Browse our range of reports and publications including performance and financial statement audit reports, assurance review reports, information reports and annual reports.
Design and Early Implementation of Residential Aged Care Reforms

Please direct enquiries through our contact page.
Audit snapshot
Why did we do this audit?
- In 2022–23, 250,273 older Australians received permanent residential aged care. The Royal Commission into Aged Care Quality and Safety recommended introducing mandatory minimum staffing standards for registered nurses (RNs) and other aged care workers (Recommendation 86). The Australian Government agreed to the recommendation.
- This audit provides early assurance to the Australian Parliament over whether the Department of Health and Aged Care (the department) and the Aged Care Quality and Safety Commission (ACQSC) have effectively introduced the mandatory staffing standards.
Key facts
- From 1 July 2023 the government required residential facilities to have an RN on site and on duty 24 hours a day (24/7 RN).
- From 1 October 2023 the government required each aged care resident to receive, on average, at least 200 minutes of care per day, including at least 40 minutes of RN care (mandatory care minutes).
What did we find?
- The design and early implementation of 24/7 RN and mandatory care minutes was largely effective.
- The department provided policy advice on Recommendation 86 reforms that was largely robust.
- The department was largely effective at introducing the new workforce requirements.
- The department and ACQSC were largely prepared to monitor and enforce compliance with 24/7 RN and mandatory care minutes.
What did we recommend?
- The ANAO made two recommendations to the department relating to assessing the risk of new policy proposals and program evaluation.
- The ANAO made two recommendations to ACQSC relating to documentation of procedures and monitoring regulatory impact.
- The department and ACQSC agreed to all recommendations.
88%
Residential aged care facilities reporting an RN on site and on duty 24/7 in September 2023, compared to departmental estimates ranging from 46% to 80% in 2020 to 2022 and a target of 100%.
194 minutes
Care provided per resident per day in April to June 2023, compared to estimates prepared for the Royal Commission of 180 in 2018–19 and a nominal sector target of 200.
37 minutes
RN care provided per resident per day in April to June 2023, compared to estimates prepared for the Royal Commission of 36 in 2018–19 and a nominal sector target of 40.
Summary and recommendations
Background
1. Residential aged care refers to accommodation and services that are provided to older Australians whose physical, mental or social functioning is affected to such a degree that the person cannot maintain themself independently. Residential aged care is subsidised by the Australian Government with payments made directly to approved providers who must meet specified standards of care regulated by the Aged Care Quality and Safety Commission (ACQSC). The Australian Government Department of Health and Aged Care (the department) is responsible for delivering residential aged care programs that contribute to improved wellbeing for older Australians.
2. In March 2021 the Royal Commission into Aged Care Quality and Safety recommended the Australian Government introduce mandatory minimum staffing standards to improve the quality and safety of residential aged care (Recommendation 86). The Royal Commission recommended that a minimum standard be set for the amount of time an average resident would receive direct care (care minutes) each day, and that a registered nurse (RN) be onsite and on duty for a prescribed number of hours each day.
3. In May 2021 the Australian Government accepted Recommendation 86 and provided $3.9 billion over four years to support the introduction of care minutes. The funding initially supported residential aged care services to voluntarily achieve 200 minutes of care per resident per day, including 40 minutes of RN care (200/40 care minutes) and have an RN on site and on duty 16 hours a day, every day (16/7 RN). Minimum care minutes and 16/7 RN would be mandated from 1 October 2023. In July 2022 the Australian Government’s policy was to implement 200/40 care minutes on the previously specified timeframe and to introduce a requirement for an RN to be on-site at all times (24/7 RN) by 1 July 2023, 12 months earlier than the Royal Commission recommendation. The Australian Government committed an additional $2.5 billion over four years to support the introduction of 24/7 RN and an increased standard for care minutes (215/44 care minutes) from 1 October 2024.
Rationale for undertaking the audit
4. Each year approximately 250,000 older Australians receive residential aged care on a permanent basis. The 2021 report of the Royal Commission into Aged Care Quality and Safety made 148 recommendations, including that RN and overall care minutes provided to each resident be increased (Recommendation 86).
5. The Australian Government has identified that aged care providers face challenges in attracting sufficient RNs and other aged care staff, particularly in rural and remote settings. This audit provides early assurance to the Australian Parliament over whether the Department of Health and Aged Care and the Aged Care Quality and Safety Commission have effectively supported the design and early implementation of Recommendation 86.
Audit objective and criteria
6. The objective of the audit was to assess whether the design and early implementation of the Australian Government’s response to Recommendation 86 of the Royal Commission into Aged Care Quality and Safety has been effective.
7. To form a conclusion against the objective, the ANAO adopted the following high-level criteria.
- Did the Department of Health and Aged Care provide robust policy advice on residential aged care workforce reforms?
- Has the Department of Health and Aged Care effectively introduced the new workforce requirements?
- Is the regulatory system prepared for the new requirements?
Conclusion
8. The design and early implementation of the Australian Government’s response to Recommendation 86 of the Royal Commission into Aged Care Quality and Safety was largely effective.
9. The department provided largely robust policy advice on residential aged care reforms in response to Recommendation 86. Advice was informed by workforce data and modelling, and conveyed some costs, benefits and risks of the proposed policies. However, established Australian Government mechanisms for analysing the costs, benefits and risks of policy options were not fully utilised. There was a lack of structured risk analysis as required under Australian Government policy. Evaluation planning was not properly addressed in policy proposals.
10. The department’s introduction of the new workforce requirements was largely effective. As at October 2023 the department’s implementation of the requirements through operational arrangements, legislation and IT systems was largely consistent with the government’s policy intent. The 24/7 RN exemption process was consistent with government requirements but delayed. Project management and governance arrangements for the new workforce measures were largely fit for purpose.
11. The department and ACQSC were largely prepared to monitor and enforce compliance with 24/7 RN and mandatory care minutes. Both entities defined their respective roles and responsibilities, consulted with stakeholders, and received funding for regulatory activities. After initial delays, both entities finalised operational plans for regulatory activities. Both entities had commenced but not completed updating procedural guidance and training staff as at October 2023. The department has performance measures in place but there is no evaluation plan. ACQSC has not planned how it will measure regulatory impact.
Supporting findings
Policy advice
12. Between March 2021 and March 2023, the department presented policy options to the Australian Government to respond to Recommendation 86. The department relied on a process to certify that a Regulatory Impact Statement did not need to be prepared for Recommendation 86 policy options, with the result that some analysis normally addressed in a Regulatory Impact Statement was not provided. (See paragraphs 2.2 to 2.11)
13. The department’s policy advice between March 2021 and March 2023 identified some risks associated with responding to Recommendation 86, such as workforce shortages, provider viability and unintended consequences of the new measures such as care shifting. The advice proposed mitigation strategies for these risks. However, there was no structured risk analysis, including through a Risk Potential Assessment Tool, which is required under Australian budget policy. (See paragraphs 2.12 to 2.19)
14. The department used workforce modelling and data to support its policy advice. It used this evidence to project how many additional workers would be required to implement mandatory care minutes and 24/7 RN, and to estimate how workforce supply would be improved through other Australian Government initiatives. Different RN workforce gap estimates were produced, depending on which data source was used. Although some of the data that informed the modelling had methodological limitations that were considered to over-state estimates of workforce supply, these limitations were acknowledged by the department and attempts were made over time to improve the data. The department considered the views of stakeholders in developing its policy advice. (See paragraphs 2.20 to 2.34)
15. The department’s policy advice contained high-level implementation plans. Although some high-level consideration of evaluation was completed as part of a supplementary Regulatory Impact Statement, and elements of an evaluation approach (such as consideration of intended outcomes and data sources) were mentioned in policy advice, there was no defined evaluation plan as at October 2023. (See paragraphs 2.35 to 2.44)
Introducing the new workforce requirements
16. The design of operational policy, legislation and IT systems for 24/7 RN and 200/40 care minutes largely conforms to the Australian Government’s policy decisions. Minor non-conformances comprise: some non-mainstream aged care services being subject to the 24/7 RN requirement without policy authority; IT systems not being updated to accommodate co-located or split services, requiring manual workarounds for a small percentage of facilities in relation to the 24/7 RN requirement; the threshold for payment of the 24/7 RN supplement being lower than that agreed by government; reporting of 24/7 RN compliance not being integrated into facilities’ star ratings; some mandatory care minute targets being lower than the Royal Commission recommended level and other inaccuracies in the calculation of care minute targets; mandatory care minute reporting not being provided at the facility level; and a slight delay in the deployment of IT systems to support public transparency. (See paragraphs 3.2 to 3.25)
17. The department established an administrative process for 24/7 RN exemptions which met legislative requirements. To determine whether to grant an exemption, the department and ACQSC assessed clinical risk and alternative care arrangements. The assessment process that was followed experienced delays in decision-making. No exemption applications were approved prior to 1 July 2023, when the 24/7 RN requirement became mandatory. Exemptions were granted over subsequent months. (See paragraphs 3.26 to 3.36)
18. The department’s project management of 24/7 RN and mandatory care minutes was consistent with the department’s project management framework, except that implementation plans were finalised five to seven months after project work had commenced. There are fit for purpose governance arrangements for coordination of the 24/7 RN and care minutes projects with other aged care reforms. (See paragraphs 3.37 to 3.46)
Preparing to regulate
19. The department and ACQSC’s respective roles and responsibilities for regulating compliance with 24/7 RN and care minutes have been clearly defined and communicated to stakeholders. The department was funded for a compliance role that exceeds its current statutory powers under the Aged Care Act 1997. The department is developing new legislation and an updated memorandum of understanding with ACQSC. (See paragraphs 4.3 to 4.9)
20. The department and ACQSC communicated with aged care providers using consultative forums, websites, webinars and newsletters. There were some targeted communications to providers at higher risk of non-compliance with the 24/7 RN requirement. There was limited engagement with consumer peak bodies through consultative forums. Engagement with state and territory regulators on mandatory care minutes and 24/7 RN proceeded in line with the lower priority that state and territory regulators placed on these measures compared to other aged care reforms. (See paragraphs 4.10 to 4.17)
21. The department and ACQSC have updated systems to incorporate care minute and 24/7 RN data into regulatory intelligence production. There are plans to increase analytic capability for risk profiling of providers in relation to mandatory care minute and 24/7 RN non-compliance. ACQSC’s processes for producing and disseminating regulatory intelligence analysis were insufficiently documented. (See paragraphs 4.18 to 4.26)
22. The entities received additional funding to resource regulatory activities. The department and ACQSC’s compliance plans for mandatory care minutes and 24/7 RN were not finalised by 1 July 2023, the date on which both entities had planned to be ready to conduct regulatory activities. ACQSC commenced regulatory activity on 4 July 2023 and finalised its regulatory approach on 22 July 2023. The absence of legal authority for aspects of the department’s contemplated audit function impeded development of the department’s operational plans. The department finalised its plan on 27 September 2023. (See paragraphs 4.27 to 4.33)
23. Guidance materials and standard operating procedures for monitoring and enforcing compliance with the new requirements were being developed but were largely not finalised as at 1 July 2023. Both entities had finalised certain guidance materials and had delivered some training by September 2023. (See paragraphs 4.34 to 4.39)
24. The department has an external performance measure for care minutes and 24/7 RN, which it monitors. The department does not have an overarching evaluation strategy to examine the impact on residential aged care quality. ACQSC’s regulatory approach acknowledges the need to measure regulatory impact, however as at October 2023, it had no detailed plans to do so. (See paragraphs 4.40 to 4.54)
Recommendations
25. This report makes two recommendations to the department and two recommendations to ACQSC.
Recommendation no. 1
Paragraph 2.14
The Department of Health and Aged Care ensure that Risk Potential Assessment Tools are completed in accordance with Australian Government policy, in particular the requirement to complete a Risk Potential Assessment Tool for new policy proposals with a financial impact of $30 million, and the requirement to revise a Risk Potential Assessment Tool for approved policy proposals when there is a significant change to one or more risk factors affecting implementation. The Department of Health and Aged Care should promote the use of the Risk Potential Assessment Tool for new policy proposals of less than $30 million.
Department of Health and Aged Care response: Agreed.
Recommendation no. 2
Paragraph 2.43
The Department of Health and Aged Care establish evaluation plans for mandatory care minutes and 24/7 RN in order to settle on the policy objectives to be assessed, potential data sources, baseline data, data collection mechanisms and specific timeframes. Gaps in information required for an effective evaluation should be identified and rectified as part of implementation.
Department of Health and Aged Care response: Agreed.
Recommendation no. 3
Paragraph 4.23
The Aged Care Quality and Safety Commission improve its documentation of processes for preparing and disseminating intelligence briefs.
Aged Care Quality and Safety Commission response: Agreed.
Recommendation no. 4
Paragraph 4.53
The Aged Care Quality and Safety Commission identify a method to assess the impact of care minute and 24/7 RN regulation on aged care quality outcomes and whether regulatory activities are effective at promoting compliance with these measures.
Aged Care Quality and Safety Commission response: Agreed.
Summary of entity response
26. The proposed audit report was provided to the department and ACQSC. An extract of the proposed report was provided to the Department of the Prime Minister and Cabinet. The department’s and ACQSC’s summary responses to the report are provided below and their full responses are at Appendix 1.
Department of Health and Aged Care
The Department of Health and Aged Care (department) welcomes the findings in the report and accepts the two recommendations directed to the department.
It was pleasing to note that the design and early implementation of the Australian Government’s response to Recommendation 86 of the Royal Commission into Aged Care Quality and Safety has been found to be largely effective, and that the department was largely effective at introducing the new workforce requirements.
The department acknowledges that, while a comprehensive risk register was maintained through the implementation of the new workforce requirements, a structured risk assessment was not completed for the mandatory care minutes or 24/7 RN policy proposals when they were considered as part of the budget process. The department requires the Risk Potential Assessment Tools to be completed for all new policy proposals and has enhanced its training and guidance to ensure compliance with this policy.
The department is committed to the effective implementation of residential aged care reforms and is taking steps to ensure that evaluation planning is embedded at the outset for the next stage of reforms, such as the new support at home model scheduled to commence from July 2024. In addition, an evaluation plan will be developed for the care minutes and 24/7 RN responsibilities.
Aged Care Quality and Safety Commission
The Aged Care and Quality Safety Commission (the Commission) welcomes the findings which align with its work program. It agrees with each of the two recommendations directed at it: to improve its documentation of processes for preparing and disseminating intelligence briefs, and; to identify a method to assess the impact of Care Minutes (CM) and 24/7 Registered Nursing (RN) regulation on aged care quality outcomes and whether regulatory activities are effective at promoting compliance with these measures.
The Commission has finalised the Standard Operating Procedure (SOP) and Work Instructions for the preparation and dissemination of intelligence briefs, including reference to the use of CM and 24/7 RN data and information. It has also finalised the risk profiling of workforce risks SOP and developed a Data and Intelligence Capability Framework which outlines the capability requirements required for the use of data and intelligence in decision making within the Commission.
The Commission acknowledges that compliance with these measures is impacted by a range of factors in addition to the Commission’s specific regulatory activities. Our evaluation, in collaboration with the Department, will seek to understand our contribution to promoting compliance with the CM and 24/7 RN regulation, and more broadly, its relationship to quality and safety outcomes for consumers.
Key messages from this audit for all Australian Government entities
Below is a summary of key messages, including instances of good practice, which have been identified in this audit and may be relevant for the operations of other Australian Government entities.
Policy/program design
Policy/program implementation
1. Background
Introduction
1.1 Residential aged care refers to accommodation and services that are provided to a person whose physical, mental or social functioning is affected to such a degree that the person cannot maintain themself independently.1 This care is subsidised by the Australian Government for persons who are aged at least 65 years, and for Aboriginal and Torres Strait Islanders and persons at risk of homelessness who are aged at least 50 years.2 The funding is paid directly to approved providers of residential care3 conditional on the provider complying with its responsibilities under the Aged Care Act 1997 (Aged Care Act). These responsibilities include ensuring that care is safe and of suitable quality. The Aged Care Act and Aged Care Quality and Safety Commission Act 2018 (the Acts) govern the provision of Australian Government funding to residential aged care providers.
1.2 For-profit, not-for-profit, and state, territory and local government entities may apply under the Acts to become approved providers of residential aged care. Approved providers may operate one or several residential aged care services, defined in the Acts as an undertaking through which residential care is provided. Each service provides care to approved care recipients at one or more residential aged care facilities (Figure 1.1). On 30 June 2023, there were 764 approved providers of 2639 mainstream services4 operating at 2559 facilities providing care to 185,127 permanent residents.5
Figure 1.1: Aged care provision under the Aged Care Act 1997

Source: Aged Care Act 1997.
1.3 The Aged Care Act contains special provisions that allow the Australian Government to subsidise residential aged care in Multi-Purpose Services (MPS), which are combined health and aged care services in small regional and remote communities. MPS are ordinarily funded jointly by the Australian Government and state and territory governments. Outside the provisions of the Aged Care Act, the Australian Government also operates the National Aboriginal and Torres Strait Islander Flexible Aged Care (NATSIFAC) Program to fund aged care services for older Aboriginal and Torres Strait Islander people (Table 1.1 and Figure 1.2). These services comprise approximately 1.7 per cent of total aged care places and are often the only available residential aged care option in large areas of Australia.
Table 1.1: Subsidised residential aged care places, by service type, at 30 June 2023
|
Type of service |
Number of operational residential places |
|
Mainstream services |
221,467 |
|
Multi-Purpose services |
3250 |
|
National Aboriginal and Torres Strait Islander Flexible Aged Care Program |
489 |
|
Total |
225,206a |
Note a: Excludes 10 residential places in the Innovative Care Programme, which is designed for younger people with disabilities.
Source: ANAO, based on Australian Institute of Health and Welfare, Aged care service list, 30 June 2023, https://www.gen-agedcaredata.gov.au/resources/access-data/2023/september/aged-care-service-list-30-june-2023 [accessed 16 October 2023].
Figure 1.2: Location of residential aged care services in Australia
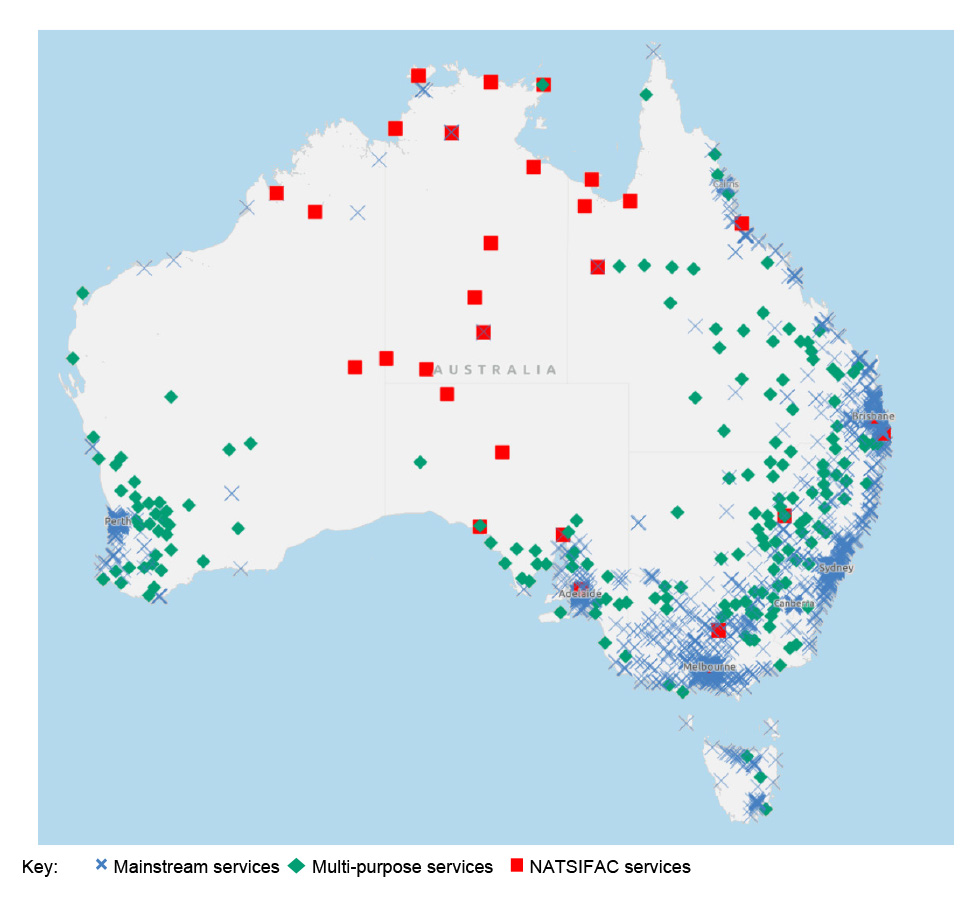
Note: Excludes external territories and Lord Howe Island.
Source: ANAO, based on Australian Institute of Health and Welfare, Aged care service list, 30 June 2023, https://www.gen-agedcaredata.gov.au/resources/access-data/2023/september/aged-care-service-list-30-june-2023 [accessed 16 October 2023].
1.4 The Australian Government Department of Health and Aged Care (the department) is responsible for administering the Acts and delivering residential aged care programs that contribute to improved wellbeing for older Australians.6 The Aged Care Quality and Safety Commission is a statutory agency responsible for regulating aged care quality and safety.
Royal Commission into Aged Care Quality and Safety
1.5 On 6 December 2018 the Australian Government established a Royal Commission to inquire into Commonwealth-funded aged care services, including actions that could be taken to ensure aged care services are high quality, safe and person-centred; and to recommend policy, legislative, administrative or structural reforms. The 2021 final report of the Royal Commission stated:
We consider that the extent of substandard care in Australia’s aged care system is deeply concerning and unacceptable by any measure. We also consider that it is very difficult to measure precisely the extent of substandard care, and that this must change. Australians have a right to know how their aged care system is performing; their government has a responsibility to design and operate a system that tells them; and aged care providers have a responsibility to monitor, improve and be transparent about the care they provide. The extent of substandard care in Australia’s aged care system reflects both poor quality on the part of some aged care providers and fundamental systemic flaws with the way the Australian aged care system is designed and governed.7
1.6 The report made 148 recommendations, including a new legislative framework for aged care, a new model for funding aged care places, a new model for regulating the aged care sector, and new monitoring and transparency arrangements.
Recommendation 86
1.7 Between July 2014 and June 2019, residential aged care providers were required under the Quality of Care Principles 2014 to ensure that ‘adequate numbers of appropriately skilled and trained staff and volunteers are available for the safe delivery of care and services’.8 From July 2019, revised quality standards specified that residential aged care providers must demonstrate that their ‘workforce is planned to enable, and the number and mix of members of the workforce deployed enables, the delivery and management of safe and quality care and services’.9
1.8 In 2018–19 the Royal Commission commissioned a report from the University of Wollongong, which found that, on average, each aged care resident received 180 minutes of care per day on average, of which 36 minutes were provided by a registered nurse (RN). Between 2020 and 2022, departmental estimates of the proportion of facilities that rostered an RN overnight ranged from 46 to 80 per cent (see paragraph 2.31).
1.9 Recommendation 8610 was that approved providers, from 1 July 2022:
- engage RNs, enrolled nurses and personal care workers for at least 200 minutes per resident per day, with at least 40 minutes of that time provided by RNs (‘200/40 care minutes’); and
- ensure a RN is on-site at each residential aged care facility during every morning and afternoon shift (16 hours per day, seven days a week) (‘16/7 RN’).
1.10 The Commissioners also recommended that, from 1 July 2024:
- care minutes should increase to 215 minutes, with at least 44 minutes of that time provided by RNs (‘215/44 care minutes’); and
- a RN is on-site at all residential aged care facilities at all times (‘24/7 RN’).
