www.health.gov.au/committees-and-groups/australian-health-protection-principal-committee-ahppc [accessed 6 September 2022].
9 People aged over 70 years, people with chronic diseases, Aboriginal and Torres Strait Islander people aged over 50, people who were immunocompromised, pregnant people and new parents with babies.
10 See paragraph 2.48 for an explanation of 3C determinations.
11 On 13 March 2020, the definition of ‘health professional at risk of COVID-19 virus’ only applied to providers who were COVID-19 positive or required to self-isolate. On 23 March 2020, the definition was expanded to include providers aged 70 years or older, or aged 50 years or older and Indigenous; pregnant; a parent of a child aged under 12 months; or immune compromised.
12 Biosecurity (Human Biosecurity Emergency) (Human Coronavirus with Pandemic Potential) Declaration 2020. The emergency declaration was in force until 17 April 2022.
13 A list of Australian Government announcements around this period can be found at Parliamentary Library, COVID-19: a chronology of Australian Government announcements (up until 30 June 2020) [Internet], 23 June 2021, available at https://www.aph.gov.au/ [accessed 12 August 2022].
14 Items added later for group therapy and similar services were exempted from this requirement.
15 There were exemptions for young infants, patients experiencing homelessness, patients in COVID-19 impacted areas, patients receiving urgent after-hours service, and patients of Aboriginal Community Controlled Health Services.
16 Voluntary patient registration is a system whereby patients register with their usual general practice and nominate their usual doctor, with a view to improving continuity of care and better long-term outcomes for that patient. The consultation draft of the Primary Health Care 10 Year Plan proposed that telehealth services be restricted to voluntarily registered patients.
17 Further details on the ANAO’s COVID-19 multi-year audit strategy is available from Australian National Audit Office, ANAO COVID-19 multi-year audit strategy [Internet], https://www.anao.gov.au/work-program/covid-19 [accessed 14 September 2022].
18 Australian Government, Policy Hub, Introduction to delivering great policy [Internet], available from https://www.policyhub.gov.au/model [accessed 2 June 2022].
19 P Shergold, Learning from Failure: Why large government policy initiatives have gone so badly wrong in the past and how the chances of success in the future can be improved [Internet], Commonwealth of Australia, 2015, available at https://www.apsc.gov.au/publication/learning-from-failure [accessed 16 August 2022].
20 See paragraph 2.48.
21 Department of Finance, Resource Management Guide 107: Risk Potential Assessment Tool [Internet], 9 November 2020, available from https://www.finance.gov.au/publications/resource-management-guides/risk-potential-assessment-tool-general-guidance-rmg-107 [accessed 14 July 2022].
22 Prime Minister and Cabinet, Australian Government Guide to Regulatory Impact Analysis [Internet], March 2020, available from https://obpr.pmc.gov.au/sites/default/files/2021-06/australian-government-guide-to-regulatory-impact-analysis.pdf [accessed 8 September 2022].
23 On 18 November 2022 the Office of Best Practice Regulation was renamed to the Office of Impact Analysis.
24 For further details of the exemption, see Office of Best Practice Regulation, Prime Minister’s Exemption – COVID-19 related measures [Internet], 31 March 2020, available from https://obpr.pmc.gov.au/published-impact-analyses-and-reports/prime-ministers-exemption-covid-19-related-measures [accessed 14 July 2022].
25 The Office of Best Practice Regulation advised the ANAO that it assessed the third telehealth extension as having ‘no more than minor impacts’, requiring a minor RIS or a related draft RIS be used to inform government decision on the extension.
26 The Office of Best Practice Regulation assesses RISs according to four assessment tiers: insufficient, adequate, good practice, and exemplary practice.
27 See paragraph 2.14 for a description of the process followed to evaluate the suggestions.
28 See paragraph 1.20.
29 On 18 October 2019 the Minister announced the appointment of expert advisors to the Primary Health Reform Steering Group to guide the creation of the 10 Year Plan.
For more information, see Department of Health and Aged Care, Primary Health Reform Steering Group Established [Internet], 18 October 2019, https://www.health.gov.au/ministers/the-hon-greg-hunt-mp/media/primary-health-reform-steering-group-established [accessed 8 September 2022].
Health advised the ANAO that the reason for the separate consultation processes was that consultation on GP and allied provider telehealth was within the scope of the terms of reference for the Primary Health Reform Steering Group while specialist telehealth was not.