1.11 The recommended care minutes per resident per day represented the appropriate level of staffing for ‘the average resident’. The recommendation further provided that the exact target of care minutes required to be delivered by an approved provider should be adjusted according to the assessed care needs (case mix) of its residents. The Royal Commission stated that ‘this means that approved providers with a higher than average proportion of high needs residents would be required to engage additional staff, and vice versa.’
1.12 In May 2021 the Australian Government accepted Recommendation 86 and provided $3.9 billion over four years to support the introduction of care minutes. The funding initially supported residential aged care services to voluntarily achieve 200/40 care minutes and 16/7 RN from 1 October 2022. The Australian Government decided minimum care minutes and 16/7 RN would be mandated from 1 October 2023 (see Table 1.2 and Appendix 3). Minimum staff time standards would be set in a new Aged Care Act ‘due to commence from 1 July 2023, subject to parliamentary processes’.
1.13 In July 2022 the Australian Government’s policy was to implement 200/40 care minutes on the previously specified timeframe and to introduce 24/7 RN by 1 July 2023, 12 months earlier than the Royal Commission recommendation (Table 1.2). The Australian Government committed an additional $2.5 billion over four years to support the introduction of 24/7 RN and an increase to 215/44 care minutes commencing 1 October 2024.
Table 1.2: Summary of Australian Government response to Recommendation 86
|
Pre-existing situation |
Royal Commission recommendation |
Government policy May 2021 |
Government policy July 2022 |
|
Care minutes — Providers were required to provide ‘sufficient’ staffing but there was no minimum standard for care minutes. In 2018–19, on average, each resident received 180 minutes of care per day, of which 36 minutes were provided by RNs. |
From 1 July 2022, 200/40 care minutes |
From 1 October 2022, additional funding to be provided to support voluntary provision of 200/40 care minutes. From 1 October 2023, 200/40 care minutes to be mandatory. |
From 1 October 2022, additional funding to be provided to support voluntary provision of 200/40 care minutes. From 1 October 2023, 200/40 care minutes to be mandatory. |
|
From 1 July 2024, 215/44 care minutes |
Agreed with recommendation but no decision taken. |
From 1 October 2024, 215/44 to be mandatory. |
|
|
Registered nurses — Providers were required to deliver an appropriate standard of care but there was no minimum RN requirement. In 2020 to 2022, estimates of the proportion of facilities with an RN rostered overnight ranged between 46 and 80 per cent. |
From 1 July 2022, 16/7 RN |
From 1 October 2022, additional funding to be provided to support voluntary provision of 16/7 RN. From 1 October 2023, 16/7 RN to be mandatory. |
From 1 October 2022, additional funding to be provided to support voluntary provision of 16/7 RN. Mandatory requirement for 16/7 RN superseded by bringing forward 24/7 RN to 1 July 2023. |
|
From 1 July 2024, 24/7 RN |
Agreed with recommendation but no decision taken. |
From 1 July 2023, 24/7 RN to be mandatory. |
|
Source: ANAO analysis.
Aged care workforce
1.14 In October 2019 the Royal Commission commissioned a study by the University of Wollongong which compared residential aged care staff levels in Australia to national and international benchmarks. The study found that 58 per cent of Australian aged care residents were in facilities that had ‘unacceptable’ levels of staffing (1 or 2 stars on the USA Centers for Medicare and Medicaid Services Nursing Home Compare system), 27 per cent had ‘acceptable’ levels (3 stars), 14 per cent had ‘good’ levels (4 stars) and one per cent had ‘best practice’ levels (5 stars).
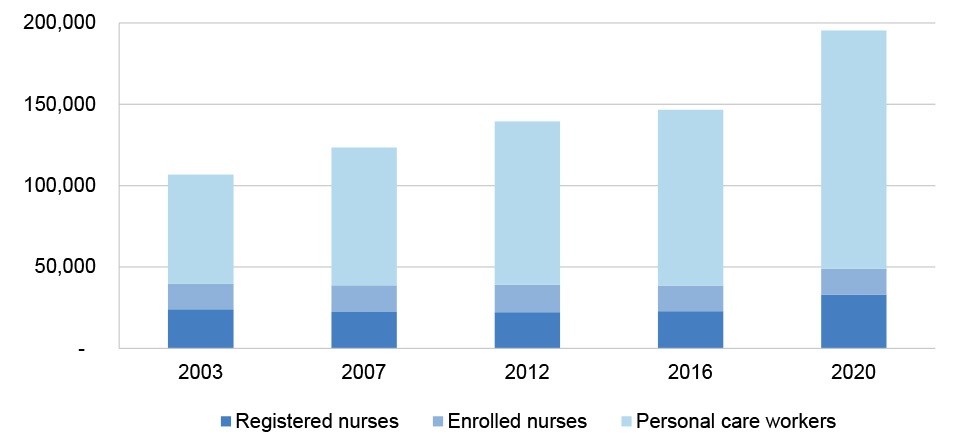
1.15 Aged care workforce modelling undertaken by Deloitte Access Economics for the Royal Commission estimated that the number of direct care workers needed to maintain current care levels, before any reforms, would be around 316,500 full time equivalent (FTE) workers by 2050 (Figure 1.3). It also estimated the number of FTE workers required at 3, 4 and 5-star levels of care.
Figure 1.3: Direct care aged care workforce requirements, by different levels of care
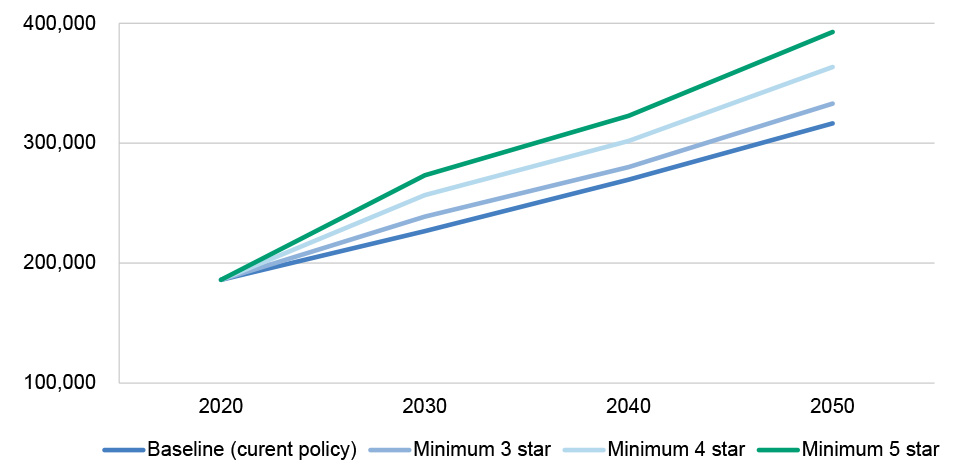
Note: Direct care workers are those who work directly with residents to provide care, and exclude kitchen workers, cleaners, gardeners, drivers, security and people performing administrative roles. Estimates are for full-time equivalent workers. Baseline estimates are based on 2016 National Aged Care Workforce Census estimates. ‘3 star’ is based on 216/40 care minutes per resident per day, or ‘acceptable levels of staffing’. ‘4 star’ is based on 247/47 care minutes per resident per day, or ‘good levels of staffing’. ‘5 star’ is based on 269/64 care minutes per resident per day, or ‘best practice levels of staffing’. The modellers treated 2020 as the baseline year and no differentiation was made in the modelling between requirements under current policy, and different star levels in 2020.
Source: ANAO, based on Royal Commission into Aged Care Quality and Safety, Final Report: Care, Dignity and Respect, Volume 3A The new system, p. 375, https://agedcare.royalcommission.gov.au/sites/default/files/2021-03/final-report-volume-3a_0.pdf [accessed 14 August 2023].
1.16 Modelling undertaken by the Committee for Economic Development of Australia in August 2021 estimated a shortfall of more than 110,000 direct care workers in residential and home care within a decade, and a shortfall of 400,000 direct care workers in residential and home care by 2050, to reach the standard of care recommended by the Royal Commission.11 The University of Technology Sydney Ageing Research Collaborative estimated in November 2022 that an additional 6922 RNs were required to implement 200/40 care minutes and 24/7 RN.12 Revised estimates in May 2023, approximately one month before 24/7 RN was to become mandatory and six months before 200/40 care minutes were to become mandatory, were that an additional 5911 RNs were required to meet the requirements.13
1.17 The Royal Commission found that the aged care sector faced barriers to attracting and maintaining well-skilled aged care workers, including low wages, poor employment conditions, lack of training, and limited career progression opportunities. The Commissioners noted that there may be circumstances where a time-limited exemption from the 24/7 RN requirement might be appropriate, where the provider could demonstrate it had been unable to recruit sufficient numbers of staff with the requisite skills.
1.18 The department has identified a need for a national strategy that looks at nursing workforce supply across all sectors including aged care. The department advised the Senate in February 2023 that a strategy would be developed by October 2024.
Rationale for undertaking the audit
1.19 Each year approximately 250,000 older Australians receive residential aged care on a permanent basis. The 2021 report of the Royal Commission into Aged Care Quality and Safety made 148 recommendations, including that RN and overall care minutes provided to each resident be increased (Recommendation 86).
1.20 The Australian Government has identified that aged care providers face challenges in attracting sufficient RNs and other aged care staff, particularly in rural and remote settings. This audit provides early assurance to the Australian Parliament over whether the Department of Health and Aged Care and the Aged Care Quality and Safety Commission have effectively supported the design and early implementation of Recommendation 86.
Audit approach
Audit objective, criteria and scope
1.21 The objective of the audit was to assess whether the design and early implementation of the Australian Government’s response to Recommendation 86 of the Royal Commission into Aged Care Quality and Safety has been effective.
1.22 To form a conclusion against the objective, the ANAO adopted the following high-level criteria which were sourced from whole-of-government and entity-level policy and operational frameworks.
- Did the Department of Health and Aged Care provide robust policy advice on residential aged care workforce reforms?
- Has the Department of Health and Aged Care effectively introduced the new workforce requirements?
- Is the regulatory system prepared for the new requirements?
1.23 The audit examined preparations made by the department and the Aged Care Quality and Safety Commission primarily in the period leading up to the implementation of mandatory care minutes and 24/7 RN. The audit did not evaluate the effectiveness of Australian Government initiatives aimed at improving aged care workforce supply and retention. The audit did not examine the effectiveness of the Australian National Aged Care Classification (AN-ACC) funding model or Services Australia’s payments to aged care providers.
Audit methodology
1.24 The audit examined relevant records and data for the period 1 January 2020 to 1 October 2023 and involved:
- reviewing submissions and briefings to the Australian Government;
- reviewing entity documentation, including meeting papers and minutes, policies and procedures, and correspondence;
- reviewing documentation for IT system development and data flows across entity IT systems;
- analysing aged care data held by the department in its enterprise data warehouse or made public by the Australian Institute of Health and Welfare;
- meeting with officers from relevant business areas within each entity; and
- reviewing nine submissions received by the ANAO from organisations and individuals.
1.25 Australian Government entities largely give the ANAO electronic access to records by consent, in a form useful for audit purposes. In April 2022 the Department of Health and Aged Care advised the ANAO that it would not voluntarily provide certain information requested by the ANAO due to concerns about its obligations under the Privacy Act 1988, secrecy provisions in Health portfolio legislation, confidentiality provisions in contracts and the Public Interest Disclosure Act 2013.14 For the purposes of this audit, the Auditor-General therefore exercised powers under section 33 of the Auditor-General Act 1997 to enable authorised ANAO officers to attend premises, and examine and take copies of documents. The department facilitated authorised officers attending the department’s premises to examine and copy documents, however the requirement was extended by the department to all documents, including those which did not relate to the department’s obligations under legislation. The department advised that this type of information largely was not segregated in the department’s record-keeping systems and the department could not be certain, in providing documents through electronic means, that documents containing this type of information were excluded. To provide comfort to the Secretary regarding the department’s obligations under portfolio legislation, on 9 August 2023 the Auditor-General issued the Secretary of the department with a notice to provide information and produce documents pursuant to section 32 of the Auditor-General Act 1997. Under this notice, the department agreed to provide the information and documents requested through electronic means.
1.26 The audit was conducted in accordance with ANAO Auditing Standards at a cost to the ANAO of approximately $660,700.
1.27 The team members for this audit were Michael McGillion, Kai Swoboda, Dr Jennifer Canfield, Sam Hayward, Bezza Wolba, Grace Sixsmith, Alexander Wilkinson, Ben Thomson and Christine Chalmers.
2. Policy advice
Areas examined
This chapter examines whether the Department of Health and Aged Care (the department) provided robust policy advice to the Australian Government relating to Recommendation 86 of the Royal Commission into Aged Care Quality and Safety (the Royal Commission).
Conclusion
The department provided largely robust policy advice on residential aged care reforms in response to Recommendation 86. Advice was informed by workforce data and modelling, and conveyed some costs, benefits and risks of the proposed policies. However, established Australian Government mechanisms for analysing the costs, benefits and risks of policy options were not fully utilised. There was a lack of structured risk analysis as required under Australian Government policy. Evaluation planning was not properly addressed in policy proposals.
Areas for improvement
The ANAO made two recommendations to the department regarding compliance with Australian Government budget policy requirements to assess the risk of new policy proposals and the evaluation of the new residential aged care workforce measures.
2.1 The Australian Government’s Delivering Great Policy model specifies that when providing policy advice, agencies should clearly define the objectives of a proposed policy; provide options that identify the key risks and benefits; be informed by quantitative and qualitative evidence; collaborate with people affected by the policy; incorporate lessons from past experience; and provide a practical plan for implementation.15 Implementation plans should identify deliverables and milestones and embed evaluation at the outset.
Did policy advice assess the costs and benefits of policy options?
Between March 2021 and March 2023, the department presented policy options to the Australian Government to respond to Recommendation 86. The department relied on a process to certify that a Regulatory Impact Statement did not need to be prepared for Recommendation 86 policy options, with the result that some analysis normally addressed in a Regulatory Impact Statement was not provided.
Advice provided between March 2020 and May 2022
2.2 The department provided initial advice to the government about mandatory staffing levels in residential aged care facilities to inform the government’s consideration of submissions from Counsel Assisting the Royal Commission in March16 and October 2020.17 The submissions included proposals for minimum care minutes ranging from 186 to 265 care minutes per resident per day, and for 24/7 RN (see paragraph 1.9 for an explanation of these measures).18 The department’s 2020 advice to government did not address the costs or benefits of these proposals.
2.3 The Australian Government’s Regulatory Impact Analysis Framework that applied at the time the policy proposals were developed required entities that put policy proposals to government to ordinarily complete a Regulatory Impact Statement (RIS).19 A RIS is intended to answer seven questions20 and is a key mechanism for communicating the costs and net benefits of a policy option. A RIS is not required for a regulatory proposal ‘where an independent review or other similar mechanism has undertaken a process and analysis equivalent to a RIS’.21 Where a RIS is not prepared because of an equivalent process, a senior executive from the entity is required to certify that the independent review followed a similar process to that required for a RIS and has adequately addressed all RIS questions. The regulatory costs must be quantified in the independent review or the certification letter.
2.4 The department presented its advice to government through several policy proposals. An initial tranche of higher priority proposals relating to the Royal Commission’s suite of recommendations (but excluding mandatory care minutes) was progressed in February 2021, followed by a tranche which included mandatory care minutes in March 2021. For both tranches, the department used a certification letter to meet RIS requirements, citing infeasible timeframes to undertake a RIS. For example, on 22 March 2021 the department completed a certification in relation to ‘a number of aged care quality measures currently being considered by Government’, including mandatory care minutes, with an estimated annual regulatory cost of $2 billion.22 The March 2021 certification letter stated that several reviews, in combination with an implementation and evaluation process still to be developed, satisfied the RIS requirements. The Office of Impact Analysis (the OIA)23, which administers the RIS process, does not assess the quality of independent reviews and RIS-like documents used in lieu of a RIS, but does assess relevance. In this case, the OIA assessed that the options analysed in the certified reviews were sufficiently relevant to the Government’s proposed responses.
2.5 The department’s March 2021 advice to government presented three options for the government to consider (200/40 care minutes and 16/7 RN; 200/40 care minutes and 24/7 RN; 215/44 care minutes and 24/7 RN) as well as options relating to the timing of making care minutes mandatory (October 2022 or October 2023). The March 2021 advice assessed the costs associated with the options. The department assessed the benefits of the proposed policy largely in terms of whether the policy option met the intent of Recommendation 86. The advice accepted the basic premise of the Royal Commission’s findings that measures to increase staffing levels would improve the quality of residential aged care.
2.6 The March 2021 cost estimate included funding for residential aged care providers covered by the Multi-Purpose Services (MPS) and National Aboriginal and Torres Strait Islander Flexible Aged Care (NATSIFAC) programs (see paragraph 1.3). The department’s advice did not make explicit that the benefits of the proposed care minutes and 24/7 RN policies would extend to residents of these non-mainstream services and did not discuss how care minute and 24/7 RN requirements for these services would be met.
2.7 The March 2021 advice about regulating the care minutes and RN staffing measures proposed that the Aged Care Quality and Safety Commission be given responsibility for monitoring and enforcing compliance from October 2023.
Advice provided between June 2022 and June 2023
2.8 In June 2022 the OIA advised the department that supplementary RIS analysis was needed on the implementation and evaluation measures, which had been foreshadowed in the department’s March 2021 certification letter, to meet the requirements of the certification process.
2.9 As noted at paragraph 2.3, a RIS is a key mechanism for communicating the costs and net benefits of a policy option. In the period prior to June 2022, the department relied on a certification letter to meet RIS requirements in the year leading up to the implementation of 24/7 RN. A third certificate24 was issued in July 2022 for the 215/44 care minutes and 24/7 RN proposals. The department prepared a supplementary RIS in June 2022 to separately examine, at a high level, the implementation and evaluation arrangements.25 The OIA was not required to, and did not, assess the quality of the supplementary RIS analysis.
2.10 In July 2022 the department provided policy advice to the Minister for Health and Aged Care and the Minister for Aged Care about introducing 24/7 RN in July 2023 rather than July 2024 and implementing 215/44 care minutes from 1 October 2024. The advice examined the costs of implementing 24/7 RN from 1 July 2023 and 215/44 care minutes from 1 October 2024, including for MPS and NATSIFAC providers.
2.11 In March 2023 the department provided advice about the additional cost for 24/7 RN and 215/44 care minutes posed by the government’s response to a decision of the Fair Work Commission that there should be a 15 per cent increase to award wages from 1 July 2023 for selected aged care workers.
Did policy advice assess risk and propose mitigation strategies?
The department’s policy advice between March 2021 and March 2023 identified some risks associated with responding to Recommendation 86, such as workforce shortages, provider viability and unintended consequences of the new measures such as care shifting. The advice proposed mitigation strategies for these risks. However, there was no structured risk analysis, including through a Risk Potential Assessment Tool, which is required under Australian budget policy.
Assessment of risk
2.12 Australian Government budget policy requires Commonwealth entities to complete a structured risk assessment (a Risk Potential Assessment Tool or RPAT) for new policy proposals with an estimated financial implication of $30 million or more, and encourages entities to complete an RPAT for all other new policy proposals.26 Additionally, entities are required to complete a revised RPAT for approved policy proposals where risk factors have changed (such as a compressed implementation schedule). Auditor-General Report No. 10 of 2022–23 Expansion of Telehealth Services suggested the department should ensure that a Risk Potential Assessment Tool is completed for all new policy proposals with a financial impact of $30 million.27
2.13 The department did not complete a structured risk assessment for the Recommendation 86 measures, either through an RPAT or another mechanism.
- The department completed an RPAT in March 2021 when preparing a new policy proposal that covered the introduction of the Australian National Aged Care Classification (AN-ACC) model, mandatory care minutes and 16/7 RN. The RPAT assessed risks of implementing the AN-ACC model but did not assess risks associated with mandatory care minutes or 16/7 RN.
- The department did not comply with the RPAT requirements for a July 2022 new policy proposal for the introduction of 24/7 RN in July 2023 and 215/44 care minutes in October 2024, which had an estimated financial impact of $2.4 billion.
- The department was not required to, and did not, complete an RPAT in September 2022 for 24/7 RN exemptions and supplementary payments. This new policy proposal had a financial impact of $26 million.
Recommendation no.1
2.14 The Department of Health and Aged Care ensure that Risk Potential Assessment Tools are completed in accordance with Australian Government policy, in particular the requirement to complete a Risk Potential Assessment Tool for new policy proposals with a financial impact of $30 million, and the requirement to revise a Risk Potential Assessment Tool for approved policy proposals when there is a significant change to one or more risk factors affecting implementation. The Department of Health and Aged Care should promote the use of the Risk Potential Assessment Tool for new policy proposals of less than $30 million.
Department of Health and Aged Care response: Agreed.
2.15 The Department of Health and Aged Care requires adherence to Government requirements with respect to the completion of Risk Potential Assessment Tools (RPATs) for all new policy proposals, including those outlined in the Cabinet Handbook and Budget Process Operational Rules (BPORs). In 2023, Budget Strategy Branch delivered Budget training sessions, which included outlining the requirements for RPATs. These sessions had over 1,950 attendees, with recordings published on the department’s Budget Literacy Intranet site. Training will be continuously reviewed to ensure alignment to the BPORs and will be actively promoted through departmental communications channels ahead of future Budget contexts.
2.16 Advice to the government on new policy proposals must contain a discussion of key risks and implementation challenges.28 Although there was no structured risk assessment, the department advised the government of some of the key risks associated with its proposed responses to Recommendation 86. Identified risks of mandatory care minutes and 24/7 RN included:
- COVID-19 pandemic risks — the comparative priority of responses to the COVID-19 pandemic over structural reform;
- workforce risks — challenges for providers in recruiting staff, particularly RNs in regional/remote areas;
- provider viability risks — care minutes funding not adequate across resident categories and the risk that the complexity of broader aged care reforms may overwhelm a sector that is experiencing significant challenges; and
- risk of unintended adverse consequences — unintended outcomes as providers prioritise the new requirements, such as changing models of care in ways that might disadvantage residents (for example, reducing the number of enrolled nurses).
Mitigation of risk
2.17 One of the identified risks to implementation of Recommendation 86 measures related to challenges in recruiting sufficient workforce, particularly RNs in regional and remote areas (see paragraph 1.17). Various advice to government between March 2021 and March 2023 discussed mitigations to workforce risks.
- March 2021 advice included estimates of the additional workforce requirements (above and beyond baseline requirements) associated with 200/40 care minutes and noted that home and residential aged care would need an additional 13,600 registered nurses and 34,200 personal care workers by the end of June 2023. The department advised the government on potential measures to improve the supply and capability of the workforce such as targeted funding and additional training places. The advice did not address whether the proposed workforce measures would provide sufficient additional workers to meet the mandatory care minute and 24/7 RN requirements.
- In June 2022 the department provided revised advice on the aged care workforce and noted that there was a gap between workforce supply and demand. The advice quantified the estimated gap at the commencement of 200/40 care minutes and 24/7 RN following the government’s decision to make 24/7 RN mandatory from 1 July 2023. The June 2022 advice included high-level information about existing workforce measures and noted that additional activities would be required to meet forecast demand.
- One mitigation of the workforce risk was to put in place an exemption to the workforce requirements for certain providers. July 2022 advice to government on the risk of providers being unable to comply with mandatory care minutes and 24/7 RN due to workforce shortages was not supportive of an exemption framework for the 24/7 RN requirement. September 2022 advice noted that exemptions would assist those facilities that faced the greatest challenges in meeting the 24/7 RN requirement, proposing that exemptions be restricted to facilities with 30 or fewer approved beds located in small rural towns, remote communities and very remote communities.29 The department advised that approximately six per cent of residential aged care facilities would be eligible.
- In March 2023 the department presented quantitative estimates of the expected impact of the Recommendation 86 measures on the available aged care workforce. The department’s advice about risks associated with workforce challenges referred to the mitigating impact of programs to increase the size and capacity of the workforce.
2.18 July 2022 and January 2023 advice discussed mitigations to provider financial viability risks.
- To address risks that some providers could not pay for 24/7 RN, in July 2022 the department suggested a supplementary payment for certain providers. The department’s proposed approach was to pay facilities with up to 60 residents at a tapered rate that was higher for rural, remote and very remote areas.
- January 2023 advice to the Minister for Aged Care and the Minister for Health and Aged Care proposed the equitable provision of care associated with the allocation of funding and proposed adjustments to the funding model.
2.19 Another identified risk related to unintended adverse consequences of the Recommendation 86 measures, such as providers changing models of care to meet the requirements. November 2022 briefings to the Minister for Health and Aged Care and the Minister for Aged Care cited media reports of providers altering clinical care arrangements by reducing enrolled nurse staffing and substituting enrolled nurses with lower-qualified personal care workers (care shifting). In February and March 2023 the department presented potential policy responses to address care shifting. These included monitoring enrolled nurse care minutes in provider quarterly reporting.
Was policy advice based on sound evidence?
The department used workforce modelling and data to support its policy advice. It used this evidence to project how many additional workers would be required to implement mandatory care minutes and 24/7 RN, and to estimate how workforce supply would be improved through other Australian Government initiatives. Different RN workforce gap estimates were produced, depending on which data source was used. Although some of the data that informed the modelling had methodological limitations that were considered to over-state estimates of workforce supply, these limitations were acknowledged by the department and attempts were made over time to improve the data. The department considered the views of stakeholders in developing its policy advice.
Workforce modelling
2.20 Among the key risks identified by the department in its policy advice to government was the challenge for providers in recruiting staff, particularly RNs in regional/remote areas (see paragraph 2.17). The department developed a workforce model which estimated growth in the aged care workforce since the 2020 Aged Care Workforce Census (see paragraph 2.24), based on growth patterns observed in Australian Bureau of Statistics labour force quarterly data. Starting from an assumption that residential aged care labour demand and supply were equal in 2021–22, the model estimated growth in baseline (before the introduction of the new measures) demand.
2.21 The model separately estimated the additional labour demand associated specifically with the introduction of care minutes and 24/7 RN. The additional labour demand was estimated by assuming that the shortfall between the minimum care minute and RN shift coverage standards and actual care provided represented a need for additional labour. The department used financial reports lodged by providers to calculate the care time provided, and used the 2020 Aged Care Workforce Census and financial reports to estimate the current RN shift coverage. The department used the workforce model to estimate the ‘gap’ between workforce supply and demand for RNs, enrolled nurses (ENs) and personal care workers (PCWs) (Figure 2.1).30
Figure 2.1: Departmental estimates of residential aged care workforce supply and demand 2023–24 to 2031–32, as at July 2022
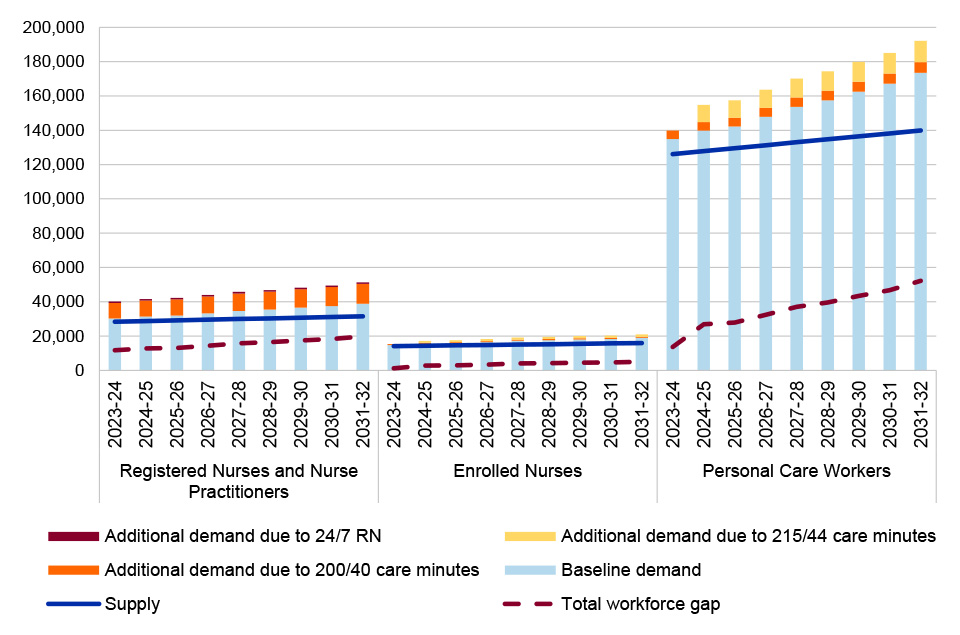
Source: ANAO based on departmental records.
2.22 The estimated additional demand was advised to the government in March 2021, and the estimated workforce gap was advised from June 2022.
- The department advised the government in March 2021 that an additional (above and beyond baseline requirements) 12,700 RNs, 1900 ENs and 17,000 PCWs were required in 2022–23 to deliver 200/40 care minutes in residential care facilities. The advice did not estimate the additional workforce requirements needed to implement 16/7 RN or 24/7 RN.
- The department advised the government in June 2022 on the workforce required to deliver 200 care minutes, 24/7 RN from 1 July 2023 and 215/44 care minutes from October 2024. At the request of the Minister for Aged Care through the Minister’s office, the advice drew attention to the workforce gap between supply and demand for the three occupational groupings (RNs, ENs and PCWs) for 2023–24 to 2031–32. For 2023–24, the estimated gap was 11,758 RNs, 1234 ENs and 13,679 PCWs.
- The department advised government on the estimated 2023–24 gaps for RNs, ENs and PCWs in July 2022, and provided updated RN gap estimates to the Senate in February 2023 and May 2023 (see Figure 2.2). The estimated additional demand associated with care minutes and 24/7 and the estimated gap were updated each time based on newly available data and different assumptions about RN shift coverage (see note to Figure 2.2).
Figure 2.2: Updates to departmental estimates of 2023–24 additional demand for registered nurses
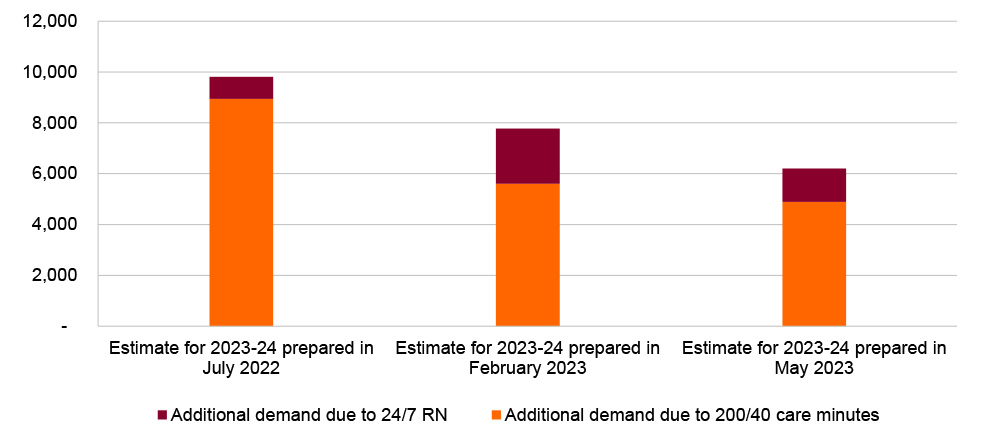
Note: Additional demand estimates for 24/7 RN made in July 2022 assumed 80 per cent of facilities already had an RN on duty 24/7. This assumption was changed to 50 per cent for the estimates made in February 2023 and 70 per cent for the estimates made in May 2023. See paragraph 2.31 for the reason for the change in assumption from 80 to 50 to 70 per cent.
Source: ANAO based on department ministerial and Senate estimates briefings.
2.23 The department’s estimates of the gap between supply and demand did not incorporate the estimated impact of Australian Government initiatives to grow the aged care workforce (such as support for wage increases, skilled migration and training and retention programs). In September 2022 the department had developed estimates of the ‘best-case’ and ‘worst-case’ impact of key workforce initiatives. In March 2023 it advised the government that the initiatives had potential to reduce the gap to 3400 RNs, 2000 ENs and 1500 PCWs in 2023–24. The advised impact for RNs was largely aligned to the best-case scenario. The department did not advise there was a range of estimates based on its September 2022 modelling. The department indicated that the estimates ‘are designed to illustrate the possible effects of different actions but are difficult to predict with certainty’.
Workforce data
2.24 As noted at paragraph 2.20, the model used data collected through a census of residential aged care providers. The department conducted similar censuses in 2003, 2007, 2012 and 2016. The department conducted another census (the 2020 Census) on 7 December 2020, which requested all providers report on their workforce as it was in November 2020. Providers were granted extensions until late January 2021 due to a low response rate.
2.25 The 2020 Census indicated that there had been an increase in the size of the total residential aged care workforce (comprising RNs, ENs and PCWs) of 33 per cent from 2016 to 2020 (Figure 2.3). Most of the increase was in PCWs, however the number of RNs also increased by 44 per cent.
Figure 2.3: Residential aged care workforce headcount, 2003 to 2020
Note: The category of RNs includes nurse practitioners from 2012. Prior to 2020 the term ‘personal care attendant’ was used instead of ‘personal care worker’.
Source: Department of Health, Aged Care Workforce, 2016, March 2017, p. 13, available at https://gen-agedcaredata.gov.au/www_aihwgen/media/Workforce/The-Aged-Care-Workforce-2016.pdf [accessed 10 August 2023]; Department of Health, 2020 Aged Care Workforce Census Report, September 2021, p. 11, health.gov.au/sites/default/files/documents/2021/10/2020-aged-care-workforce-census.pdf [accessed 10 August 2023].
2.26 Prior to 2020, there was insufficient information available about which facilities employed an RN 24/7. The department added a new question to the 2020 Census which asked providers whether an RN was rostered on duty overnight every day in the last fortnight.31 This additional question provided previously unavailable information that was directly relevant to implementing 24/7 RN. The 2020 Census found that 80 per cent of facilities had an RN rostered on duty overnight every day in the preceding fortnight, while a further nine per cent had an RN on call every night. The department used these figures in its advice to government in October 2021.
2.27 Although it was described as a ‘census’, less than half (49 per cent) of providers returned valid responses to the 2020 Census.32 Furthermore, the department acknowledged that workers might be duplicated in headcount totals if they worked across multiple facilities. To correct for non-response and obtain estimates for the sector as a whole, the department applied weightings derived from response rates across planning regions. The application of these weightings was informed by work performed by the University of Wollongong.
2.28 An academic paper published in September 2022 drew attention to several shortcomings of the 2020 Census in measuring the size of the workforce due to double counting workers with multiple jobs, the inclusion of COVID-19 surge staff in provider reports, and methodological factors associated with response rates, weightings and converting headcounts to full-time equivalent workers.33 The paper asserted that the reported increase in the workforce was inflated by these extraneous factors34, and that the data and analyses needed to be treated with caution and could not be relied upon for projections to inform policy.
2.29 The department was invited to review the paper before it was published. The department’s response to the author acknowledged the reliability of the 2020 Census may have been affected by the COVID-19 pandemic response (including the counting of ‘surge’ staff), and the relatively low response rate. It noted that it had contracted Quantium Health to undertake a process to de-duplicate workers in head-count totals through an examination of multiple data sets, including Australian Bureau of Statistics data. It also noted that the weightings for residential care workers were not identified as problematic by the statistician who had developed the weights.
2.30 The department advised the government in July 2022 that it had some concerns about the 2020 Census result relating to 24/7 coverage across facilities, cautioning that the finding that 80 per cent of services had 24/7 RN might have been an overstatement.
2.31 Between November 2022 and June 2023, the department’s data about the aged care workforce was supplemented with data derived from analysis of RN shift information collected through the Quarterly Financial Report (QFR).35 March 2023 advice to government included workforce estimates that took into account the first instalment of QFR data (July to September 2022). These estimates suggested that a lower proportion of facilities already had an RN on duty 24 /7 than the 80 per cent estimate derived from the 2020 Census. Based on the derived data, fewer than half (46 per cent) could be considered as providing 24/7 RN at all times in the quarter. In the department’s May 2023 Senate estimates briefing pack, analysis of the second instalment of QFR data (October to December 2022) stated that around 70 per cent of residential aged care facilities had ‘the capacity’ to meet the 24/7 RN requirement. The department’s estimates of the gap (see Figure 2.2) incorporated these changed estimates of 24/7 RN coverage.
Stakeholder engagement
2.32 As part of the implementation of the AN-ACC funding model, the department convened a working group in September 2019 (Residential Aged Care Funding Reform Working Group or RACFRWG) to understand stakeholder views about policy options. The membership of RACFRWG in 2021 comprised representatives of 24 organisations including peak bodies representing aged care providers, large corporate providers, advocacy groups for aged care consumers and their families, and other stakeholders such as the Australian Medical Association and the University of Sydney. The RACFRWG first considered care minutes arrangements in August 2021 and considered mandatory care minutes and 24/7 RN at 10 of its 11 meetings between August 2021 and June 2023. The department advised the government on stakeholder opinions collected through the RACFRWG, such as the definition of a PCW, and said it would consult with the RACFRWG about establishing specific EN care minutes targets.
2.33 The department also consulted with the Aged Care Council of Elders in September 202236 and issued draft legislation on 24/7 RN exemptions for public consultation in February 2023. Twenty of the 22 submissions about the draft legislation were from stakeholders that were not represented on the RACFRWG.
2.34 In March 2023 the department advised the Minister for Aged Care about the stakeholder feedback, summarising key themes raised and proposed responses to these. For example, the Minister was told that the legislative instrument had been amended to incorporate requirements that providers must inform care recipients if the facility was subject to an exemption to the 24/7 RN requirement and the conditions the facility was required to meet under the exemption.
Did policy advice contain plans for implementation and evaluation?
The department’s policy advice contained high-level implementation plans. Although some high-level consideration of evaluation was completed as part of a supplementary Regulatory Impact Statement, and elements of an evaluation approach (such as consideration of intended outcomes and data sources) were mentioned in policy advice, there was no defined evaluation plan as at October 2023.
Implementation
2.35 The department provided initial implementation advice to government in March 2021.
- The advice provided a high-level implementation plan that established key commencement dates for care minutes and identified whether the timing was consistent with the timeframe recommended by the Royal Commission. The advice did not establish implementation timing for 215/44 care minutes or 24/7 RN.
- The advice identified which entities would be responsible for implementation, proposing that the Aged Care Quality and Safety Commission (ACQSC) would have responsibility for regulating the arrangements.
- As noted at paragraph 2.6, the proposal for 200/40 care minutes and 16/7 RN included funding for MPS and NATSIFAC services, however the March 2021 advice did not consider the implementation of the new measures or comparable arrangements by MPS and NATSIFAC providers.
2.36 The high-level implementation plan in the March 2021 advice was followed by other implementation considerations in advice provided between June 2022 and March 2023, including the requirement for new legislation, the division of responsibilities between the department and ACQSC, and dependencies with other concurrent aged care reforms.
Evaluation
2.37 Since December 2021 the Commonwealth Evaluation Policy has provided that to support an evaluative culture entities should:
Plan to conduct fit for purpose monitoring and evaluation activities before beginning any program or activity. This includes identifying time-frames, resources, baseline data and performance information.37
The Commonwealth Evaluation Policy built upon requirements for evaluation planning to be properly addressed in proposals and policy impact analysis considered in Budget and Cabinet processes.38 The Australian Government’s Delivering Great Policy model specifies that implementation plans should embed evaluation at the outset.39
2.38 As noted at paragraph 2.4, on 22 March 2021 the department issued a certification stating that RIS requirements for the government’s response to the Recommendation 86 were met through independent reviews, including the Royal Commission. The certification justified not undertaking a RIS by stating that the analysis requirements would be met in part by ‘ongoing evaluation … as part of implementation’. As noted at paragraph 2.8, the department issued another certification on 7 July 2022 which at the request of OIA was accompanied by a supplementary RIS addressing at a high level RIS Question 7, ‘How will you implement and evaluate your chosen option?’ In the supplementary RIS, under the heading of ‘Evaluation’, the department noted that it was planning a ‘multi-level evaluation strategy’.40
2.39 Although the supplementary RIS included some high-level plans for evaluation, as at October 2023, the department had not developed an evaluation plan which41: nominates the criteria by which the success of the policy could be evaluated; identifies which data will be used to measure success and how these relate to the measures of success; establishes baseline measures or benchmarks for impact analysis; and institutes a mechanism to collect this data from the commencement of the policy.
2.40 Although there is no evaluation plan, policy advice set out the expected benefits that could be used to set the criteria of an impact evaluation, such as lifting the quality of care and reduced out of hours hospitalisations.
2.41 In March 2021 the department advised government that it would commission an evaluation of the AN-ACC funding model as a whole, to which care minutes are tied, after two years of operation followed by a five-year Post Implementation Review in 2027.42 The supplementary RIS noted that two years of full operation would enable an accurate assessment of the extent to which the AN-ACC model is achieving reform objectives.
2.42 As part of a separate Royal Commission recommendation agreed to by government (Recommendation 148), the Inspector-General of Aged Care is to undertake independent evaluations of the effectiveness of the measures and actions taken in response to the recommendations of the Royal Commission, five and 10 years after the tabling of the Royal Commission’s final report. As at October 2023 the department had not specifically considered the mechanisms required to enable the Inspector-General of Aged Care to perform this function in relation to mandatory care minutes and 24/7 RN.43
Recommendation no.2
2.43 The Department of Health and Aged Care establish evaluation plans for mandatory care minutes and 24/7 RN in order to settle on the policy objectives to be assessed, potential data sources, baseline data, data collection mechanisms and specific timeframes. Gaps in information required for an effective evaluation should be identified and rectified as part of implementation.
Department of Health and Aged Care response: Agreed.
2.44 The Department of Health and Aged Care (the department) will establish evaluation plans for mandatory care minutes and 24/7 RN to ensure the impact of the policies is measured and delivery of policy objectives is assessed. More broadly the department is working to ensure that evaluation planning, including the collection of baseline data, is undertaken in advance of implementation for the next stage of aged care reforms.
3. Introducing the new workforce requirements
Areas examined
This chapter examines whether the Department of Health and Aged Care (the department) effectively introduced the 24/7 RN and mandatory care minutes requirements recommended by the Royal Commission into Aged Care Quality and Safety (the Royal Commission).
Conclusion
The department’s introduction of the new workforce requirements was largely effective. As at October 2023 the department’s implementation of the requirements through operational arrangements, legislation and IT systems was largely consistent with the government’s policy intent. The 24/7 RN exemption process was consistent with government requirements but delayed. Project management and governance arrangements for the new workforce measures were largely fit for purpose.
3.1 The department must implement new aged care policies in accordance with the decisions of the Australian Government. The department’s project documentation for 24/7 RN and mandatory care minutes (see paragraph 1.9 for a description of these measures) identified design work in three interdependent domains: settling the finer details of operational policy; drafting legislation to give legal effect to operational policy; and designing and deploying IT systems to give practical effect to operational policy. The Australian Government decided that for the first 12 months of 24/7 RN, certain very small regional facilities would be invited to apply for an exemption. The department was also responsible for managing the exemption process. Implementation of the new workforce measures needed to be coordinated with the department’s Aged Care Transformation Program.
Do operational policy, legislation and IT systems for the new requirements conform to the Australian Government’s decisions?
The design of operational policy, legislation and IT systems for 24/7 RN and 200/40 care minutes largely conforms to the Australian Government’s policy decisions. Minor non-conformances comprise: some non-mainstream aged care services being subject to the 24/7 RN requirement without policy authority; IT systems not being updated to accommodate co-located or split services, requiring manual workarounds for a small percentage of facilities in relation to the 24/7 RN requirement; the threshold for payment of the 24/7 RN supplement being lower than that agreed by government; reporting of 24/7 RN compliance not being integrated into facilities’ star ratings; some mandatory care minute targets being lower than the Royal Commission recommended level and other inaccuracies in the calculation of care minute targets; mandatory care minute reporting not being provided at the facility level; and a slight delay in the deployment of IT systems to support public transparency.
24/7 Registered Nurse requirement
3.2 Table 3.1 depicts the decisions of the Australian Government in relation to 24/7 RN. In addition to the core requirement of 24/7 RN, government made decisions about supplementary funding, monitoring and compliance, exemptions and transparency. The ANAO examined whether the department’s design of operational policy, legislation and IT systems for 24/7 RN was consistent with the Australian Government’s policy decisions.
Table 3.1: Operational policy, subordinate legislation and IT system development for 24/7 RN
|
Theme |
Australian Government policy decision |
Operational policy details |
Operational policy conforms to government decisions? |
Legislation |
Legislation prepared on-time? |
IT development undertaken |
Necessary IT systems deployed? |
|
Core requirement |
From 1 July 2023, require mainstream residential aged care facilities to have a RN onsite 24 hours a day, seven days a week. |
Clarification of policy application in all circumstances. |
▲ |
Aged Care Amendment (Implementing Care Reform) Act 2022 |
◆ |
No IT development undertaken to accommodate administration in relation to ‘facilities’ as opposed to ‘services’. |
▲a |
|
Supplementary funding |
Introduce a new non-means tested funding supplement (24/7 RN supplement) to provide additional support to approved providers to deliver on this requirement, to be targeted based on facility bed size and location. First supplement to be payable in August 2023, in relation to the month of July 2023. |
Controls to ensure supplement payment integrity. |
▲ |
Aged Care Legislation Amendment (Subsidies) Principles 2023 |
◆ |
System deployed 3 July 2023 |
◆ |
|
Monitoring and compliance |
Introduce new compulsory monthly reporting by residential aged care services on their compliance with 24/7 RN via an integrated ICT solution to support funding and quality compliance monitoring. No date specified however the ANAO has inferred this was meant to be in place before the end of July 2023, in line with the supplementary funding requirement. |
What the monthly compliance report should contain. |
◆ |
Aged Care Legislation Amendment (Registered Nurses) Principles 2023 |
◆ |
System deployed 3 July 2023 |
◆ |
|
Exemptions |
Provide one-off 12 month exemptions to very small facilities (30 approved beds or less) located in rural and remote (Modified Monash Model 5 to 7) areas where appropriate alternative care arrangements are in place. No date specified however the ANAO has inferred this was meant to be in place before the end of July 2023, in line with the supplementary funding requirement. |
What constitutes appropriate alternative care. |
◆ |
Aged Care Amendment (Implementing Care Reform) Act 2022 Aged Care Legislation Amendment (Registered Nurses) Principles 2023 |
◆ |
System deployed 3 July 2023 |
◆ |
|
Transparency |
From December 2023, public reporting of facility compliance with the 24/7 RN requirement through star ratings. |
How 24/7 RN compliance data will be displayed and integrated into star ratings. |
▲ |
Aged Care Legislation Amendment (Registered Nurses) Principles 2023 |
◆ |
IT system design approved, with IT build commencing in August 2023. |
Not able to be assessed as at October 2023 |
Key: ◆ Conformed to decision of government ▲ Minor non-conformance ■ Major non-conformance
Note a: With the exception of co-located and split service facilities (see paragraphs 3.5 to 3.6), no additional IT development was required to implement the core requirement, as there was an existing system. The assessment reflects that IT development to accommodate co-located and split service facilities was not undertaken.
Source: ANAO analysis of department records and the Federal Register of Legislation.