30 The Consultation Hub seeks information and invites submissions from members of the public and specific stakeholder groups on a range of consultations.
31 The National Health Reform Agreement 2020–2025 is an agreement between the Australian Government and all state and territory governments. Through the agreement, the Australian Government contributes funds to the states and territories for public hospital services.
For further background, see Australian Government, The National Health Reform Agreement, [Internet], available from https://federalfinancialrelations.gov.au/agreements/national-health-reform-agreement [accessed 12 October 2022].
32 NACCHO is a national peak body representing 144 Aboriginal Community Controlled Health Organisations.
33 Between 2015 and 2020, the MBS Review Taskforce reviewed over 5700 items on the MBS and provided 1400 recommendations to the Australian Government regarding potential changes to the MBS.
For further information, see Department of Health and Aged Care, Medicare Benefits Schedule (MBS) Review Taskforce [Internet], available from https://www.health.gov.au/committees-and-groups/mbs-review-taskforce [accessed 22 August 2022].
34 The report can be accessed at Department of Health and Aged Care, Medicare Benefits Schedule Review Taskforce: Report from the Telehealth Working Group [Internet], June 2020, available from https://www.health.gov.au/sites/default/files/documents/2021/06/final-report-from-the-telehealth-working-group.pdf [accessed 8 September 2022].
35 The Medical Services Advisory Committee is an independent non-statutory advisory committee that provides advice to the Australian Government on whether a new medical service should be publicly funded by assessing its comparative safety, clinical effectiveness, cost-effectiveness and total cost.
For further background, see Department of Health and Aged Care, Medical Services Advisory Committee [Internet], available from http://www.msac.gov.au/ [accessed 22 August 2022].
36 The Institute for Evidence-Based Healthcare at Bond University was headed by a former MBS Review Taskforce member with previous MSAC experience.
37 In accordance with the Health Insurance Act 1973 and Health Insurance (Professional Services Review Scheme) Regulations 2019, a provider who provides 80 professional attendance services per day on 20 or more days in a 12-month period must be referred to the Director of Professional Services Review to consider whether the provider was engaged in inappropriate practice. The Professional Services Review is a statutory agency within the Health portfolio responsible for reviewing and examining possible inappropriate practice by providers.
38 Similar to the 80/20 rule, the 30/20 rule applies to 30 telehealth attendances by phone per day on 20 or more days in a 12-month period.
39 Advice was provided at the same time to the Australian Government regarding plans for ongoing performance monitoring and evaluation of MyGP. The advice noted that MyGP arrangements could help ensure the safety and quality of GP telehealth services, and that rates of telehealth claiming under MyGP would be a performance measure for MyGP.
40 The 80/20 and 30/20 rules were reintroduced for telehealth items on 1 July 2022 and 1 October 2022, respectively.
41 Sections 15 to 18 of the Public Governance, Performance and Accountability Act 2013 impose general duties on the accountable authority of a Commonwealth entity to establish and maintain an appropriate system of internal control and an appropriate system of risk oversight and management for the entity; to encourage officials to collaborate with others to achieve common objectives; to take into account the risks and effects of imposing requirements for the management of public resources on others; and to promote the proper use of public resources.
42 Prior to August 2020, the Benefits Integrity and Digital Health Division was called the Provider Benefits and Integrity Division and the Health Resourcing Group was called the Health Financing Group. In this report the current names of business areas are used throughout to avoid confusion.
43 Health’s project management framework is a resource that provides Senior Responsible Officers, project managers and project teams with guidance on the project management practices and procedures that should be applied to deliver a project.
44 If a Senior Responsible Officer determines that an ‘item’ in ‘Health Tracker – Planner’ should be managed as a project in accordance with the project management framework, a concurrent ‘Health Tracker – Implementation’ record is created and maintained.
45 The 2021–22 divisional plan for Benefits Integrity and Digital Health Division identified ‘adapting, innovating and responding to new and emerging compliance risks such as telehealth, vaccines, hospital compliance, MBS changes and other emerging issues’ under a heading entitled ‘Challenges’. The plan did not evaluate how this challenge might affect divisional objectives or how these impacts would be managed by the division.
46 Services Australia maintains similar agreements with other agencies for whom it delivers services and payments.
For further background, see Auditor-General Report No. 30 2019–20 Bilateral Agreement Arrangements Between Services Australia and Other Entities.