3.3 Overall, the department has implemented most of the government’s operational policy, legislative and IT requirements for 24/7 RN, including for the core requirement, supplementary funding, monitoring and compliance, exemptions and transparency. There are two minor non-conformances in the department’s implementation of the core 24/7 RN requirement (relating to National Aboriginal and Torres Strait Islander Flexible Aged Care (NATSIFAC) Program providers in operational policy and IT systems); one minor non-conformance in the department’s implementation of supplementary funding; and one minor non-conformance in the department’s implementation of public reporting of facility compliance with 24/7 RN.
Core requirement
Operational policy
3.4 As at 1 July 2023 the Australian Government had not decided whether 24/7 RN should be extended to NATSIFAC services (see paragraph 1.3). However, the department amended the NATSIFAC Program Manual44 such that non-exempted NATSIFAC services were required to comply with 24/7 RN from 1 July 2023. Of 25 NATSIFAC services that provide residential care, 19 had been provided an automatic exemption and six are subject to the 24/7 RN requirement without policy authority. The department advised the ANAO that while there was no explicit policy authority, it had ‘made a policy decision to include 24/7 [RN] as a requirement under the NATSIFAC grant agreement to align with mainstream residential aged care’.
IT systems
3.5 While there is usually a one-to-one relationship between a residential care service and the facility in which it operates, some residential aged care facilities host two or more services (‘co-located’ services) and some services operate across multiple facilities (‘split’ services) (see Figure 3.1). The department advised the Minister for Aged Care (the Minister) in February and March 2023 that it estimated approximately 4.5 per cent of services were co-located and 0.5 per cent were split.
Figure 3.1: Definition of one-to-one, co-located and split services

Note: Facility street addresses are illustrative examples and do not relate to a specific facility.
Source: ANAO, adapted from departmental records.
3.6 The core 24/7 RN requirement was for mainstream facilities to have an RN onsite 24 hours a day, seven days a week from 1 July 2023. Compliance requirements under the Aged Care Act 1997 (Aged Care Act) generally apply to providers or services rather than to facilities. The department identified the application of 24/7 RN to co-located services as an issue needing resolution in June 2022 during the process of developing the primary legislation. It identified which services were co-located through manual analysis of street address data and correspondence with providers and the Aged Care Quality and Safety Commission (ACQSC). This process identified 157 co-located services operating 76 facilities, and two split services — totalling six per cent of mainstream services. On 28 June 2023 the department provided ACQSC with the finalised list of co-located services for the purposes of regulating 24/7 RN.
3.7 As at October 2023 the department’s IT systems did not have functionality that enabled the department to administer compliance requirements that apply to facilities rather than providers or services. For example, the department’s IT system did not support the targeting of compliance obligations or application of funding at a facility level. In the absence of system functionality, to meet requirements for facilities associated with co-located and split services, the department and ACQSC put in place manual processes and workaround solutions for the receipt of 24/7 RN compliance reports, the calculation of the 24/7 RN supplement, and the recording of 24/7 RN exemptions.
3.8 In April 2023 the department raised requests to change IT systems to accommodate co-located and split services, with an indicative deployment date of October 2023. However, the department advised the ANAO in June 2023 it had not yet decided when the IT development would be progressed. The department advised the ANAO that policy development to reform the Aged Care Act (which is planned to commence in 2024) may eliminate the legislative distinction between a service and facility, which would negate the need to change IT systems.
Supplementary funding
3.9 The 24/7 RN supplement was to provide additional financial support to certain approved providers to meet the 24/7 RN requirement. In 2023 the department estimated 1221 facilities would be eligible for an RN supplement payment. The Australian Government decided to introduce the 24/7 RN supplement based on advice from the department that the supplement would be paid only to facilities that were delivering 24/7 RN care.
3.10 On 23 February 2023 the Australian National Aged Care Classification (AN-ACC) and Residential Aged Care Funding Reform (RACFR) Board (the AN-ACC and RACFR Board, see paragraphs 3.38 to 3.39) agreed that from 1 July 2023, providers should receive the supplement if RN care was 23 hours and 15 minutes per day or more. The aim was to provide a degree of tolerance for providers experiencing unexpected RN absenteeism. The AN-ACC and RACFR Board agreed to review the settings after 1 January 2024.
3.11 On 13 April 2023 the department requested that the Minister approve the supplement eligibility threshold of at least 23 hours and 15 minutes per day of RN care. However, following feedback from the Minister through the Minister’s office, on 24 May 2023 the department requested the Minister approve a lower threshold of at least 20 hours per day of RN care. In making the request, the department advised the Minister that this arrangement differed from the Australian Government’s decision, and that it introduced risks that providers may perceive the change as license to provide a lower standard of RN care. The department requested the Minister agree that the department should review this setting in October 2023 (rather than January 2024). The Minister agreed to the department’s proposal. A total of 167 facilities that provided less than 24/7 RN coverage received 24/7 RN supplement payments totalling $2,802,180 for July 2023. The setting was reviewed on 30 October 2023 and a decision was made to leave the lower threshold unchanged.
Transparency
3.12 By September 2023 the department had settled its approach to publicly reporting facility compliance with 24/7 RN. The department planned to publish 24/7 RN coverage statistics for each service adjacent to the service’s staffing star rating on My Aged Care from December 2023.45 However, the integration of 24/7 RN compliance into the star ratings was not planned to be completed by December 2023.
Care minutes
3.13 Table 3.2 depicts the decisions of the Australian Government in relation to mandatory care minutes. In addition to the core requirement of 200/40 care minutes per resident per day, government made decisions about monitoring and compliance, and transparency. The ANAO examined whether the department’s design of operational policy, legislation and IT systems for mandatory care minutes was consistent with the Australian Government’s policy decisions. The department’s activities in relation to non-mainstream aged care services are not assessed in Table 3.2 for reasons discussed in paragraph 3.25.
Table 3.2: Operational policy, subordinate legislation and IT system development for mandatory care minutes
|
Themes |
Australian Government policy decision |
Operational policy details |
Operational policy conforms to government decisions? |
Legislation |
Legislation prepared on-time? |
IT development undertaken |
Necessary IT systems deployed? |
|
Core requirement |
From 1 October 2023, 200 minutes of care per resident per day (including 40 minutes of RN time) will become mandatory. To be tailored for each service (‘case mix adjusted’) based on the relative care needs of its residents. |
How providers’ care time targets will be linked to the AN-ACC casemix model (see Appendix 4) to ensure that targets set a standard of 200 care minutes and 40 RN minutes for the ‘average resident’. How care time targets will be set for each service. Clarification of application to all circumstances. |
▲ |
Aged Care Legislation Amendment (Care Minutes Responsibilities) Principles 2023 |
◆ |
IT system deployed 27 June 2022 |
◆ |
|
Monitoring and compliance |
From 1 July 2022, require provider reporting of care minutes per facility consistent with Recommendation 122 of the Royal Commission.a |
How the data should be reported by providers. What the report should contain. |
▲ |
Aged Care Legislation Amendment (Financial Information) Principles 2022 |
◆ |
In-house IT development delayed and interim solution adopted (outsourced to Forms Administration Pty Ltd) |
◆ |
|
Transparency |
From 1 December 2022, require the publishing of care minutes provided per facility on the My Aged Care websiteb including the conversion of data into a star rating. |
How star ratings should be calculated for care minutes. |
◆ |
Aged Care Legislation Amendment (Financial Information) Principles 2022 |
◆ |
IT system deployed 19 December 2022 |
▲ |
Key: ◆ Conformed to decision of government ▲ Minor non-conformance ■ Major non-conformance
Note a: Recommendation 122 was that from 1 July 2022, the Accountability Principles 2014 (Cth) should be amended to require all approved providers of residential aged care to report, on a quarterly basis, the total direct care staffing hours provided each day at each facility they conduct, specifying the different employment categories.
Note b: My Aged Care is a website maintained by the Australian Government that provides information about aged care services, eligibility assessments for aged care service types; referrals to service providers; and information about the cost of aged care.
Source: ANAO analysis of department records and the Federal Register of Legislation.
3.14 Overall, the department has largely implemented the government’s operational policy, legislative and IT requirements for the core, monitoring and compliance, and transparency requirements of mandatory care minutes. There were three minor exceptions in relation to the implementation of:
- the core requirement in terms of how the service-level targets for per resident per day care minutes are calculated;
- monitoring and compliance requirements for reporting at the facility level; and
- transparency requirements due to a 19-day delay in the deployment of IT systems.
Core requirement
3.15 In March 2022 the department designed a formula to set per resident per day care minute targets for each of 13 AN-ACC patient classes. The result of the formula is then used to calculate a case mix adjusted target for each residential aged care service (see paragraph 3.17 and Appendix 4). The department advised the ANAO that it designed the formula in early 2022 to allow the sector six months’ time to prepare for the changes, which were to be implemented on 1 October 2022.
3.16 If the formula is calibrated correctly, the average care minute target for the entire residential aged care sector should be very close to 200/40 minutes. In each quarter between July 2022 and June 2023, the average sector-wide care minute target fell short of 200/40 minutes by approximately two per cent (Table 3.3). The department advised the ANAO that the shortfall arose because the actual distribution of the residential aged care population across the 13 AN-ACC classes in July 2022 to June 2023 was different to the population distribution used to set the targets, which dated from March 2021 to January 2022.46 The department advised that the formula will be recalibrated by 1 October 2024 (when the minimum standard increases to 215/44).
Table 3.3: Sector-wide average per resident per day care minute targets, by quarter
|
Quarter |
Calculated care minute target (sector average) |
Calculated RN care minute target (sector average) |
|
July to September 2022 |
196.48 |
39.52 |
|
October to December 2022 |
195.56 |
39.39 |
|
January to March 2023 |
196.05 |
39.44 |
|
April to June 2023 |
197.59 |
39.62 |
|
July to September 2023 |
199.48 |
39.85 |
Source: ANAO analysis of departmental records.
3.17 In 2021 the department decided its approach would be that each service’s individual care minute target would be set by the Secretary of the department at the start of each quarter. When care minute targets were voluntary (i.e. prior to 1 October 2023), the Secretary used occupancy data from the preceding quarter to set the target for the following quarter (see Appendix 4). The use of the previous quarter’s residency data means that there is a risk that a service’s target for any given quarter does not accurately reflect the actual care needs of the service’s residents in that quarter. In the three quarters between July 2022 and March 2023, 42 per cent of care minute targets and 35 per cent of RN minute targets tested by the ANAO were below the actual care needs of residents (Figure 3.2 and Figure 3.3). Twelve targets set for care minutes and four targets set for RN minutes were 90 per cent or less of actual care needs, which is equivalent to 180/36 minutes per resident per day.47 Conversely, some targets exceeded requirements.
Figure 3.2: Ratio of service-level quarterly care minute targets to actual care needs, July 2022 to March 2023
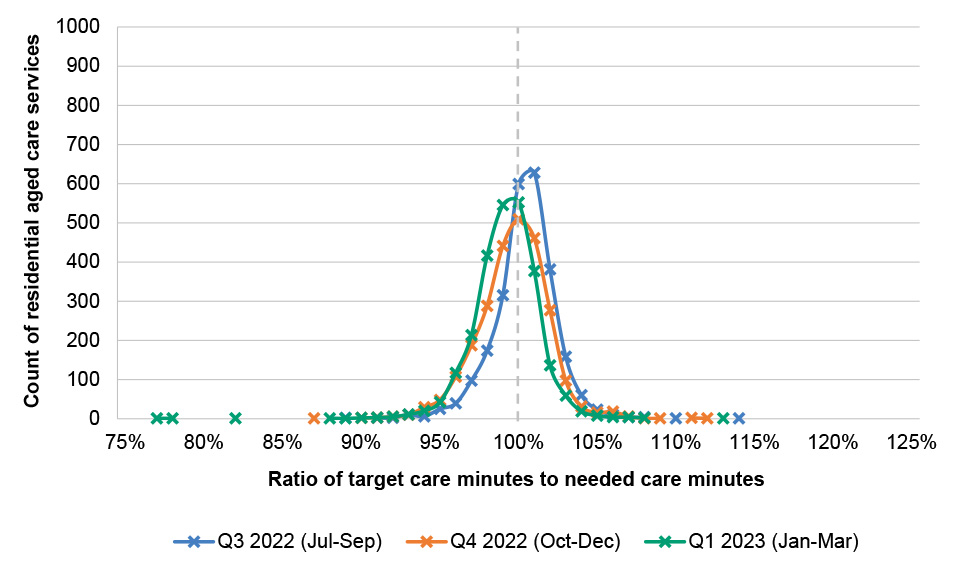
Note: Services in continuous operation between April 2022 to March 2023.
Source: ANAO analysis of departmental records.
Figure 3.3: Ratio of service-level quarterly registered nurse minute targets to actual care needs, July 2022 to March 2023
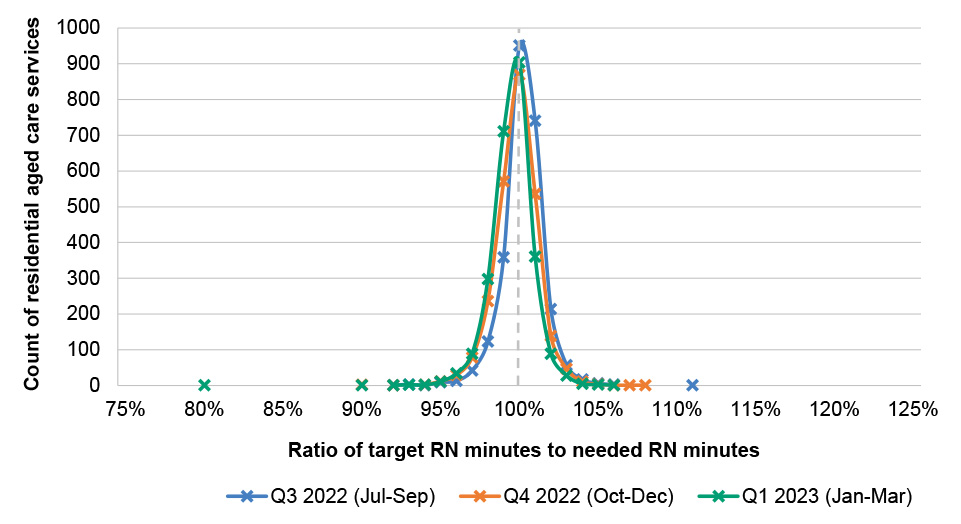
Note: Services in continuous operation between April 2022 to March 2023.
Source: ANAO analysis of departmental records.
3.18 In the course of drafting subordinate legislation in December 2022 (17 months after the operational policy for care minute targets was settled), the department identified that its preferred approach to calculating service-level targets may carry risks due to legal constraints, which would prevent mandatory targets from being calculated in the same manner as non-mandatory targets.48 The department advised the ANAO that from 1 October 2023 (when 200/40 care minutes became mandatory), targets would be calculated based on a three-month reference period (e.g. June to August 2023) and then advised to providers in the month prior (e.g. September 2023) to the relevant quarter (e.g. October to December 2023) commencing. The revised approach means that older historical data is used to calculate the target.
3.19 In November 2023 the department advised the ANAO that it had identified an IT issue which meant that an estimated four per cent of notifications relating to residents entering or exiting residential aged care had not been communicated to the department in the period October 2022 to October 2023. The consequence was that a source of data relied upon to calculate care minute and RN minute targets was not complete. The department advised that due to the incomplete data, care minute and RN minute targets for all services were inaccurately calculated between October 2022 and December 2023. The department provided a provisional analysis (shown in Figure 3.4 and Figure 3.5) which depicted the impact of the issue for targets in the quarter October to December 2023 (the first quarter in which care minute targets were mandatory).
Figure 3.4: Number of services affected by inaccurate care minute targets, October to December 2023
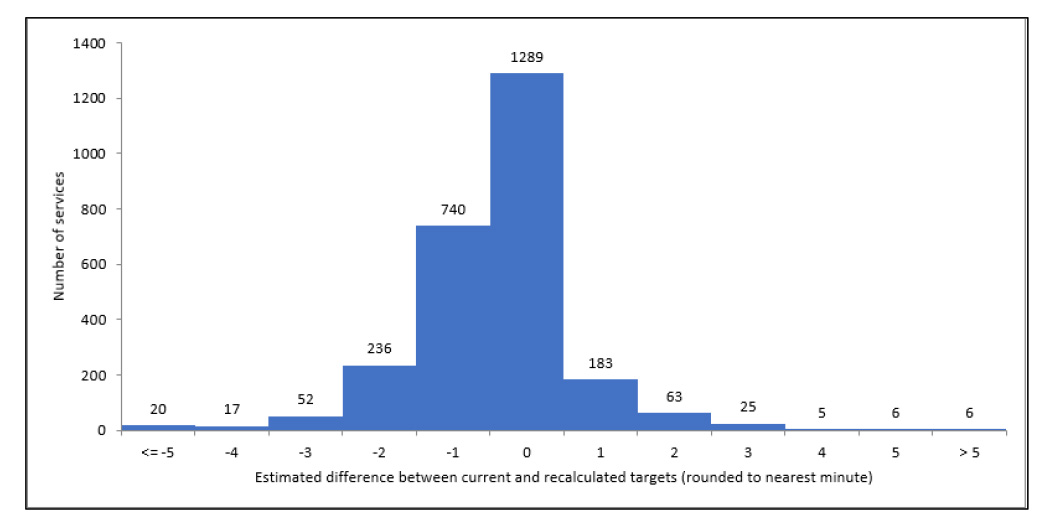
Source: Department of Health and Aged Care.
Figure 3.5: Number of services affected by inaccurate RN minute targets, October to December 2023
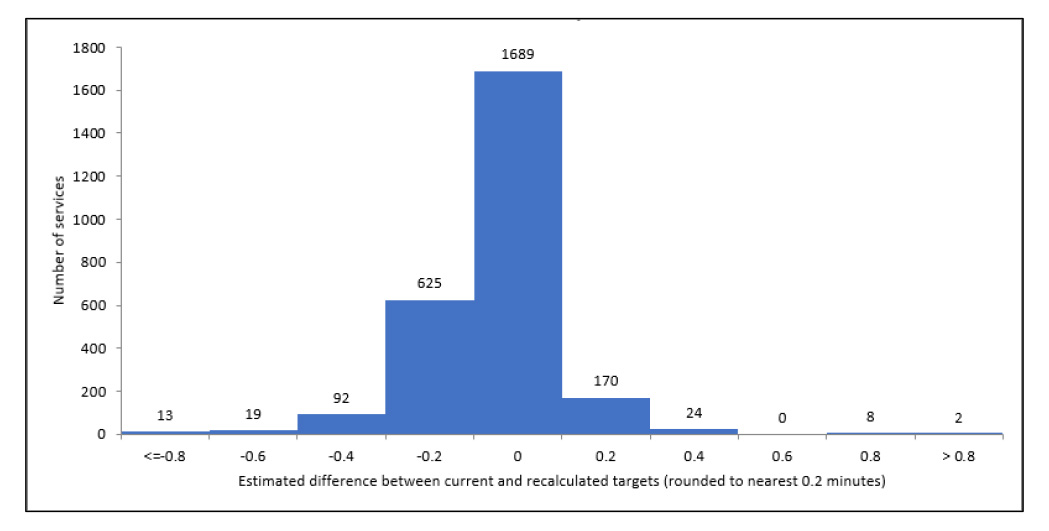
Source: Department of Health and Aged Care.
3.20 The department found, based on provisional analysis, that in each quarter between October 2022 to June 2023, between eight and 24 services had a staffing star rating affected by the issue, and between one and seven services had an overall star rating affected by the issue. The department advised the ANAO it was taking steps to fix the issue and remediate its impact on affected services, and that the department would identify and implement systems assurance controls to detect the issue in the future.
Monitoring and compliance
3.21 The Australian Government, acting with advice from the department, decided that reporting on care minutes should be at the facility level. In contrast to 24/7 RN (see paragraphs 3.5 to 3.8), however, the department imposed care minute reporting requirements on providers at the service rather than facility level. Although not fully conformant with the government’s requirements, the ANAO notes that this approach: avoids the 24/7 RN implementation issues for co-located and split facilities; and reduces regulatory burden on providers by aligning reporting with financial reporting obligations.
Transparency
3.22 The My Aged Care website publishes details of each mainstream service’s (i.e. excluding NATSIFAC and Multi-Purpose Service (MPS) providers) care minute targets and delivery. The website displays a ‘staffing rating’ of between one to five stars to indicate whether the service’s staffing level is satisfactory. The rating is assigned by the department based on a comparison of actual care minutes delivered by the service to the service’s target. The IT system to support this public reporting was deployed 19 days later than planned.
Mandatory care minutes in non-mainstream residential aged care services
3.23 Unlike mainstream services, the department did not implement minimum care minutes in MPS from 1 October 2023. MPS are not required to report care minutes delivered and no data appears on My Aged Care. The department advised the ANAO that MPS’ IT, payment and compliance systems are different to mainstream services and that it is consulting with Australian governments on how care minutes in MPS could be aligned to mainstream services in the future. The department advised that the funding allocated by the Australian Government to implement mandatory care minutes in MPS was not continued past 2022–23.
3.24 The program manual for NATSIFAC providers was amended in March 2023 such that, from 1 October 2023, NATSIFAC services would deliver a non-case mix adjusted target of 200/40 care minutes per resident per day.49 NATSIFAC services must report occupancy rates and the number of hours worked by RNs and other aged care staff in a six-monthly Service Activity Report, however this data is not reported on My Aged Care.
3.25 When deciding to introduce care minutes, the Australian Government allocated funding for the MPS and NATSIFAC programs in 2022–23 but did not indicate how the requirement should be applied to non-mainstream services (see paragraph 2.35), which are not subject to the AN-ACC funding model. The government’s response to Recommendations 52 and 55 of the Royal Commission (which dealt with the alignment of MPS and NATSIFAC programs to mainstream services) did not address care minutes. Given this, the ANAO has not assessed the effectiveness of the department’s implementation of care minutes in MPS and NATSIFAC services.
Were processes for exemptions from the requirement effective?
The department established an administrative process for 24/7 RN exemptions which met legislative requirements. To determine whether to grant an exemption, the department and ACQSC assessed clinical risk and alternative care arrangements. The assessment process that was followed experienced delays in decision-making. No exemption applications were approved prior to 1 July 2023, when the 24/7 RN requirement became mandatory. Exemptions were granted over subsequent months.
3.26 As discussed in Table 3.1, the Australian Government decided that small residential aged care facilities located in rural and remote areas would be eligible for a one-off exemption of up to 12 months from 24/7 RN, provided appropriate alternative care arrangements are in place.
Management of exemption applications
3.27 Exemptions may be granted by the Secretary of the department (or their delegate) in response to an application by an approved provider. In February and March 2023, the department identified and contacted 79 approved providers eligible to apply for an exemption. There were also sector-wide communications in April and May 2023 that any eligible provider could apply.
3.28 The department developed a standard operating procedure, templates and checklists for the exemption process. The standard operating procedure was consistent with the legislation that governed the granting of 24/7 RN exemptions prior to 1 July 2023. Exemption applications may only be approved if the provider has taken reasonable steps to ensure the clinical needs of residents will be met (‘alternative care arrangements’) while the exemption is in force. The legislation requires the Secretary or their delegate to have regard to certain information given by ACQSC in relation to the provider before deciding whether to grant an exemption. The standard operating procedure provides that once the department has received an application it will be referred to ACQSC so that ACQSC can advise the department about the applicant’s compliance history and the clinical risk to residents under the alternative care arrangements.
3.29 The department began accepting exemption applications from 1 April 2023, three months prior to the commencement of the 24/7 RN on 1 July 2023. The first applications were received in mid-April 2023 (Figure 3.6). By 30 June 2023 the department had received exemption applications for 50 facilities.50 No exemption applications were approved before 1 July 2023. On 30 June 2023: four had been presented to the delegate for consideration; 10 were complete51, however the information had not been collated for the delegate’s consideration; and 36 required further analysis. Half of the applications on hand at 30 June 2023 were submitted by providers to the department on 13 June 2023 or later.
Figure 3.6: 24/7 RN exemption applications, at 30 June 2023
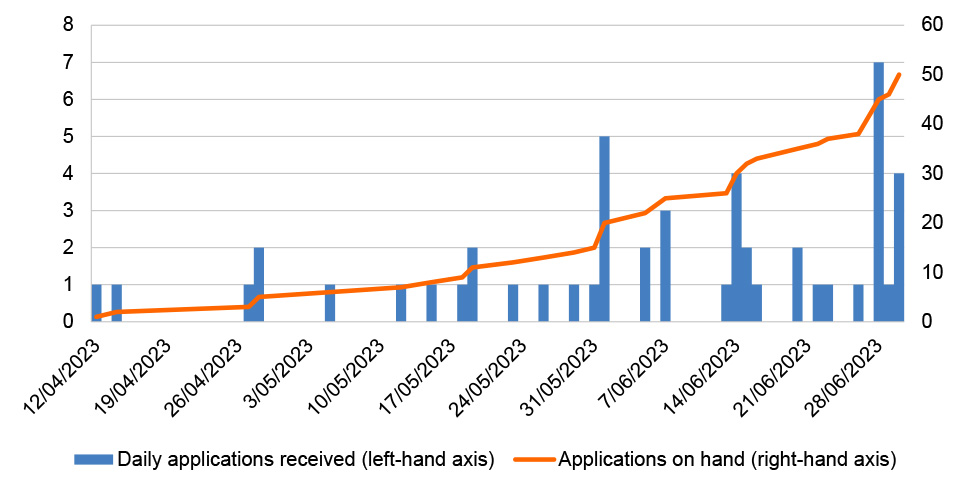
Source: ANAO analysis of departmental records.
3.30 On 23 June 2023 the department and ACQSC met to discuss issues with the referral process that were presenting difficulties in finalising applications. These issues included:
- delays in requesting and receiving additional information from applicants that was needed to inform ACQSC’s clinical risk assessment52; and
- ACQSC’s assessment of clinical risk being presented in a manner that did not meet the needs of the delegate.
|
Case study 1. Assessment of clinical risk by ACQSC – Provider A |
|
Provider A applied for a 24/7 RN exemption for one of its facilities on 24 May 2023. Details of the application were sent to ACQSC on the same day. On 7 June 2023 the departmental delegate received a briefing package recommending an exemption be granted. The package contained a letter from ACQSC stating that Provider A had not been subject to adverse regulatory activity and had been found in an accreditation audit conducted in the preceding month to have met all 42 requirements under the Aged Care Quality Standards. Over four pages, the letter detailed clinical factors to inform whether an exemption should be granted: the facility’s resident profile, shift coverage, on-call and on-attendance arrangements, workforce training and management, and alternative clinical care arrangements in the absence of an RN. The letter stated that each of the assessed clinical factors ‘neither increases or decreases’ the risk that the clinical care needs of the care recipients would not be met during the exemption period. On 16 June 2023 the delegate requested ACQSC clarify its assessment of clinical risk. On 26 and 30 June 2023 ACQSC provided revised letters which nominated which of the clinical factors decreased the risk that the clinical care needs of residents would not be met. The department granted the exemption on 31 July 2023. |
3.31 On 29 June 2023 the department briefed the AN-ACC and RACFR Board that it had raised a new high risk in the risk register for the 24/7 RN project that applications would not be in place by 1 July 2023 due to insufficient information being available for the delegate to decide whether to approve or reject the exemption.
3.32 On 30 June 2023, following consultation with ACQSC, the department sent a form email to applicants whose applications were still pending. The email stated: ACQSC would not take compliance action for a facility that was the subject of a pending exemption application; applicants were expected to have alternative arrangements in place from 1 July 2023 to meet the clinical needs of residents when an RN is not available; and delays in exemption processing were often attributable to providers not submitting sufficient information on alternative clinical care arrangements.
3.33 On 1 September 2023 the department published a list of 45 facilities that were granted exemptions between 26 July and 1 September 2023. For the 42 facilities that applied before 1 July 2023 and were granted exemptions, the time elapsed between submitting the application and the exemption taking effect ranged from 30 to 118 calendar days with an average time elapsed of 63 calendar days. Table 3.4 depicts the alternative care arrangements that the department assessed were satisfactory.
Table 3.4: Alternative care arrangements at exempted facilities, September 2023
|
Alternative care arrangements when an RN is not on site and on duty |
Percentage of 45 exempted facilities with these arrangements |
|
On-call arrangements with RNs |
100% |
|
On-call arrangements with general practitioners or other clinicians |
82% |
|
Access to clinical support via telehealth (including on-call arrangements with specialist telehealth services) |
71% |
|
Enrolled nurse (EN) or endorsed ENa on site and on duty (with on-call access to RNs or other clinicians) |
42% |
|
Access to RNs or clinicians in co-located or closely located health care or aged care services |
40% |
|
Support arrangements with local hospital |
13% |
|
Access to RNs who sleep overnight on-site |
2% |
Note a: Endorsed EN is a term used prior to 2010 to refer to ENs that can administer medicines. July 2023 guidance from the Nursing and Midwifery Board states ‘since 2010, there has been no such title as an ‘endorsed enrolled nurse’ and this title must not be used.’ See Nursing and Midwifery Board, Fact sheet: Enrolled nurses and medicines administration [Internet], Australian Health Practitioner Regulation Agency, July 2023, available from https://www.nursingmidwiferyboard.gov.au/Codes-Guidelines-Statements/FAQ/Enrolled-nurses-and-medicine-administration.aspx# [accessed 19 September 2023].
Source: ANAO analysis of departmental records.
3.34 The delegate refused three applications between 23 and 31 August 2023 because they were not satisfied that the provider had taken reasonable steps to ensure the clinical needs of residents would be met. All refused applicants were advised that the department would contact them to discuss the supports provided by the Australian Government to residential facilities.
3.35 The exemption process required applicants to demonstrate the clinical appropriateness of alternative care arrangements at the time of application and increased the likelihood that the applicant would be required to respond to compliance monitoring by ACQSC in the following 12 months (see Appendix 5). Exempted providers were still required to submit a monthly 24/7 RN compliance report, which is a more resource-intensive task for entities that have not provided 24/7 RN.53
3.36 Smaller providers that apply for an exemption do so in the knowledge it will make them ineligible for the 24/7 RN supplement. As noted in paragraph 3.11, on 24 May 2023 the department proposed a threshold of 20 hours per day of RN care for eligible providers to receive the 24/7 RN supplement. ACQSC’s regulatory approach provides for a ‘proportionate’ approach to regulating 24/7 RN. This means that ‘technical’ non-compliance with 24/7 RN alone would not be sufficient to trigger compliance activity; there must also be concern that the provider is not attempting to recruit and retain RNs or is not providing safe and quality care to residents. As a result, the accommodative regulatory approach to non-compliance with the 24/7 RN requirement is different to the high level of scrutiny applied to the exempted providers and applicants. The department advised the ANAO that the high level of scrutiny for exemption applications and exempted providers was required by the Aged Care Act.54
Are implementation governance arrangements fit for purpose?
The department’s project management of 24/7 RN and mandatory care minutes was consistent with the department’s project management framework, except that implementation plans were finalised five to seven months after project work had commenced. There are fit for purpose governance arrangements for coordination of the 24/7 RN and care minutes projects with other aged care reforms.
Project management
3.37 The department’s project management framework sets out the department’s requirements for project management, including procedures, tools and templates to support project delivery. The department initially established three projects (Table 3.5) to manage the response to Recommendation 86. In accordance with the project management framework, each project was recorded in a project reporting tool called ‘Health Tracker’, which is used to monitor progress and identify project delivery issues.
Table 3.5: 24/7 RN and care minutes projects
|
Project name |
Date record created |
Date record closed |
Description of project |
|
‘Care minutes’ |
1 June 2021 |
23 February 2023a |
Implementation of care minutes, including the online publication of care minutes provided, quarterly provider reporting requirements, and the introduction of mandated 200 care minutes per resident per day by October 2023. |
|
Increasing care minutes to 215 minutes per resident per day (‘Increasing care minutes’) |
1 July 2022 |
N/A |
Implementation of an increase in the minimum care minutes requirement, from 200 minutes per resident per day (including 40 minutes provided by an RN) (200/40) to 215 minutes per day (including 44 minutes by an RN) (215/44). |
|
Registered nurses onsite 24/7 (‘24/7 RN’) |
26 October 2022 |
N/A |
Implementation of all changes for the 24/7 RN requirement, including transitional exemption arrangements and public reporting through star ratings. |
Note a: The mandated 200 care minutes component of this project was moved to the ‘Increasing care minutes to 215 minutes per resident per day’ project.
Source: ANAO, based on departmental records.
3.38 A project manager was appointed to the projects and the RACFR project management office was responsible for maintaining project documentation. The project management framework requires a Senior Responsible Officer (SRO) be accountable for each project. The First Assistant Secretary of the Home and Residential Division within the Ageing and Aged Care Group was appointed as the SRO for all three projects. Oversight of the projects was provided by a governance board (the AN-ACC and RACFR Board) chaired by the SRO.
3.39 Between May 2022 (when the AN-ACC and RACFR Board assumed responsibility for the ‘increasing care minutes’ and ‘24/7 RN’ projects) and June 2023, the Board met twelve times and considered updates on the new workforce measures at each meeting since August 2022. Activities undertaken by the AN-ACC and RACFR Board included:
- agreeing to key policy decisions, such as thresholds for the 24/7 RN supplement;
- noting emerging risks and issues, including concerns from stakeholders that providers may reduce EN staffing to meet 24/7 RN and care minute requirements; and
- endorsing a report that assessed the readiness of the 24/7 RN IT deployment to launch on 3 July 2023.
3.40 The project management framework requires a documented project plan to be approved at project commencement. Work on the ‘increasing care minutes’ and ‘24/7 RN’ projects commenced in July 2022. Project management plans were approved after the work had commenced. Project management plans were approved by the AN-ACC and RACFR Board on 23 February 2023, although an abbreviated planning document (termed a Plan on a Page) with substantially similar information was noted by the Board on 5 December 2022 for the 24/7 RN project.
3.41 The department documented project benefits, risks and stakeholder engagement in a manner consistent with the requirements of the project management framework.
Coordination with other aged care reforms
3.42 The response to Recommendation 86 is part of the Aged Care Transformation Program (ACTP), which was established by the department to coordinate the implementation of the Royal Commission’s recommendations. Recommendation 147 of the Royal Commission was that the department establish a taskforce to implement the Royal Commission’s recommendations, supported by a cross-department Deputy Secretary-level steering committee. The ACTP is governed by a steering committee, which met 23 times between 26 May 2021 and 23 June 2023.55 The ACTP Steering Committee is supported by the ACTP program management office, which coordinates all projects under the ACTP.
Figure 3.7: Governance arrangements for 24/7 RN and care minutes, at 28 April 2023
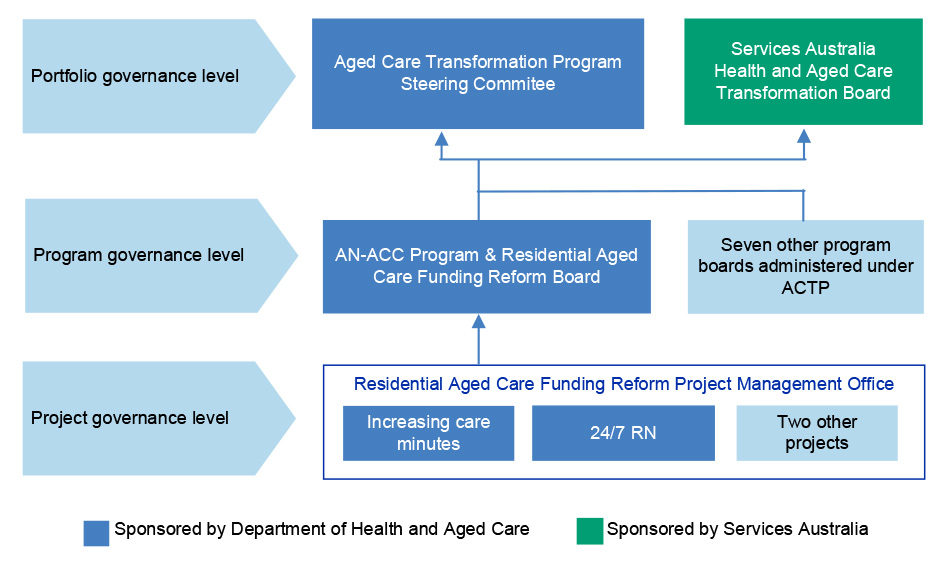
Note: The two other projects governed by the AN-ACC and RACFR Board were the introduction of the AN-ACC funding model and the Independent Health and Aged Care Pricing Authority.
Source: ANAO, based on departmental records.
3.43 The AN-ACC and RACFR Board reports to the ACTP Steering Committee monthly. Project updates communicated to the ACTP Steering Committee by the AN-ACC and RACFR Board included overdue milestones for the 24/7 RN project and the successful passing of subordinate legislation.
3.44 A Master Plan was first developed by the department in July 2021 to achieve consistency and coordination across ACTP projects. The Master Plan outlines the governance and reporting arrangements at the portfolio (ACTP), program (AN-ACC and RACFR Board), and project (24/7 RN and care minutes) levels. This governance arrangement was followed and documented in the project management plans for the ’increasing care minutes’ and ‘24/7 RN’ projects.
3.45 The ‘increasing care minutes’ and ‘24/7 RN’ projects have interdependencies with ACTP projects that are not governed by the AN-ACC and RACFR Board. The department uses an integrated schedule to monitor and coordinate ACTP projects, and to track progress and milestone dependencies. Risks identified as critical or high-risk in the AN-ACC and RACFR program integrated risk register (see paragraph 3.41) are also monitored by the ACTP Steering Committee.
3.46 The ACTP Steering Committee includes members from Services Australia and ACQSC, to facilitate coordination with projects within these entities that correspond with the department’s work. The department is represented in an equivalent governance body at Services Australia.
4. Preparing to regulate
Areas examined
This chapter examines whether the aged care regulatory system, as administered by the Department of Health and Aged Care (the department) and the Aged Care Quality and Safety Commission (ACQSC), was prepared for the commencement of the mandatory care minutes and 24/7 registered nurse (RN) requirements.
Conclusion
The department and ACQSC were largely prepared to monitor and enforce compliance with 24/7 RN and mandatory care minutes. Both entities defined their respective roles and responsibilities, consulted with stakeholders, and received funding for regulatory activities. After initial delays, both entities finalised operational plans for regulatory activities. Both entities had commenced but not completed updating procedural guidance and training staff as at October 2023. The department has performance measures in place but there is no evaluation plan. ACQSC has not planned how it will measure regulatory impact.
Areas for improvement
The ANAO made two recommendations to ACQSC aimed at improving the documentation of intelligence production processes and measuring performance. The ANAO made one suggestion to the department to seek an update to the department’s regulatory Statement of Intent.
4.1 ACQSC’s regulatory operating model56 comprises five components: engagement and communication about risk; using data and intelligence to understand risks and providers; planning regulatory operations; delivering regulatory operations; and understanding regulatory impact and outcomes. The ANAO examined the department’s and ACQSC’s preparedness for mandatory care minutes and 24/7 RN (see paragraph 1.9 for a description of these measures) across these five components.
4.2 The ANAO also examined whether roles and responsibilities for regulating mandatory care minutes and 24/7 RN are clear, as previous independent reviews of aged care regulation have found that indistinct, duplicative or inappropriate allocation of roles and responsibilities between the department and the regulator have reduced the effectiveness of aged care quality and safety regulation.57 The Department of Finance has stated that regulators should establish clear operational scopes and minimise duplication.58
Are roles and responsibilities clear?
The department and ACQSC’s respective roles and responsibilities for regulating compliance with 24/7 RN and care minutes have been clearly defined and communicated to stakeholders. The department was funded for a compliance role that exceeds its current statutory powers under the Aged Care Act 1997. The department is developing new legislation and an updated memorandum of understanding with ACQSC.
4.3 Following consultation with the department, on 13 April 2023 ACQSC published a regulatory bulletin on mandatory care minutes and 24/7 RN. The bulletin provided a clear definition of the respective regulatory roles and responsibilities of the two entities (Table 4.1).
Table 4.1: Regulatory roles and responsibilities for care minutes and 24/7 RN
|
Department of Health and Aged Care |
Aged Care Quality and Safety Commission |
|
|
Source: ACQSC, Workforce-related responsibilities – including 24/7 registered nurse and care minutes, available at https://www.agedcarequality.gov.au/resources/rb-2023-19-workforce-related-responsibilities [accessed 5 July 2023].
4.4 The roles and responsibilities set out in the bulletin are consistent with the statutory powers of the department and ACQSC under the Aged Care Act 1997 (Aged Care Act) and the Aged Care Quality and Safety Commission Act 2018 (ACQSC Act), except for the department conducting a program of audits of provider compliance reporting.
- The Aged Care Legislation Amendment (New Commissioner Functions) Act 2019 (New Commissioner Functions Act) assigned ACQSC the function of ensuring provider compliance with the Aged Care Act and ACQSC Act. The explanatory memorandum stated that the intent was to centralise regulatory functions and powers within a single regulator to address the fragmentation and silos identified in the Review of National Aged Care Quality Regulatory Processes. The New Commissioner Functions Act also conferred statutory powers on ACQSC to monitor, investigate and enforce compliance with Chapter 4 of the Aged Care Act (which sets out the responsibilities of approved providers, including the requirement to report 24/7 RN and care minute data). These powers include monitoring whether information given by providers is correct.
- The department has statutory powers under the Aged Care Act to verify the accuracy or data quality of providers’ monthly compliance reports and quarterly financial reports (QFRs). The principal power is that the Secretary may issue a notice requiring a provider to provide further information.59 The Aged Care Act does not give the department powers relating to entry and search, monitoring and investigation, requiring persons to attend a place and answer questions, or issuing sanctions.
- Under the terms of a 2019 memorandum of understanding (MOU) between the department and ACQSC, the department can refer suspected provider non-compliance with Chapter 4 of the Aged Care Act to ACQSC. As at October 2023 the department and ACQSC were developing an updated MOU that will provide greater detail on how regulatory cooperation including referrals of suspected non-compliance will occur. The MOU is meant to be finalised by June 2024.
4.5 The department advised the Australian Government in October 2022 that in addition to desk-based verification activities that are within its existing legal powers, it would conduct a program of ‘more intensive, forensic on-site audits in higher risk residential aged care facilities’ to check the accuracy of reported care minute and 24/7 RN information. The department advised that current legislation ‘does not provide the legal power necessary’ for the new activities, and that primary legislation would be required to empower the department. The advice did not present alternative options for consideration, such as ACQSC undertaking on-site activities using its existing legal powers for higher risk providers referred by the department. Despite the advised legal limitation, the department commenced plans in August 2022 for developing an audit function that would undertake on-site audits (see paragraph 4.27). Departmental documentation stated the rationale for establishing a program to ‘monitor provider compliance with legislated requirements to deliver appropriate care minutes and 24/7 [RN] coverage’ was to maintain the integrity of Commonwealth subsidies and ensure the accuracy of information reported on My Aged Care.
4.6 The department examined options to address the gap between its statutory powers and its contemplated audit function.
- From December 2022 the department and ACQSC examined whether it is possible to delegate powers of the Aged Care Quality and Safety Commissioner (the Commissioner) to departmental officers60 — in particular, to empower officials to impose sanctions on providers. ACQSC advised the department on 23 July 2023 that it did not support the delegation of these powers.
- In February and March 2023 the department developed drafting instructions for a new Aged Care Act which proposed that the department have comparable monitoring and enforcement powers to ACQSC, for the purposes of program assurance and safeguarding the integrity of aged care payments.
4.7 ACQSC identifies and follows up providers that have not submitted QFRs or fulfilled other financial reporting responsibilities under Chapter 4 of the Aged Care Act. The department advised the ANAO on 6 September 2023 that these activities are largely oriented towards monitoring the governance of services and financial viability, which contrasts with the department’s responsibility to obtain assurance over data used to monitor whether funding from the Australian Government was used correctly.
4.8 The Aged Care Quality and Safety Commissioner issued a Statement of Intent on 2 December 2022 which set out its approach to regulating the aged care sector. The Secretary of the department issued a regulator Statement of Intent on 21 July 2023, which identified six regulatory functions undertaken by the department.61 None of the six functions encompass the department’s current program of activities to verify aged care provider reporting or any other activities in relation to the aged care sector.
|
Opportunity for improvement |
|
4.9 The department could seek to update its regulatory Statement of Intent to address departmental regulatory functions in relation to aged care providers. An update could be made in relation to the department’s current program of activities to verify provider reporting. A further update could be made if new activities (such as on-site audits) result from changes to aged care legislation. An updated Statement of Intent could address how departmental regulatory functions in relation to the aged care sector are differentiated from functions of ACQSC. |
Has there been appropriate stakeholder engagement?
The department and ACQSC communicated with aged care providers using consultative forums, websites, webinars and newsletters. There were some targeted communications to providers at higher risk of non-compliance with the 24/7 RN requirement. There was limited engagement with consumer peak bodies through consultative forums. Engagement with state and territory regulators on mandatory care minutes and 24/7 RN proceeded in line with the lower priority that state and territory regulators placed on these measures compared to other aged care reforms.
4.10 The ANAO assessed stakeholder engagement against the department’s internal stakeholder engagement framework and Department of Finance guidance concerning regulatory engagement (Resource Management Guide 128: Regulator Performance).
Consultative forums
4.11 The department and ACQSC used two consultative forums as a mechanism to engage with key providers, consumer peak bodies and other stakeholders about mandatory care minutes and 24/7 RN prior to their introduction.62
- Residential Aged Care Funding Reform Working Group (RACFRWG) — as discussed in paragraph 2.32, the department convened the RACFRWG to get feedback on how the new measures could be implemented and to understand risks and challenges to implementation. The membership of RACFRWG comprised peak bodies representing aged care providers and medical professions, aged care consumer advocacy groups and academia. The department maintained meeting agenda and discussion papers but did not keep minutes. Based on agenda and meeting papers, the ANAO determined that RACFRWG met nine times between August 2021 and March 2023 and each of the nine meetings was used to discuss aspects of the implementation of care minutes or 24/7 RN. Members were also invited to provide feedback on the measures out-of-session.
- Consultative Forum — ACQSC established a standing quarterly Consultative Forum in 2019 with the aim of discussing emerging issues and gathering feedback from key stakeholders in the aged care sector about ACQSC’s approach. The Consultative Forum comprises the department and national consumer and provider peak bodies including the Aged Care Industry Association, Dementia Australia, National Aboriginal Community Controlled Health Organisation and Older Persons Advocacy Network. The Consultative Forum discussed mandatory care minutes and 24/7 RN at two meetings (1 July 2022 and 31 March 2023). At these meetings, ACQSC explained its regulatory expectations and stakeholders were invited to give feedback (including on perceived barriers to compliance or potential unintended consequences of the new requirements).
4.12 ACQSC established a Consumers and Families Panel in July 2022 made up of residential and home care consumers, their carers or family members and senior Australians who are considering using aged care services in the future. The Consumers and Families Panel states that it holds activities around three times per year, however it was not used to discuss mandatory care minutes or 24/7 RN as at July 2023.
Communications activities
4.13 The department and ACQSC settled a joint communications plan in February 2023. The focus of the joint communications plan was on supporting implementation of minimum care minutes and 24/7 RN, including the 24/7 RN supplement and exemption. The joint communications plan identified activities such as webinars, newsletters, and website updates.63 Of 28 activities scheduled to occur prior to 1 July 2023, 24 targeted providers only, one targeted providers and consumers, and three targeted internal stakeholders. Most (21 of 28) were conducted in accordance or largely in accordance with the plan.