47 Informal liaison was also used to communicate likely implementation issues for Services Australia to Health. Following informal liaison between Health and Services Australia, on 26 March 2020 Services Australia advised Health that the proposed relaxation of mandatory bulk billing could not feasibly be implemented in billing systems by the planned implementation date of 30 March 2020. Health advised the Minister through his office and the implementation date for this change was delayed by one week to 6 April 2020.
48 Since 1 July 2018, section 12 of the Australian Government Agencies Privacy Code has required entities to conduct a PIA for all high risk projects. A project will be high risk if it involves any new or changed ways of handling personal information that is likely to have a significant impact on the privacy of individuals.
For further background, see Office of the Australian Information Commissioner, Australian Government Agencies Privacy Code [Internet], OAIC, available from https://www.oaic.gov.au/privacy/privacy-for-government-agencies/australian-government-agencies-privacy-code [accessed 14 September 2022].
49 Between 2019–20 and 2020–21, Health’s Portfolio Budget Statements stated that a measure of performance for the health provider compliance program included the prevention of non-compliance where possible.
50 As noted in paragraph 3.23, Health’s risk tolerance is permissive for policy and delivery risks, and restrictive for financial and regulatory risks.
51 For further background, see paragraph 2.10 of Auditor-General Report No. 17 of 2020–21 Managing Health Provider Compliance.
52 Australian Medical Association, Australian Association of Practice Managers, Royal Australian College of General Practitioners, Rural Doctors Association of Australia and Australian College of Rural and Regional Medicine.
53 The spreadsheet additionally listed 42 tip-offs where the provider in question was already subject to treatment and a decision was taken to add a file note about the telehealth allegation to the case file rather than initiating new treatment.
54 Examples included whether telehealth consultations are being billed for clinically appropriate services, or whether exemptions aimed at improving access for patients in COVID hotspots or mandatory isolation are being correctly applied. Health’s provider compliance framework and activities to monitor and treat integrity risks are discussed in paragraphs 3.54 to 3.59.
55 Item numbers 93000 and 93013, respectively.
56 Paragraphs 3.23 to 3.31 of Auditor-General Report No. 3 2022–23 Australia’s COVID-19 Vaccine Rollout; paragraphs 3.3 to 3.11 of Auditor-General Report No. 5 2021–22 Improving Immunisation Coverage; paragraphs 4.8 to 4.9 of Auditor-General Report No. 22 2020–21 Planning and Governance of COVID-19 Procurements to Increase the National Medical Stockpile.
57 Paragraph 3.26 of Auditor-General Report No. 3 2022–23 Australia’s COVID-19 Vaccine Rollout.
58 See footnote 37 for an explanation of the Professional Services Review.
59 Policy advice provided to the Australian Government in December 2021 included consideration of MBS billing patterns for telehealth in 2021.
60 Further information on the Medical Services Advisory Committee is provided in paragraph 2.43.
61 The MBS Continuous Review, led by the MBS Review Advisory Committee, was established in September 2021 to review MBS items and services in a similar manner to the (by then concluded) MBS Review Taskforce.
For further background, see Department of Health and Aged Care, Medicare Benefits Schedule (MBS) Continuous Review [Internet], available from https://www.health.gov.au/initiatives-and-programs/medicare-benefits-schedule-mbs-continuous-review [accessed 9 September 2022].
62 See paragraph 2.22.
63 The Australian Institute of Health and Welfare is an independent statutory Australian Government agency within the Health portfolio that produces information and statistics to inform policy and service delivery decisions with the aim of improving health and welfare for Australians.
For further information, see Australian Institute of Health and Welfare, Our role & strategic goals [Internet], AIHW, available at https://www.aihw.gov.au/about-us/what-we-do [accessed 9 September 2022].
64 Details of the grant can be viewed at GrantConnect, Grant Award View – GA168275 [Internet], Department of Finance, available from https://www.grants.gov.au/Ga/Show/5b2566ef-5d0f-4425-804b-86c678745069 [accessed 1 September 2022].
65 Department of Health and Aged Care, Medicare Benefits Schedule Review Advisory Committee – Terms of reference, [Internet], available from https://www.health.gov.au/resources/publications/medicare-benefits-schedule-review-advisory-committee-terms-of-reference [accessed 14 September 2022].