4.14 ACQSC established a media plan in April 2023 to support the implementation of 24/7 RN. The plan was to address six key themes including the benefits of 24/7 nursing, concerns that 24/7 RN would lead to service closures, challenges faced by rural and remote services, and how the 24/7 exemption would work. Nine activities were to be conducted prior to 1 July 2023, comprising two targeted at providers and seven targeted at consumers, their families, and the public. Three of the nine activities were conducted in accordance with the media plan.
4.15 Between April and June 2023 the department planned to email or phone 547 aged care services who were ineligible for an exemption and whose reported delivery of RN minutes between October to December 2022 suggested a potential gap in RN care provision of six and a half or more hours per day. On 29 June 2023 the AN-ACC and RACFR Board (see paragraph 3.38) was told that 361 services (66 per cent of the targeted services) had been contacted by 15 June 2023. The Board was told that the department was also planning to contact approximately 350 services that had not yet logged into the IT system through which 24/7 RN monthly compliance reports were to be submitted by 7 August 2023. On 3 August 2023 the department called 45 out of 54 services that were yet to log in or commence a 24/7 RN compliance report as at that date.
Engagement with other regulators
4.16 The department convened an intergovernmental Senior Officials Group with state and territory governments in February 2022 to coordinate the implementation of recommendations from the Royal Commission into Aged Care Quality and Safety (the Royal Commission). The Senior Officials Group determined which Royal Commission recommendations were a high priority requiring action in the Senior Officials Group forward workplan. In May 2023, the response to Recommendation 86 was listed as a low to medium priority in the workplan. The Senior Officials Group agreed that a working group should be formed to examine reforms to the Multi-Purpose Services (MPS) program, including how 24/7 RN and mandatory care minutes could be applied to MPS. ACQSC’s engagement with other regulators prioritised other aged care reforms such as the serious incident reporting scheme64 and a code of conduct for aged care workers.65
Submissions to the audit
4.17 The ANAO invited submissions to the audit from eight state and territory governments and 20 stakeholders (aged care peak bodies and providers, medical peak bodies, consumer advocacy groups and unions) with a history of participating in departmental or Parliamentary consideration of aged care reforms. Five of the nine submissions received by the ANAO commented on the department’s or ACQSC’s engagement with them.
- Two providers and one state government expressed satisfaction at the level of engagement but suggested that guidance and support provided by the department or ACQSC could be improved (more detailed or less prolific, clearer, or more timely).
- One union expressed satisfaction with its engagement with the department but noted it had no engagement with ACQSC.
- One consumer peak body expressed dissatisfaction with the department’s choice of consumer representatives on consultative forums. The peak body stated that while it is impossible to include every consumer representative on advisory bodies, ‘failure to embed broad consumer representation has hindered quality improvements’.
Does regulatory intelligence incorporate the new requirements?
The department and ACQSC have updated systems to incorporate care minute and 24/7 RN data into regulatory intelligence production. There are plans to increase analytic capability for risk profiling of providers in relation to mandatory care minute and 24/7 RN non-compliance. ACQSC’s processes for producing and disseminating regulatory intelligence analysis were insufficiently documented.
4.18 The department and ACQSC jointly maintain the Risk Based Targeting, Information Sharing system (RBTIS) (Figure 4.1). RBTIS relies on an enterprise data warehouse maintained by the department, which integrates residential aged care provider and service data. RBTIS users draw upon this data for ad hoc data analysis, automated provider risk profiling, and task-specific interactive dashboards.
Figure 4.1: Risk Based Targeting, Information Sharing system
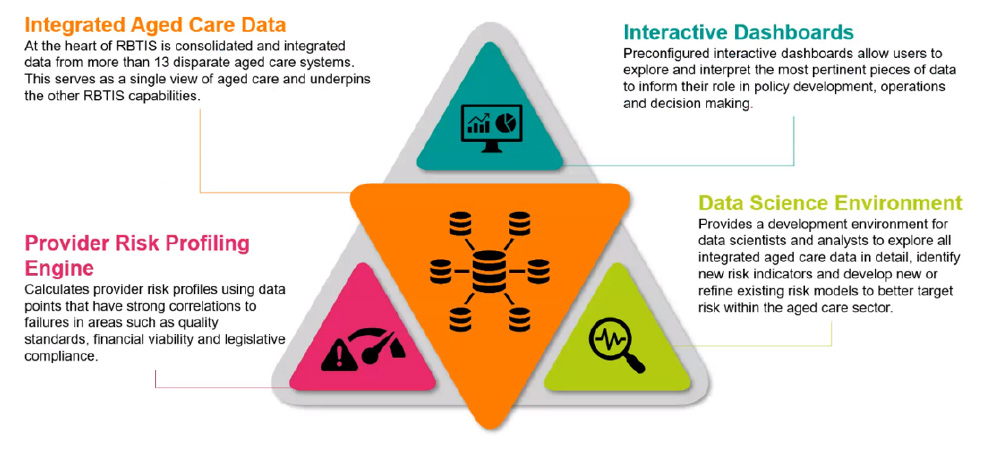
Source: Department of Health and Aged Care.
4.19 The data warehouse has been updated to ingest provider reports of care minutes provided (as reported in QFRs), 24/7 RN compliance data, and service-level care minute targets. The 24/7 RN compliance data is recorded against services rather than facilities because RBTIS is not designed to target facilities (see paragraphs 3.5 to 3.8). The department and ACQSC use an agreed service-to-facility mapping approach to support manual analysis at a facility level. Interactive dashboards have been created that display care minute and 24/7 RN compliance data.
4.20 Both entities have used RBTIS and the data warehouse to inform regulatory activity in relation to 24/7 RN and care minutes. ACQSC used RBTIS to analyse the compliance history of an applicant for a 24/7 RN exemption. The department used data from the data warehouse to conduct an initial round of risk-based targeting for its verification activities (see paragraph 4.5 and Case Study 2).
|
Case study 2. Use of Audit Site Development Tool in quarter 1, 2023–24 |
|
In planning required resources for a care minutes audit function, the department assumed that 755 facilities would be targeted for audit each year from 1 July 2023 to 30 June 2026, of which 680 (90 per cent) would be targeted on a risk-basis and 75 (10 per cent) would be selected at random to benchmark the effectiveness of the targeting strategy. The department stated that this would enable auditing of 28 per cent of all facilities each year. The department developed the Audit Site Development Tool to assign relative risk levels to residential aged care services to support risk-based targeting, and also to generate an unbiased sample of services on a randomised basis. The risk-based targeting aimed to identify services that reported unusually high or low expenses for RNs and care workers, and unusually high RN or total care minutes provided relative to the service’s RN or total care minutes target. The department used the tool to select 450 services for verification activities in the July to September 2023 quarter, of which 45 services (10 per cent) were targeted on the basis of a risk assessment. Internal correspondence stated the proportion of services targeted on a risk (as opposed to randomised) basis in the July to September quarter was temporarily set low while business processes were still being established to support the department in measuring the accuracy of the targeting model prior to its broader application. The department subsequently incorporated this targeting approach as one component of a broader risk model in its audit methodology (see paragraph 4.29). |
4.21 ACQSC planned to produce an internal monthly intelligence report which would rank services with reported gaps in RN coverage. The ranking would take into account actual care minutes reported in providers’ QFRs and indicators of risk such as previous non-compliance, serious incident reporting relating to neglect or significant harm, or poor resident experience survey data. ACQSC also planned to conduct risk profiling. Additional funding was secured to recruit a data scientist in 2023–24 for this purpose. ACQSC commenced risk profiling work in August 2023 and advised the ANAO that the development of further risk profiles would require more reporting data.
4.22 The ANAO sought to test whether ACQSC’s standard operating procedures for preparing and disseminating intelligence briefs were updated to accommodate mandatory care minutes and 24/7 RN. ACQSC intelligence staff advised the ANAO in May 2023 that the procedures were largely undocumented. In August 2023 ACQSC provided the ANAO a guidance template created in October 2022 which contained a statement that QFRs are a source of information on staffing arrangements and which had not since been updated. In November 2023 ACQSC provided the ANAO standard operating procedures on preparing intelligence briefs (which contained reference to care minutes and 24/7 RN and two supporting work instructions) and on updating the 24/7 RN risk profiling model, both of which had been finalised in November 2023.
Recommendation no.3
4.23 The Aged Care Quality and Safety Commission improve its documentation of processes for preparing and disseminating intelligence briefs.
Aged Care Quality and Safety Commission response: Agreed.
4.24 The Commission has finalised the Standard Operating Procedure (SOP) and Work Instructions for the preparation and dissemination of intelligence briefs. This SOP includes reference to the use of Care Minutes (CM) and 24/7 Registered Nursing (RN) data and information in intelligence briefs, where relevant.
4.25 Additionally, the Commission has finalised the SOP for risk profiling of workforce risks (Care Minutes and 24/7 Registered Nursing).
4.26 The Commission has recently developed a Data and Intelligence Capability Framework which outlines the capability requirements (People, Process, Technology) required for the use of data and intelligence in decision making within the Commission. This will include the collection, analysis and dissemination of intelligence. This framework identified the need to update and develop Data and Intelligence policies and processes, with related work currently underway and to be completed by March 2024.
Does operational planning incorporate the new requirements?
The entities received additional funding to resource regulatory activities. The department and ACQSC’s compliance plans for mandatory care minutes and 24/7 RN were not finalised by 1 July 2023, the date on which both entities had planned to be ready to conduct regulatory activities. ACQSC commenced regulatory activity on 4 July 2023 and finalised its regulatory approach on 22 July 2023. The absence of legal authority for aspects of the department’s contemplated audit function impeded development of the department’s operational plans. The department finalised its plan on 27 September 2023.
Department of Health and Aged Care
4.27 In October 2022 the department sought $22.7 million over four years to establish an audit function for care minutes and 24/7 RN provider reporting. The department’s proposal included engaging a consultancy firm to develop an audit methodology and deliver training, recruiting 33 staff, and establishing a bespoke customer relationship database and specialist auditing software. The Australian Government approved $7.4 million terminating on 31 December 2023, and requested the department come back on the longer-term approach for the program assurance role.
4.28 Through a November 2022 procurement process, the department contracted EY to develop and deliver the audit methodology, a pilot activity to test the methodology, and training for staff by 30 June 2023. The department also planned for the recruitment of staff to be completed by 30 June 2023, so that audit activity could commence for care minutes from 1 July 2023, and for 24/7 RN from mid-August 2023. The department planned to deploy an IT solution to support booking audits, uploading audit findings and viewing provider data by 9 October 2023.
4.29 The EY contract deliverables were not finalised by 30 June 2023, mainly because of an absence of legal authority for the department’s proposed program of audits (see paragraph 4.5).
- On 12 May 2023 EY delivered a draft methodology. In accordance with the department’s instructions, the draft methodology presumed that the department’s statutory powers had already been expanded by the passage of a new Aged Care Act and did not make provision for the department to apply the methodology in the absence of these powers.
- The pilot was to be delivered between 22 May 2023 and 9 June 2023 but was delayed. The department confirmed in May 2023 that there was no legislative basis for undertaking the pilot audit activity, and the activity could only be undertaken to the extent that participating providers consented to it. Planning for the pilot activity resumed by 16 June 2023, however the pilot was to be undertaken under different conditions, where there would be no consequences for non-compliant providers.
- A 29 June 2023 contract variation extended the deadlines for the final EY deliverables. On 31 August 2023 EY submitted the final methodology which set out a program of activities that was largely the same as was provided in the draft methodology, while acknowledging that the new Aged Care Act to support the auditing function was yet to be implemented. EY reported to the department that the pilot was ‘reduced’ to being a practical walkthrough of the care minute reporting methodology with a single provider due to several challenges including legal limitations and a lack of provider responsiveness.
4.30 The department revised the final methodology delivered by EY to omit activities that would require powers under a new Aged Care Act, and to clarify that the department’s role was limited to verifying the accuracy of provider data using existing statutory powers. On 27 September 2023 the AN-ACC and RACFR Board approved the revised version of the methodology.
4.31 By 1 July 2023 recruitment for the audit function was not complete and the department had not confirmed a deployment date for its proposed IT solution. Although the audit methodology, recruitment and supporting IT systems had not been finalised by 30 June 2023, the department identified 526 services that it planned to be subject to verification activities between July to September 2023. The department advised the ANAO that verification activities commenced on 28 September 2023 and as at 24 November 2023 none had been completed.
Aged Care Quality and Safety Commission
4.32 In March 2023 ACQSC received $3.2 million in additional funding to resource regulatory activities for mandatory care minutes and 24/7 RN in 2023–24. The funding request was based on estimates of the number and type of regulatory activities that would need to be undertaken for the new measures as well as the predicted impact of the new measures on business as usual functions such as complaints handling, clinical advice, legal advice, operational policy, performance reporting and communications.
4.33 On 22 July 2023 ACQSC finalised a ‘regulatory approach’ containing a three-phase plan that aimed to ‘deliver a tiered, risk-based response model to potential non-compliance’ with mandatory care minutes and 24/7 RN during 2023–24 (see Appendix 5). Regulatory action (phase three) was planned to commence in July 2023. Under phase three, aged care services were divided into three tranches depending on their risk profile. The regulatory approach provided for 495 desk-based monitoring contacts and 198 one-day site visits that would monitor alternative clinical care arrangements in place (at facilities exempted from 24/7 RN), assess the sufficiency of provider efforts to comply with 24/7 RN, determine if there were any unmanaged risks to consumers, and determine whether there was any non-compliance with the Quality Standards.66 The regulatory approach assumed that approximately 30 to 40 services would require escalation to a full on-site review against the Quality Standards. The regulatory approach stated that ACQSC had overestimated the number of exempted services that would require monitoring, and would seek to redeploy excess resources to support the desk-based monitoring contacts and one-day site visits. ACQSC advised the ANAO that activities under phase three of the regulatory approach commenced on 4 July 2023, as planned, and that as at 17 October 2023, 17 desk-based and 20 on-site monitoring activities had been conducted.
Have procedures been adapted for the new requirements?
Guidance materials and standard operating procedures for monitoring and enforcing compliance with the new requirements were being developed but were largely not finalised as at 1 July 2023. Both entities had finalised certain guidance materials and had delivered some training by September 2023.
Department of Health and Aged Care
4.34 EY was commissioned to develop procedural guidance and training materials for the new audit function by 30 June 2023. EY submitted a draft procedural guidance document and a draft training pack to the department on 23 May 2023. The covering letter stated that a limitation of the materials was that they relied on drafting instructions provided by the department for a new Aged Care Act rather than existing legislation. The covering letter noted that the material would be amended in response to any learnings from the pilot activity that was originally scheduled for May 2023 but was postponed to June and July 2023. In accordance with a variation to the contract, EY delivered finalised guidance and training materials to the department on 31 August 2023. The final training and guidance materials were based on a version of the department’s audit methodology (see paragraph 4.29) which did not address the legal basis for these activities prior to the introduction of a new Aged Care Act. The department advised the ANAO that the materials were used to deliver training on 30 August 2023 with the omission of content regarding on-site audit activity.
4.35 Separate to the EY contract, the department developed practices, procedures and training materials for the processing of 24/7 RN exemption applications (see paragraph 3.28). These were largely finalised by 8 May 2023 and fully completed by 4 July 2023.
Aged Care Quality and Safety Commission
4.36 The ACQSC regulatory approach indicated that ACQSC planned to create training materials and procedural guidance to assist quality assessors to deliver the first tranche of a targeted monitoring program, which was to commence in July 2023 (see Appendix 5). The proposed materials included work instructions to guide the collection and assessment of 24/7 RN compliance information and quick reference materials about 24/7 RN for complaints officers. The regulatory approach did not propose changes to October 2022 policy and procedures that governed compliance management of the Quarterly Financial Report requirement. The regulatory approach set an indefinite deadline for developing the new materials that fell between July and October 2023.
4.37 A work instruction for quality assessors was finalised on 31 August 2023. ACQSC advised the ANAO that as at September 2023, 221 staff had completed training on the work instruction. As at October 2023 a number of training materials were still being finalised, including: an eLearning module on 24/7 RN aimed at all staff within ACQSC; tailored factsheets and frequently asked questions; and tailored learning for complaints and customer contact centre staff.
4.38 A standard operating procedure for case coordination and monitoring for first tranche entities was prepared in August 2023. The procedure provided tailored instructions for each of the three cohorts identified in the first tranche of the regulatory approach (services refused a 24/7 RN exemption, non-exempted services demonstrating high-risk indicators, and services with indicators of high clinical risk that did not apply for an exemption).
4.39 Separate to training and materials provided under the regulatory approach, ACQSC had earlier developed practices, procedures and training for the provision of information to the department in relation to 24/7 RN exemption applications.
Is there a plan to monitor regulatory impact and outcomes?
The department has an external performance measure for care minutes and 24/7 RN, which it monitors. The department does not have an overarching evaluation strategy to examine the impact on residential aged care quality. ACQSC’s regulatory approach acknowledges the need to measure regulatory impact, however as at October 2023, it had no detailed plans to do so.
4.40 The department has four outcomes in the Australian Government’s 2023–24 Portfolio Budget Statements, and ACQSC67 has one outcome. Three programs contribute to the department’s Outcome 3 (Ageing and Aged Care)68: Program 3.1 Access and Information, Program 3.2 Aged Care Services, and Program 3.3 Aged Care Quality.
Department of Health and Aged Care
4.41 In September 2022 the department engaged Synergy Group to review the department’s performance measures for the Ageing and Aged Care Group and suggest improvements to better align performance measures to aged care reforms. Synergy Group made recommendations in February 2023 which included that performance measures for care minutes and 24/7 RN be placed under Program 3.3 (Aged Care Quality), which is linked to ACQSC’s Outcome 1.
4.42 The department commissioned Synergy Group again in March 2023 to develop performance plans for all three programs under Outcome 3. Later that month, Synergy Group delivered draft performance plans including performance measures, logic maps and proposed processes to collect and assure data that would be used to report on performance. By the time Synergy Group delivered its logic maps, the department had already decided to map care minutes and 24/7 RN to Program 3.2 (Aged Care Services) rather than Program 3.3.69 This decision was taken because the department identified a need to have quantitative measures of performance for residential aged care funding (which falls under Aged Care Services), in recognition that it represents over $20 billion in funding.
4.43 The 2023–24 Portfolio Budget Statements identified care minutes provided and 24/7 RN compliance rates as a departmental performance measure under Program 3.2.70
Older Australians receive residential care services that contributes to their quality of life as measured through: a. provider metrics b. care minutes c. 24/7 nursing.
4.44 The 2023–24 target for this measure was specified as:
a. Establish measurement baseline for ‘Quality of Life’ indicator
b. Maintain average of 200 care minutes per resident per day, including a minimum of 40 minutes of registered nurse (RN) time per day
c. All non-exempt residential aged care facilities have an RN onsite and on duty 100% of the time.71
4.45 In June 2023 the department advised the Minister for Aged Care of a gradual increase in actual care minutes and RN minutes delivered per resident per day since 2020–21 (Figure 4.2). The advice did not include the quarter April to June 2023 (193.98 care minutes delivered and 36.78 RN minutes delivered) as this information was yet to be reported by providers to the department.
Figure 4.2: Performance reporting produced for the Minister, June 2023
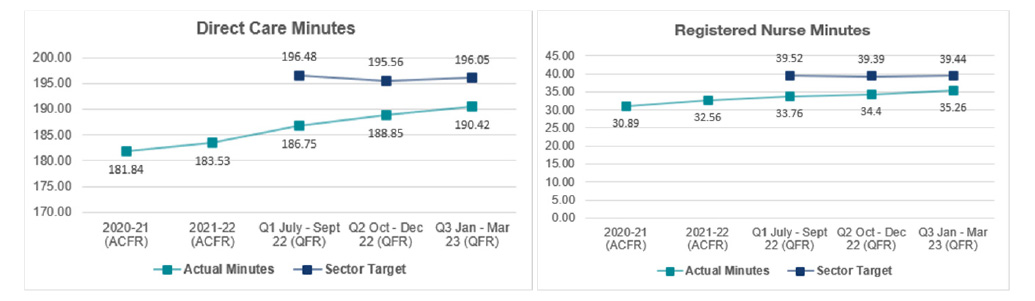
Note: ACFR refers to Aged Care Financial Report, which is a report similar to a QFR submitted annually by approved providers.
Source: Department of Health and Aged Care.
4.46 In August 2023 the department published a dashboard report (see Appendix 6) summarising RN coverage in residential aged care in July 2023. A note to the dashboard indicated that it excludes split service facilities, exempted facilities and facilities where an exemption application is pending. Among six headline statistics depicted on the dashboard were the ‘average percentage of reported hours an RN was on site and on duty’ (98 per cent) and the ‘percentage of reported facilities that have an RN on-site 24/7’ (86 per cent). However, the dashboard also shows that six per cent did not report and that, when non-reporting is taken into account, 81 per cent of mainstream, non-split and non-exempted facilities had reported 24/7 RN coverage.
4.47 Although the department has established public performance measures for mandatory care minutes and 24/7 RN, as noted at paragraph 2.39, as at October 2023, there is no evaluation strategy for the new measures that includes an assessment of the impact of the new measures on aged care quality outcomes.
Aged Care Quality and Safety Commission
4.48 ACQSC’s regulatory operating model includes ‘understanding regulatory impact and outcomes’ as one of five components. ACQSC’s regulatory approach provides that there will be iterative review to provide opportunity for continuous improvement across the three phases of the strategy. The regulatory approach also provides for a post-implementation review to be conducted in July 2024. The regulatory approach defines four measures of success:
Failures in care, or harms to residents where there are gaps in RN coverage are minimised
Unmanaged risks to residents and non-compliance are identified and remedied through regulatory action and engagement with providers preventing future harms
Gaps in RN coverage reduce as the regulatory oversight (including funding arrangements) incentivises providers ‘best efforts’ in ensuring RN coverage
Sector capability and understanding of workforce related responsibilities increases, with a greater focus by governing bodies on effective workforce management and planning, supporting readiness for implementation of the strengthened Quality Standards.
4.49 The regulatory approach does not provide a methodology for collecting data that will be used to measure performance against these four measures of success. No targets for these measures are established. ACQSC does not have a 2023–24 Portfolio Budget Statements measure that is specifically related to care minutes and 24/7 RN regulation.
4.50 ACQSC advised the ANAO that it:
- is still maturing as an organisation that measures regulatory impact as opposed to levels of compliance; and
- considers it prudent to gain experience from early regulatory activity in relation to care minutes and 24/7 RN to better understand how the new measures affect regulatory outcomes before formulating metrics to evaluate the extent to which the measures affect regulatory outcomes.
4.51 ACQSC enforces compliance with eight Quality Standards. Each Quality Standard incorporates a description of the standard to be achieved by a provider and the intended consumer outcome. ACQSC has identified that Quality Standards Two, Three, Seven and Eight are related to 24/7 RN and care minutes (see Table 4.2).
Table 4.2: Quality Standards relevant to 24/7 RN and care minutes
|
Quality Standard |
Provider standard |
Consumer outcome |
|
Quality Standard 2: Ongoing assessment and planning with residents |
The organisation undertakes initial and ongoing assessment and planning for care and services in partnership with the consumer. Assessment and planning has a focus on optimising health and well-being in accordance with the consumer’s needs, goals and preferences. |
I am a partner in ongoing assessment and planning that helps me get the care and services I need for my health and well-being. |
|
Quality Standard 3: Personal care and clinical care |
The organisation delivers safe and effective personal care, clinical care, or both personal care and clinical care, in accordance with the consumer’s needs, goals and preferences to optimise health and well-being. |
I get personal care, clinical care, or both personal care and clinical care, that is safe and right for me. |
|
Quality Standard 7: Human Resources |
The organisation has a workforce that is sufficient, and is skilled and qualified to provide safe, respectful and quality care and services. |
I get quality care and services when I need them from people who are knowledgeable, capable and caring. |
|
Quality Standard 8: Organisational governance |
The organisations’ governing body is accountable for the delivery of safe and quality care and services. |
I am confident the organisation is well run. I can partner in improving the delivery of care and services. |
Source: ANAO, based on ACQSC documentation and Federal Register of Legislation.
4.52 In response to a Royal Commission recommendation, the department released a consultation paper proposing revised Quality Standards that contain multiple statements of expectations for providers corresponding to a single consumer expectation statement for each standard. ACQSC advised the ANAO that the reform of the Quality Standards and the introduction of a new Aged Care Act presents an opportunity to embed the collection and measurement of data about regulatory impact into the regulatory framework.
Recommendation no.4
4.53 The Aged Care Quality and Safety Commission identify a method to assess the impact of care minute and 24/7 RN regulation on aged care quality outcomes and whether regulatory activities are effective at promoting compliance with these measures.
Aged Care Quality and Safety Commission response: Agreed.
4.54 The Commission acknowledges that compliance with these measures is impacted by a range of factors in addition to the Commission’s specific regulatory activities. These include, for example, supplementary funding to the sector and enhanced transparency about compliance with the workforce requirements on My Aged Care. Our evaluation, in collaboration with the Department, will seek to understand our contribution to promoting compliance with the Care Minutes (CM) and 24/7 Registered Nursing (RN) regulation, and more broadly, its relationship to quality and safety outcomes for consumers.
Appendices
Appendix 1 Entity responses
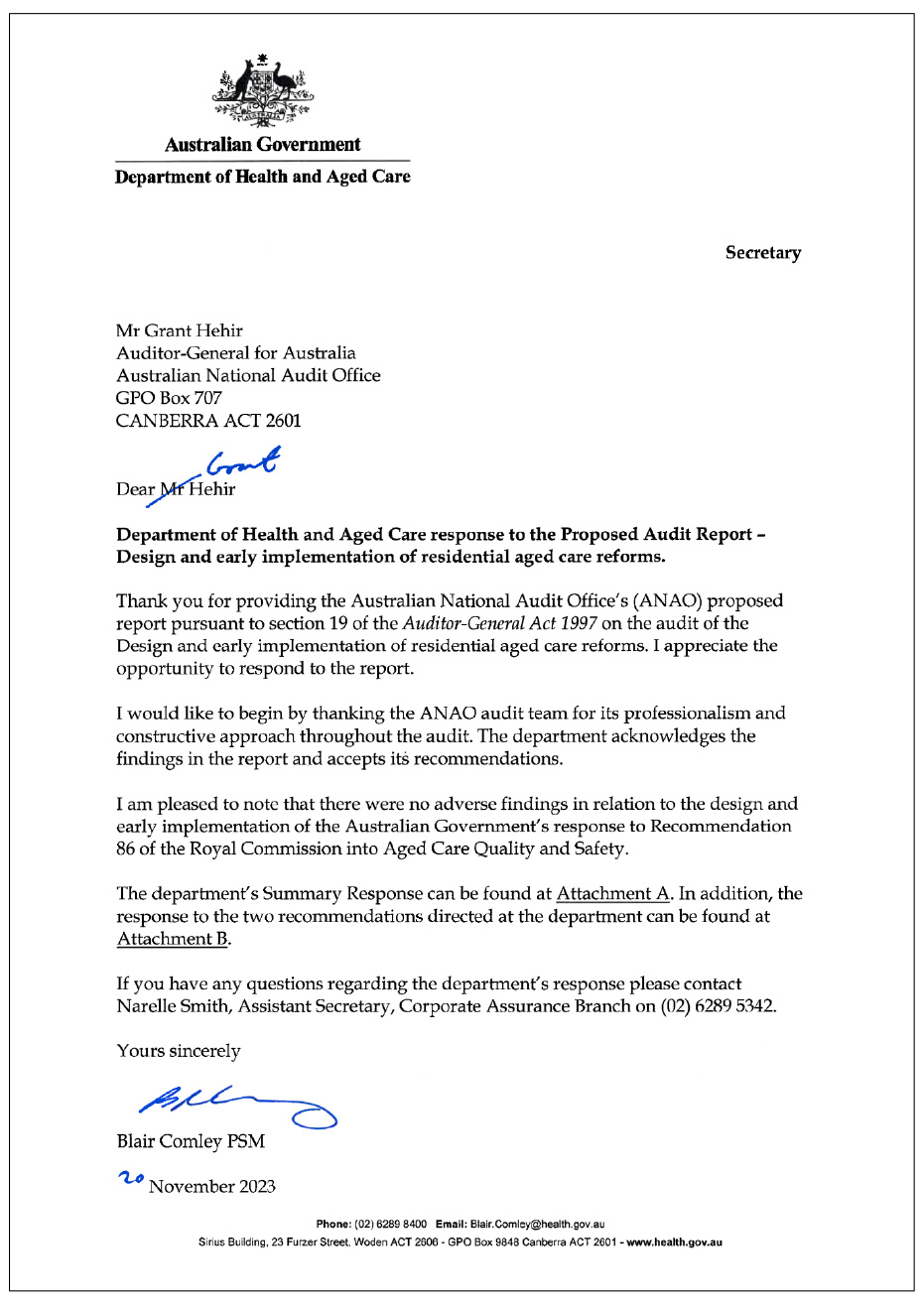
Appendix 2 Improvements observed by the ANAO
1. The existence of independent external audit, and the accompanying potential for scrutiny improves performance. Improvements in administrative and management practices usually occur: in anticipation of ANAO audit activity; during an audit engagement; as interim findings are made; and/or after the audit has been completed and formal findings are communicated.
2. The Joint Committee of Public Accounts and Audit (JCPAA) has encouraged the ANAO to consider ways in which the ANAO could capture and describe some of these impacts. The ANAO’s 2023–24 Corporate Plan states that the ANAO’s annual performance statements will provide a narrative that will consider, amongst other matters, analysis of key improvements made by entities during a performance audit process based on information included in tabled performance audit reports.
3. Performance audits involve close engagement between the ANAO and the audited entity as well as other stakeholders involved in the program or activity being audited. Throughout the audit engagement, the ANAO outlines to the entity the preliminary audit findings, conclusions and potential audit recommendations. This ensures that final recommendations are appropriately targeted and encourages entities to take early remedial action on any identified matters during the course of an audit. Remedial actions entities may take during the audit include:
- strengthening governance arrangements;
- introducing or revising policies, strategies, guidelines or administrative processes; and
- initiating reviews or investigations.
4. During the period examined by this audit, the Department of Health and Aged Care and the Aged Care Quality and Safety Commission made numerous changes to governance arrangements and administrative processes. Many of these changes are described in the body of the report, and it is impractical to list all of these changes here.
Appendix 3 Recommendation 86
Recommendation 86: Minimum staff time standard for residential care
1. The Australian Government should require approved providers of residential aged care facilities to meet a minimum staff time quality and safety standard. This requirement should take the form of a quality and safety standard for residential aged care. The minimum staff time standard should allow approved providers to select the appropriate skills mix for delivering high quality care in accordance with their model of care.
2. From 1 July 2022, the minimum staff time standard should require approved providers to engage registered nurses, enrolled nurses, and personal care workers for at least 200 minutes per resident per day for the average resident, with at least 40 minutes of that staff time provided by a registered nurse.
3. In addition, from 1 July 2022, the minimum staff time standard should require at least one registered nurse on site per residential aged care facility for the morning and afternoon shifts (16 hours per day).
4. From 1 July 2024, the minimum staff time standard should increase to require approved providers to engage registered nurses, enrolled nurses, and personal care workers for the average resident for at least 215 minutes per resident per day for the average resident, with at least 44 minutes of that staff time provided by a registered nurse.
5. In addition, from 1 July 2024, the minimum staff time standard should require at least one registered nurse on site per residential aged care facility at all times.
6. The minimum staff time standard should be linked to the casemix‐adjusted activity based funding model for residential aged care facilities. This means that approved providers with a higher than average proportion of high needs residents would be required to engage additional staff, and vice versa.
7. Approved providers should be able to apply to the System Governor for an exemption from the quality and safety standard relating to staff skills mix, but not the standard relating to numbers of staff. Any exemption should be granted for a limited time, and details of the exemption should be published on My Aged Care. The grounds for granting an exemption should include:
- specific purpose residential aged care facilities, such as specialist homeless facilities, where the profile of the residents is such that it may be appropriate to substitute a registered nurse with another qualified health professional
- residential aged care facilities that are co‐located with a health service, such as Multi‐Purpose Services, where registered and enrolled nurses are present at the collocated health service
- regional, rural and remote residential aged care facilities, where the approved provider can demonstrate it has been unable to recruit sufficient numbers of staff with the requisite skills, and
- residential aged care facilities where an alternative skills mix is being trialled and it would be appropriate to substitute a registered nurse with another qualified health professional. There should be a requirement for any such trial to be comprehensively evaluated and publicly reported.
8. The Australian Commission on Safety and Quality in Health and Aged Care should review and update this standard as appropriate. At a minimum, this should occur in line with significant revisions of the casemix classification for residential aged care facilities, or at least every five years.
Australian Government response (May 2021)
The Government accepts this recommendation and is responding through the measure Residential Aged Care Services and Sustainability ‐ Reforming residential care funding to drive better care and a viable system.
With the introduction of the Australian National Aged Care Classification (AN‐ACC) funding model on 1 October 2022, additional funding will be provided to support services to meet the Royal Commission’s recommended minimum 200 minute care time standard, and having a registered nurse onsite for 16 hours per day. The minimum care time standard will become mandatory from 1 October 2023.
The new Aged Care Act will set minimum staff time standards for residential aged care.
Appendix 4 Care minute target calculations
1. Care minute targets for each provider are derived from the 2017–18 Resource Utilisation and Classification Study (RUCS), which was considered by the Royal Commission into Aged Care Quality and Safety.
2. RUCS proposed the Australian National Aged Care Classification (AN-ACC) model. The AN-ACC model classifies permanent aged care residents into one of 13 classes based on an assessment of mobility, cognitive ability, function and pressure sore risk, and other ‘compounding’ factors (such as wound care and the need for daily injections) (Figure A.1).
Figure A.1: AN-ACC classes for permanent residential aged care residents
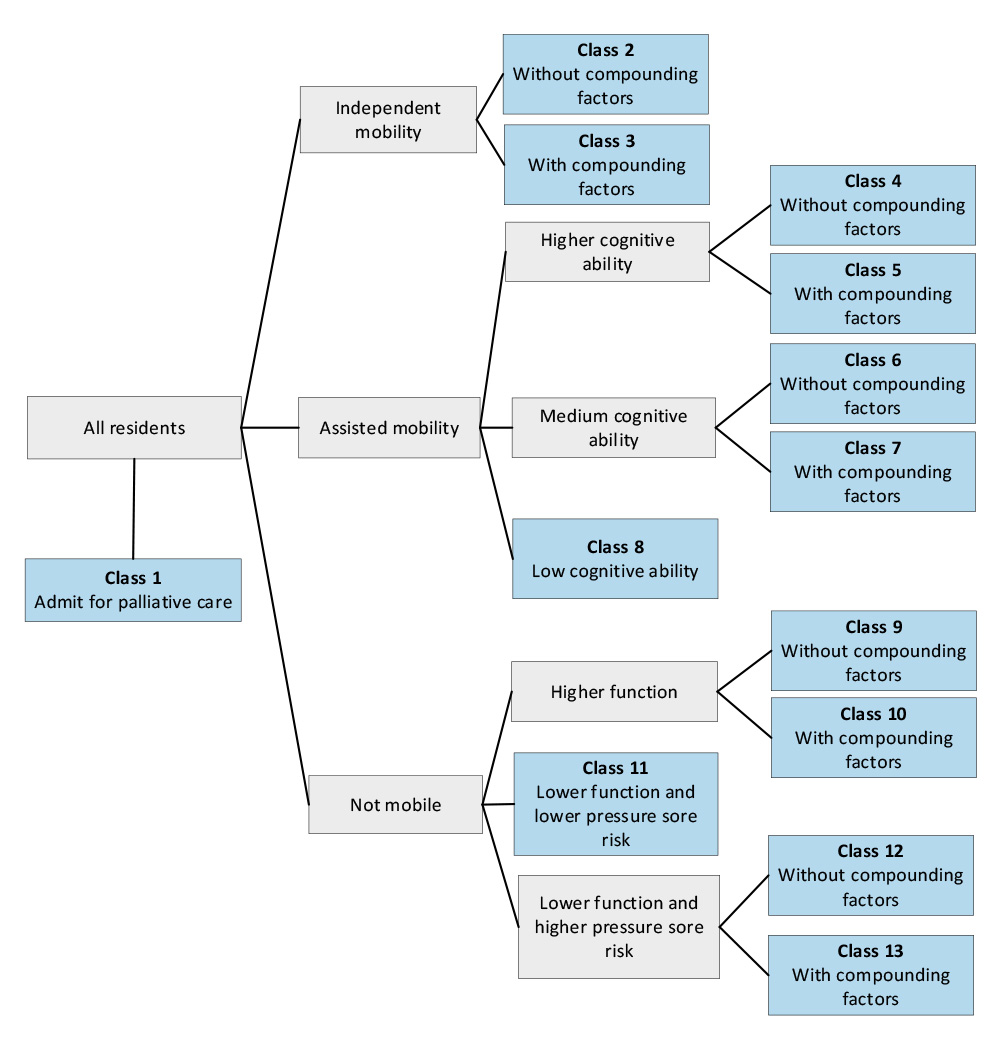
Source: Department of Health and Aged Care.
3. Care minute and registered nurse (RN) minute provider targets are determined as shown in Figure A.2.
- RUCS assigned each of the 13 classes a score (referred to as a ‘relative value unit’ or RVU), which is based on the care needs of each class.
- The Department of Health and Aged Care (the department) combines the RVUs and the spread of the residential aged care population across the 13 classes to calculate a weight to be applied for each of the 13 classes.
- The weight is intended to reflect the needs of a resident for individual (‘tailored’) care weight (e.g. toileting). A separate weight with a value of one for all classes is assigned for shared care (such as assistance at meal times). A combined weight is then calculated for both elements of care, using a 50:50 ratio. From October 2023 this changed to a 64:36 (tailored to shared) ratio instead.
- The final weight is then multiplied by the 200/40 care minute standard to produce a care minute target for each of the 13 AN-ACC classes that reflects the relative care need of each class. The target for higher need AN-ACC classes will be greater than 200 care minutes, while the target for lower need classes will be less than 200 care minutes. In theory, after applying these weights, the sector-wide average target should equate to 200/40 minutes.
- The class target then permits the department to set an individual service-level target that is based on the specific case mix (proportion of residents of each class) in the facilities that the service runs.
Figure A.2: Process followed to determine care minute targets for each AN-ACC class
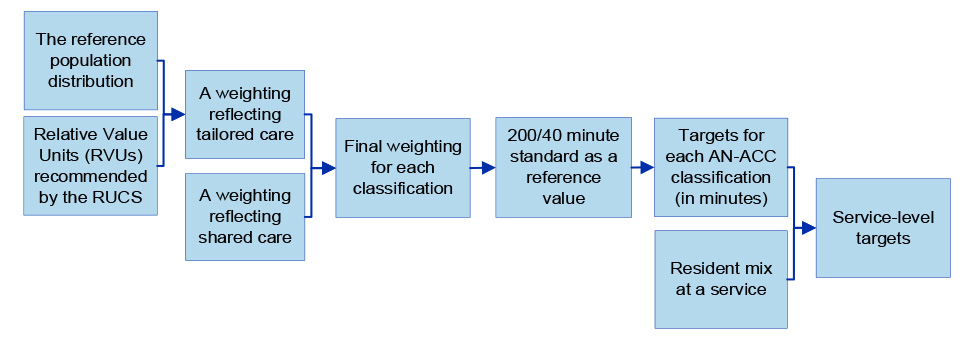
Source: ANAO, based on departmental records.
4. Table A.1 shows the final care minute targets for each AN-ACC class. In calculating the weights for the period October 2022 to September 2023, the department used a January 2022 population distribution of residents across the 13 classes. The actual distribution of occupied bed days in October 2022 and April 2023 is provided in the right hand columns.
5. In May 2023, the department announced amended targets for each AN-ACC class that would apply from 1 October 2023. The new targets were calculated using the same January 2022 population distribution used for targets applying between October 2022 to September 2023.
Table A.1: Care minute and RN minute targets for residents in each AN-ACC class
|
AN-ACC class |
RUCS Relative value units |
Care minutes target (October 2022 – September 2023) |
RN minutes target (October 2022 – September 2023) |
Care minutes target (from October 2023) |
RN minutes target (from October 2023) |
Department’s assessment of distribution of resident population (March 2022)a |
Distribution of occupied bed days (October 2022)b |
Distribution of occupied bed days (April 2023)c |
|
1 |
1.95 |
284 |
53 |
317 |
57 |
1.0% |
0.0% |
0.0% |
|
2 |
0.37 |
135 |
32 |
110 |
30 |
6.3% |
5.1% |
3.9% |
|
3 |
0.61 |
157 |
34 |
143 |
32 |
2.3% |
1.8% |
1.4% |
|
4 |
0.41 |
139 |
30 |
115 |
28 |
6.8% |
7.8% |
7.2% |
|
5 |
0.73 |
169 |
39 |
157 |
39 |
20.0% |
21.0% |
20.2% |
|
6 |
0.69 |
166 |
35 |
152 |
34 |
7.3% |
8.5% |
8.5% |
|
7 |
0.95 |
189 |
37 |
186 |
36 |
12.1% |
13.7% |
14.3% |
|
8 |
1.05 |
200 |
38 |
200 |
38 |
8.4% |
8.4% |
8.8% |
|
9 |
1.06 |
200 |
44 |
202 |
46 |
7.3% |
7.2% |
6.9% |
|
10 |
1.70 |
261 |
52 |
282 |
56 |
4.9% |
4.4% |
4.8% |
|
11 |
1.63 |
254 |
41 |
274 |
41 |
12.0% |
11.8% |
12.4% |
|
12 |
1.59 |
250 |
42 |
269 |
42 |
2.9% |
2.7% |
2.8% |
|
13 |
1.95 |
284 |
53 |
317 |
57 |
8.8% |
7.6% |
8.8% |
Note a: Calculated in March 2022, based on January 2022 data.
Note b: An occupied bed is an available bed where there is a patient physically in the bed or the bed is being retained for a patient (e.g. the patient is receiving treatment or is on leave). Days were calculated for the month of October 2022. A resident who occupied a bed for the entire month would count as 31 occupied bed days.
Note c: Days were calculated for the month of April 2023.
Source: ANAO, based on departmental records.
6. The care minute and RN minute targets for each AN-ACC class are used in combination with actual occupancy data at a residential aged care service to set a quarterly care minute and RN minute target that is specific to each service. Between July 2022 to October 2023 the department used occupancy data from the preceding quarter to set the target for the following quarter.
7. For example, the department calculated care minute targets for ‘Service A’, as depicted in Figure A.3. The July to September 2022 target was based on the provider’s actual residency and care need case mix that applied in April to June 2022. Similarly, the October to December 2022 target was based on July to September 2022 data. Due to changes in care needs in the resident population from one quarter to the next for that service, the daily care minute targets did not reflect the actual care needs of the residents in any quarter.
Figure A.3: Care minute targets and actual need for ‘Service A’, July 2022 to March 2023
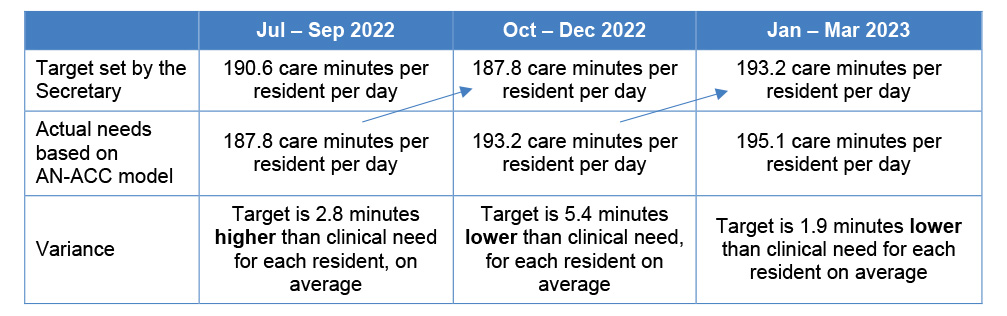
Source: ANAO, based on departmental records.
8. The department advised the ANAO that from 1 October 2023 (when 200/40 care minutes became mandatory), targets would be calculated based on a three-month reference period (e.g. June to August 2023) and then advised to providers in the month prior (e.g. September 2023) to the relevant quarter (e.g. October to December 2023) commencing. The revised approach means that older historical data is used to calculate the target.
Appendix 5 Regulatory approach to new workforce measures
1. The Aged Care Quality and Safety Commission’s (ACQSC’s) regulatory approach set out three phases of activity:
Phase 1: Preparation for, and implementation of, the 24/7 RN responsibility.
Phase 2: Preparation for, and implementation of, mandatory care minutes targets (to be developed following implementation of Phase 1).
Phase 3: Running in parallel to Phases 1 and 2, deployment and revision of an agile monitoring and regulation model for workforce-related responsibilities across three tranches of regulatory activity from July 2023 to July 2024, in response to:
- an increasing quantum of data on reported gaps in RN coverage (Phase 1) and care minute targets (Phase 2); and
- increased … pre-planned and responsive monitoring activities informed by risk factors including incoming RN gap-data and other regulatory intelligence.
2. The regulatory approach divided Phase 3 into three tranches targeting specific cohorts of providers:
Tranche 1 – July to October 2023: Services that applied for but did not successfully gain an exemption; services that applied for an exemption and were identified as high risk by the assessment team at time of application; any service where other indicators of risk suggest that there may be an issue with staffing sufficiency and clinical care.
Tranche 2 – November 2023 to February 2024: Services with the largest proportion of gaps in 24/7 coverage, combined with deficient alternative care arrangements and that have other high risk indicators (noting that these risk indicators will be refined from learnings in tranche 1); services with the largest deficits across all care minutes requirements (RN, EN and PCW) and that have other high risk indicators; exempt services not monitored in Tranche 1.
Tranche 3 – March to June 2024: Priorities to be informed by outcomes of tranche[s] 1 and 2.
3. The regulatory approach also set out the expected operational impacts of the introduction of 24/7 RN and mandatory care minutes on other functions within ACQSC.
Appendix 6 Registered Nurse dashboard reports, July to September 2023
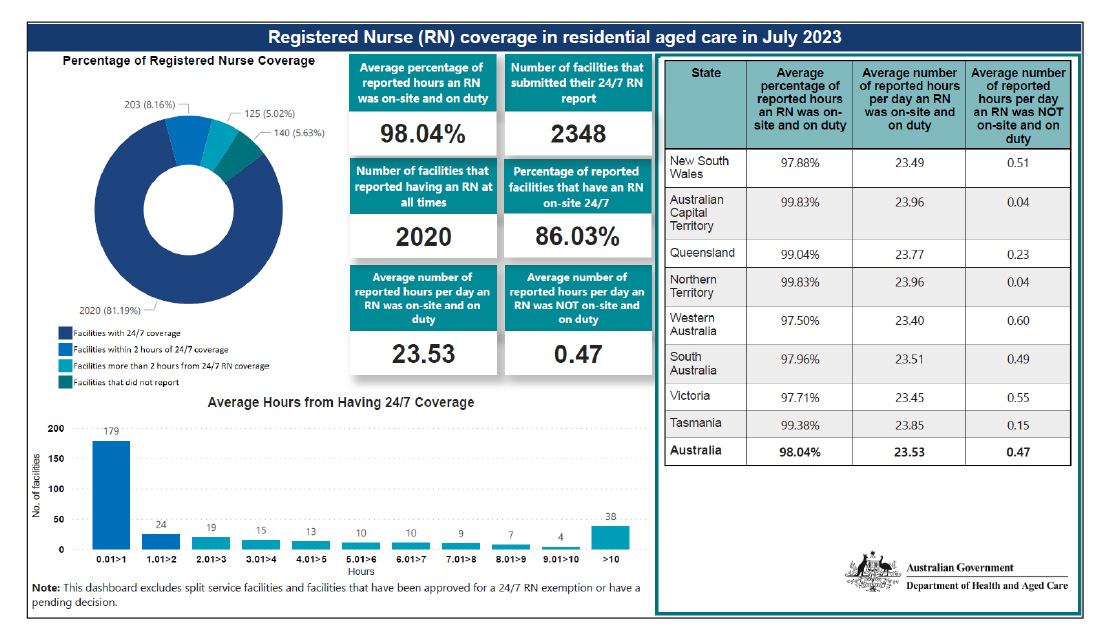
Source: Department of Health and Aged Care, Registered nurse coverage in residential aged care dashboard [internet], available at https://www.health.gov.au/resources/publications/registered-nurse-coverage-in-residential-aged-care-dashboard [accessed 21 August 2023].
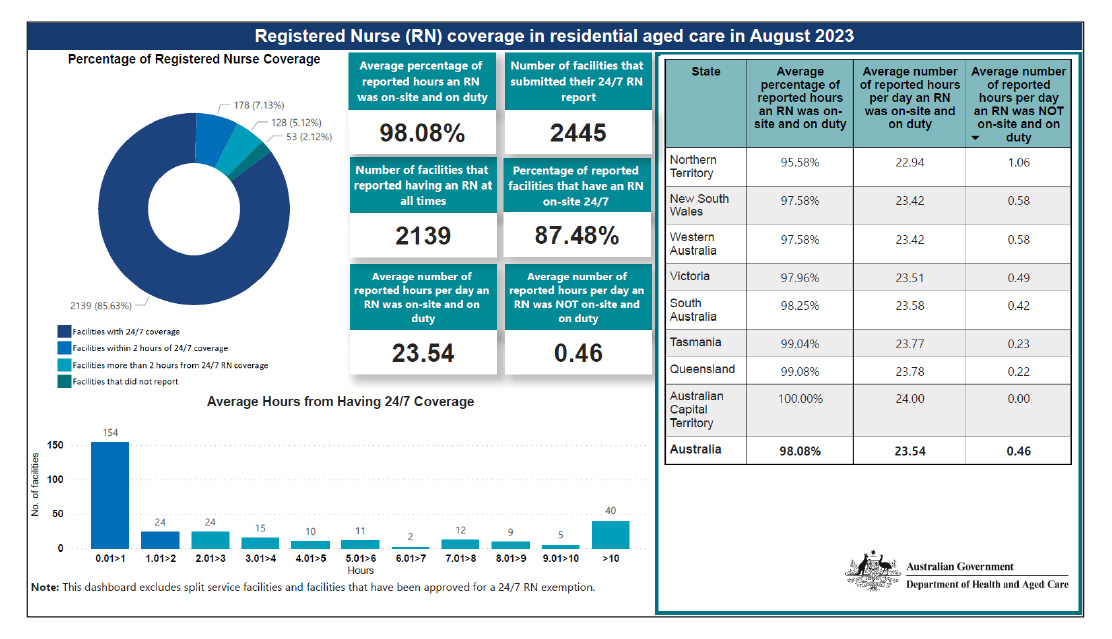
Source: Department of Health and Aged Care, Registered nurse coverage in residential aged care dashboard [internet], available at https://www.health.gov.au/resources/publications/registered-nurse-coverage-in-residential-aged-care-dashboard [accessed 18 October 2023].
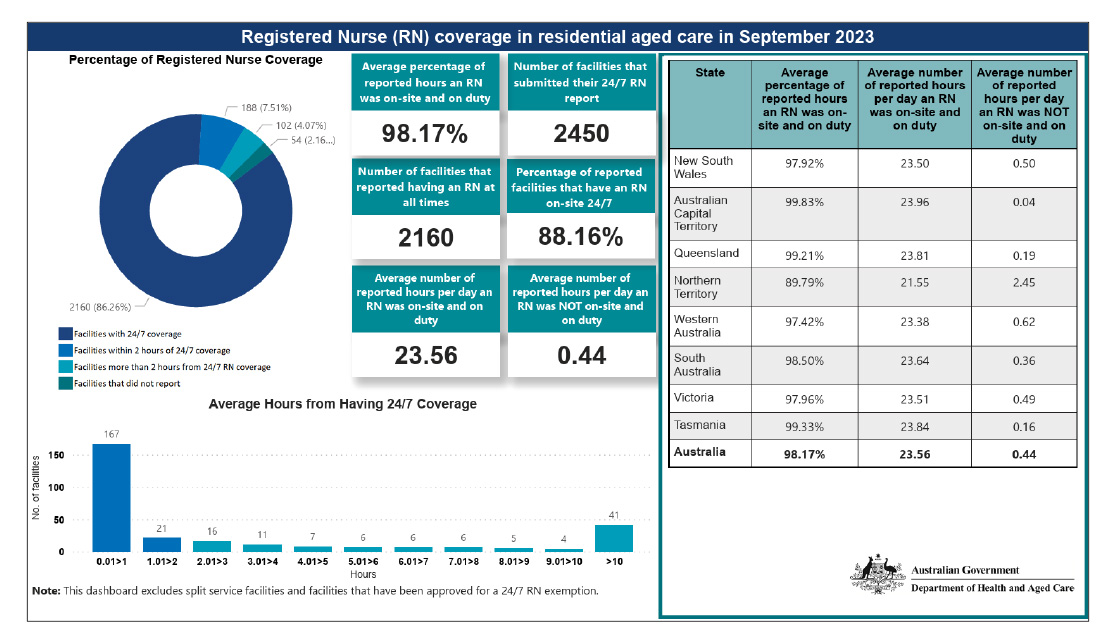
Source: Department of Health and Aged Care, Registered nurse coverage in residential aged care dashboard [internet], available at https://www.health.gov.au/resources/publications/registered-nurse-coverage-in-residential-aged-care-dashboard [accessed 27 November 2023].
Footnotes
1 Aged Care Act 1997, section 41-3 (definition of ‘residential care’) and schedule 1 (Dictionary).
2 Approval of Care Recipients Principles 2014, section 11A. Persons who do not meet these age requirements but have disabilities that require accommodation and support services similar to those provided in residential aged care facilities may also be subsidised if no suitable alternative to a residential aged care facility is available.
3 Aged Care Act 1997, section 43-1.
4 Mainstream services exclude Multi-Purpose Services and services provided under the National Aboriginal and Torres Strait Islander Flexible Aged Care Program.
5 The total number of residents who received residential care on a permanent basis at any point in the full 2022–23 financial year was 250,273.
6 Australian Government, Portfolio Budget Statements 2023–24: Budget related paper No. 1.9, Health and Aged Care Portfolio, pp. 93 and 101, available at https://www.health.gov.au/sites/default/files/2023-05/health-portfolio-budget-statements-budget-2023-24.pdf [accessed 8 August 2023].
7 Royal Commission into Aged Care Quality and Safety, Final Report: Royal Commission into Aged Care Quality and Safety, Volume 1, p. 73, available at https://agedcare.royalcommission.gov.au/sites/default/files/2021-03/final-report-volume-1_0.pdf [accessed 31 July 2023].
8 Quality of Care Principles 2014 (as made), schedule 1, part 1, section 1, item 1.7, https://www.legislation.gov.au/Details/F2014L00830 [accessed 9 August 2023].
9 Quality of Care Amendment (Single Quality Framework) Principles 2018, schedule 1, paragraph 6(3)(a), https://www.legislation.gov.au/Details/F2018L01412 [accessed 9 August 2023].
10 See Appendix 3 for the full text of Recommendation 86.
11 Committee for Economic Development of Australia, Duty of Care: Meeting the aged care workforce challenge, 9 August 2021, available from https://cedakenticomedia.blob.core.windows.net/cedamediacontainer/kentico/media/researchcataloguedocuments/recent%20research/pdfs/aged-care-workforce-2021-final_1.pdf [accessed 29 August 2023].
12 University of Technology Sydney Ageing Research Collaborative, Australia’s Aged Care Sector Full Year Report 2021-22, 25 November 2022, p. 92, available from https://opus.lib.uts.edu.au/bitstream/10453/163697/2/UARC_Aged%20Care%20Sector%20Full%20Year%20Report%202021-22.pdf [accessed 29 August 2023].
13 ibid., p. 11.
14 The Joint Committee of Public Accounts and Audit has identified the operation of information-gathering powers under the Auditor-General Act 1997 as an issue that should be considered further by the Committee. Joint Committee of Public Accounts and Audit, Parliament of Australia, Report 491 Review of the Auditor-General Act 1997 (2022), pp. 36-39, available at https://www.aph.gov.au/Parliamentary_Business/Committees/Joint/Public_Accounts_and_Audit/~/link.aspx?_id=55642D5AAA1D44E8B818F3DA84B8FE7B&_z=z [accessed 9 October 2023].
15 Australian Government, Policy Hub, Introduction to delivering great policy [Internet], available from https://www.policyhub.gov.au/model [accessed 1 August 2023].
16 Royal Commission into Aged Care Quality and Safety Submissions by the Commonwealth, The future of the aged care workforce, 13 March 2020, p. 3, available from https://webarchive.nla.gov.au/awa/20230921191316/https://agedcare.royalcommission.gov.au/system/files/2020-09/AWF.650.00110.0001.pdf [accessed 11 October 2023]
17 Australian Government, Submissions by Commonwealth Departments in response to Counsel Assisting’s Final Submissions (RCD.0013.0014.0037), 12 November 2020, available from https://webarchive.nla.gov.au/awa/20230923080447/https://agedcare.royalcommission.gov.au/system/files/2021-02/RCD.0013.0014.0037.pdf [accessed 11 October 2022]
18 Royal Commission into Aged Care Quality and Safety Counsel Assisting’s Submissions on Workforce, 26 February 2020, p. 34, available from https://webarchive.nla.gov.au/awa/20230921101302/https://agedcare.royalcommission.gov.au/sites/default/files/2020-03/submissions-by-counsel-assisting.pdf [accessed 11 October 2020]; Royal Commission into Aged Care Quality and Safety Counsel Assisting’s Final Submissions, 22 October 2020, p. 211, available from https://webarchive.nla.gov.au/awa/20230921190002/https://agedcare.royalcommission.gov.au/sites/default/files/2021-02/RCD.9999.0541.0001.pdf [accessed 11 October 2023]
19 Prime Minister and Cabinet, Australian Government Guide to Regulatory Impact Analysis [Internet], March 2020, available from https://obpr.pmc.gov.au/sites/default/files/2021-06/australian-government-guide-to-regulatory-impact-analysis.pdf) [accessed 13 August 2023]. A revised guide was issued by the Office of Impact Analysis in February 2023.
20 The seven RIS questions that applied at the time were: What is the policy problem you are trying to solve? Why is government action needed? What policy options are you considering? What is the likely net benefit of each option? Who did you consult and how did you incorporate their feedback? What is the best option from those you have considered? How will you implement and evaluate your chosen option?
21 Prime Minister and Cabinet, Australian Government Guide to Regulatory Impact Analysis [Internet], March 2020, p. 57, available from https://obpr.pmc.gov.au/sites/default/files/2021-06/australian-government-guide-to-regulatory-impact-analysis.pdf) [accessed 13 August 2023].
22 Letter from Department of Health to the Office of Best Practice Regulation, available at https://oia.pmc.gov.au/sites/default/files/posts/2021/06/certification_of_independent_reviews_-_22_march_2021.pdf [accessed 13 August 2023].
23 Prior to 18 November 2022 the OIA was named the Office of Best Practice Regulation.
24 Department of Health and Aged Care, Letter to Office of Best Practice Regulation, Certification of independent reviews: Initial response to the Royal Commission (Quality and Safety) – Strengthening providers; New Aged Care Act, dated 7 July 2022, available at https://oia.pmc.gov.au/sites/default/files/posts/2022/08/Certification%20letter%2024-7%20Registered%20Nurses%20and%20Minimum%20Care%20Minutes.pdf [accessed 14 August 2023].
25 Department of Health and Aged Care, Introduction of 24/7 onsite registered nurse and increased minimum care minutes requirements: Supplementary Regulatory Impact Analysis, July 2022, available at https://oia.pmc.gov.au/sites/default/files/posts/2022/08/Supplementary%20Regulatory%20Impact%20Analysis%20-%2024-7%20Nurses%20Registered%20Nurses%20and%20Minimum%20Care%20Minutes.pdf [accessed 15 August 2023].
26 Department of Finance, Resource Management Guide 107: Risk Potential Assessment Tool [Internet],, available at https://www.finance.gov.au/risk-potential-assessment-tool-rmg-107 [accessed 19 July 2023].
27 Auditor-General Report No. 10 2022–23 Expansion of Telehealth Services, p. 28.
28 Department of the Prime Minister and Cabinet, Cabinet Handbook (14th edition), PM&C, 2020, p. 11 and Department of the Prime Minister and Cabinet, Cabinet Handbook (15th edition), PM&C, 2022, p. 32.
29 The department used the Modified Monash Model (areas 5 to 7) to specify these locations. A factsheet explaining the Modified Monash Model geographical classification scheme can be found at Department of Health and Aged Care, Modified Monash Model – fact sheet [Internet], available at https://www.health.gov.au/resources/publications/modified-monash-model-fact-sheet [accessed 8 September 2022].
30 RNs and ENs require specific professional qualifications and registration. A PCW provides a range of care services including personal care, cleaning and food services for aged care residents under the direction and support of an EN or RN and does not require specific skills or qualifications.
31 Department of Health and Aged Care, 2020 Aged care workforce census report, September 2021, p. 13, available at https://www.health.gov.au/sites/default/files/documents/2021/10/2020-aged-care-workforce-census.pdf [accessed 1 August 2023].
32 In comparison, the response rate to the 2016 Census was 76 per cent. See Department of Health, Aged Care Workforce, 2016, March 2017, p. 8, available at https://gen-agedcaredata.gov.au/www_aihwgen/media/Workforce/The-Aged-Care-Workforce-2016.pdf [accessed 10 August 2023].
33 A Howe, ‘The 2020 Aged Care Workforce Census and Issues Arising for Residential Care Workforce Planning and Policy’, The Australian Economic Review, 55(3), 2022, p. 342.
34 ibid., p. 331.
35 The QFR is a report submitted to the department quarterly in relation to each residential aged care service that contains information such as viability and prudential compliance, quarterly financial statements, residential care labour cost and hours; and food and nutrition. The first QFR, concerning the period July to September 2022, was due on 4 November 2022.
36 The Aged Care Council of Elders was established by the government as an advisory body to the aged care reforms. Members of the Council are appointed by the Minister for Health and Aged Care.
37 Department of the Treasury, Commonwealth Evaluation Policy [Internet], Treasury, 2021, available at https://evaluation.treasury.gov.au/about/commonwealth-evaluation-policy [accessed 16 October 2023].
38 Department of Finance, Resource Management Guide 130 Evaluation in the Commonwealth: Why evaluate?, Finance, available at https://webarchive.nla.gov.au/awa/20211213010854/https://www.finance.gov.au/government/managing-commonwealth-resources/planning-and-reporting/commonwealth-performance-framework/evaluation-commonwealth-rmg-130/why-evaluate [accessed 16 October 2023].
39 Australian Government, Policy Hub, Introduction to delivering great policy [Internet], available at https://www.policyhub.gov.au/model [accessed 1 August 2023].
40 Department of Health and Aged Care, Introduction of 24/7 onsite registered nurse and increased minimum care minutes requirements, Supplementary Regulatory Impact Analysis, July 2022, pp. 8–9, available at https://oia.pmc.gov.au/sites/default/files/posts/2022/08/Supplementary%20Regulatory%20Impact%20Analysis%20-%2024-7%20Nurses%20Registered%20Nurses%20and%20Minimum%20Care%20Minutes.pdf [accessed 14 August 2023].
41 These elements are included in Department of Finance, Quick Reference Guide: Evaluation planning for new policy proposals [Internet] available at https://www.finance.gov.au/quick-reference-guide-evaluation-planning-new-policy-proposals [accessed 15 August 2023].
42 A Post Implementation Review evaluates whether the regulation remains appropriate, and how effective and efficient it has been in meeting its objectives. Office of Impact Analysis, Post-implementation reviews August 2023 [Internet), available at https://oia.pmc.gov.au/sites/default/files/2023-08/post-implementation-reviews_1.pdf [accessed 15 August 2023].
43 Mr Ian Yates AM commenced as Interim Inspector-General of Aged Care on 30 January 2023 and became the acting Inspector-General of Aged Care upon the commencement of the Inspector-General of Aged Care Act 2023 on 16 October 2023.
44 The NATSIFAC Program Manual outlines the operational requirements of the NATSIFAC Program. It is designed for service providers funded under the NATSIFAC Program and forms part of their NATSIFAC Program grant agreement.
45 The star ratings system assigns an overall star rating and star ratings in four categories (compliance, residents’ experience, staffing minutes and quality measures) to residential aged care services on a public facing website operated by the department (My Aged Care) to help older Australians and their representatives make more informed choices about their care. Further information is available on the department’s website at https://www.health.gov.au/our-work/star-ratings-for-residential-aged-care [accessed 23 November 2023].
46 The department advised that actual resident care needs were slightly lower on average, when compared to the earlier data upon which the formula was based, and this resulted in the sector average care minute target being lower than 200/40 minutes.
47 Recommendation 86 was informed by research that found the average level of care in Australian residential aged care facilities was 180/36 minutes. The Royal Commission stated that ‘the status quo is unacceptable’. Royal Commission into Aged Care Quality and Safety, Final Report: Royal Commission into Aged Care Quality and Safety, Volume 1, pp. 8, 29, 129-130, available at https://agedcare.royalcommission.gov.au/sites/default/files/2021-03/final-report-volume-1_0.pdf [accessed 31 July 2023].
48 Providers must know a mandatory quarterly target before the quarter has commenced. The time taken to calculate the target meant that the target could only be advised to providers after the quarter had commenced.
49 The 200/40 target applies to all NATSIFAC services regardless of the care needs of residents because residents of NATSIFAC services are not assessed and classified under the AN-ACC funding model, meaning a casemix adjusted target cannot be set.
50 Excludes four applications that were subsequently withdrawn by the applicant and applications for three facilities that were ineligible by reason of location or bed numbers.
51 ‘Complete’ means that the department possessed all information from the applicant and ACQSC required to be considered by the delegate.
52 For legal reasons, from 16 April 2023 the process required ACQSC to identify information gaps to the department, who would request this information from the applicant. The department proposed on 23 June 2023 that joint phone calls be made to enable ACQSC staff to talk directly to applicants.
53 A provider must explain the circumstances of each block of 30 minutes or more during a month in which an RN was not on-site and on-duty.
54 Section 54-1A of the Aged Care Act requires the Secretary (or delegate) to be satisfied that the provider has taken reasonable steps to ensure that the clinical care needs of the care recipients in the facility will be met during the period for which the exemption is in force.
55 The ACTP Steering Committee is chaired by the Deputy Secretary Ageing and Aged Care Group and comprises the chair, two other Deputy Secretaries, five First Assistant Secretaries from the Ageing and Aged Care Group, First Assistant Secretaries from Information Technology, Digital Transformation and Delivery, and Health Economics and Research divisions, the Chief Nursing and Midwifery Officer, the Aged Care Quality and Safety Commissioner, a representative from Services Australia and an independent assurance adviser.
56 ACQSC’s operating model is described on page 29 of its 2023–24 Corporate Plan, available at https://www.agedcarequality.gov.au/sites/default/files/media/acqsc-corporate-plan-2023-24.pdf [accessed 5 October 2023].
57 Royal Commission into Aged Care Quality and Safety, Final Report: Care, Dignity and Respect (Volume 1), pp. 15–16 and 49–50, Commonwealth of Australia, 2021; Carnell K and Paterson R, Review of National Aged Care Quality Regulatory Processes, Commonwealth of Australia, October 2017, pp. 77–78; Productivity Commission, Caring for Older Australians, Report No. 53, 2011, Commonwealth of Australia, p. 387.
58 Department of Finance, Resource Management Guide 128: Regulator Performance, Finance, 2023.
59 The department has other statutory powers, such as section 93-1 of the Aged Care Act, that could be used in limited circumstances to test the veracity of information provided to the department in relation to a claim for the 24/7 RN supplement.
60 Under section 76 of the ACQSC Act, the Commissioner may delegate the ability to impose sanctions for provider non-compliance, however the Commissioner cannot delegate other enforcement and compliance powers. Under section 34, the Commissioner may make arrangements to be assisted by departmental staff to perform services in connection with the performance of any of the Commissioner’s functions, including ensuring compliance with the Aged Care Act and ACQSC Act.
61 A Statement of Intent is issued by a regulator to set out how it will deliver on the Australian Government’s expectations regarding regulatory policy objectives and the conduct of regulatory activities. Ministers and secretaries are responsible for identifying what are the regulatory functions within a department. See Department of Finance, Guidance Note to Resource Management Guide 128 Regulator Performance, Finance, 20 February 2023, available at https://www.finance.gov.au/government/managing-commonwealth-resources/regulator-performance-rmg-128/guidance-note [accessed 18 October 2023].
62 In this report, the ANAO has used ‘consultative forum’ to refer to certain advisory bodies convened by the department or ACQSC.
63 The department and ACQSC maintain websites that publish information about the new requirements, generally directed at approved providers of residential aged care. The department also maintains My Aged Care, which is website designed to be read by consumers and families rather than providers.
64 In response to Recommendation 100 of the Royal Commission, on 1 April 2021 the Australian Government introduced a requirement for providers to report a broad range of serious incidents such as sexual misconduct, neglect, psychological abuse and inappropriate use of restraint to ACQSC.
65 In response to Recommendation 77 of the Royal Commission, the Australian Government introduced a code of conduct for aged care workers and empowered ACQSC to enforce compliance with the code.
66 Approved providers are required to comply with eight aged care Quality Standards, which set out minimum standards of care in domains such as consumer dignity and choice, personal and clinical care, and organisational governance. The aged care Quality Standards are outlined at: Aged Care Quality and Safety Commission, Quality Standards [Internet], ACQSC, 2022, available at https://www.agedcarequality.gov.au/providers/standards [accessed 19 August 2023].
67 ACQSC Outcome 1 (Protect and enhance the safety, health, wellbeing and quality of life of aged care consumers, including through effective engagement with them, regulation and education of Commonwealth-funded aged care service providers and resolution of aged care complaints.).
Australian Government, Portfolio Budget Statements 2023–24, Budget Related Paper 1.9 (Budget Initiatives and Explanations of Appropriations), 2023, p. 7.
68 Department of Health and Aged Care Outcome 3: Ageing and Aged Care (Improved wellbeing for older Australians through targeted support, access to appropriate, high quality care, and related information services.).
Australian Government, Portfolio Budget Statements 2023–24, Budget Related Paper 1.9 (Budget Initiatives and Explanations of Appropriations), 2023, pp. 6 and 93.
69 Unlike Program 3.3, Program 3.2 is not linked to ACQSC’s single outcome in the Portfolio Budget Statements.
70 Australian Government, Portfolio Budget Statements 2023–24, Budget Related Paper 1.9 (Budget Initiatives and Explanations of Appropriations), 2023, p. 102.
71 The measure is calculated as ‘the amount of time’ an RN was onsite and on duty, averaged across all residential facilities each month and averaged across all months to produce an annualised percentage. The methodology for care minute and 24/7 RN performance measures excludes non-mainstream services.