Browse our range of reports and publications including performance and financial statement audit reports, assurance review reports, information reports and annual reports.
Administration of the Agreements for the Management, Operation and Funding of the Mersey Community Hospital
Please direct enquiries relating to reports through our contact page.
The objective of the audit was to assess the effectiveness of the administration, by DoHA and the Commonwealth partners, of the 2008 and 2011 Heads of Agreement for the management, operation and funding of the Mersey Community Hospital (The Commonwealth partners for this audit were the Tasmanian Government Department of Health and Human Services and the Tasmanian Health Organisation – North West).
Summary
Introduction
1. The Mersey Community Hospital (MCH) is located in Latrobe, 10 kilometres south-east of Devonport, Tasmania. The MCH provides hospital services to around 62 000 people in a catchment area that is characterised by population growth over recent years, an ageing population, socio-economic disadvantage and significant chronic disease, particularly cardiovascular disease, diabetes and cancer.
2. The MCH has approximately 100 beds and provides medical services, including emergency, general adult and paediatric medicine, general surgery, ophthalmological, some oncology, limited rehabilitation and allied health support. There are approximately 500 staff members employed at the MCH.1
3. First opened in 1961, the MCH has been operated at various times in its history by the Tasmanian Government and by private providers. In November 2007, the Commonwealth purchased the MCH from the Tasmanian Government in response to local community concern over proposed service changes at the hospital. The MCH is the only hospital in Australia both owned and directly funded by the Commonwealth. Since 1 September 2008, the Tasmanian Government has managed and operated the MCH under successive Heads of Agreement (HoA) with the Commonwealth, endorsed in 2008 and 2011, which have provided Commonwealth funding of $169.8 million and $197.5 million respectively for this purpose.2
4. Over the period in which the Tasmanian Government has managed and operated the MCH under the HoA, the Australian health care system has undergone significant reform. This includes: the 2011 National Health Reform Agreement (NHRA), which established independent Local Hospital Networks as the management model for public hospitals, with states and territories funded as system administrators; and the National Health Performance Authority, supported by a Performance and Accountability Framework (PAF), to improve transparency and accountability for hospital performance.
5. Until 30 June 2012, the MCH was managed as part of Tasmania’s North West Area Health Service (NWAHS), a division of the Tasmanian Government Department of Health and Human Services (DHHS). On 1 July 2012, in accordance with the NHRA’s requirement that states and territories establish Local Hospital Networks, the three Area Health Services in Tasmania—North West, North and South—became Tasmanian Health Organisations.3 The MCH has been managed by the Tasmanian Health Organisation-North West (THO-NW) since 1 July 2012. However, the current HoA remains an agreement between the Commonwealth and Tasmania, and continues to be administered by the Australian Government Department of Health and Ageing (DoHA) and DHHS. The THO areas and Tasmania’s acute hospitals are shown in Figure S1.
Figure S.1: Tasmanian Health Organisation areas and acute hospital locations
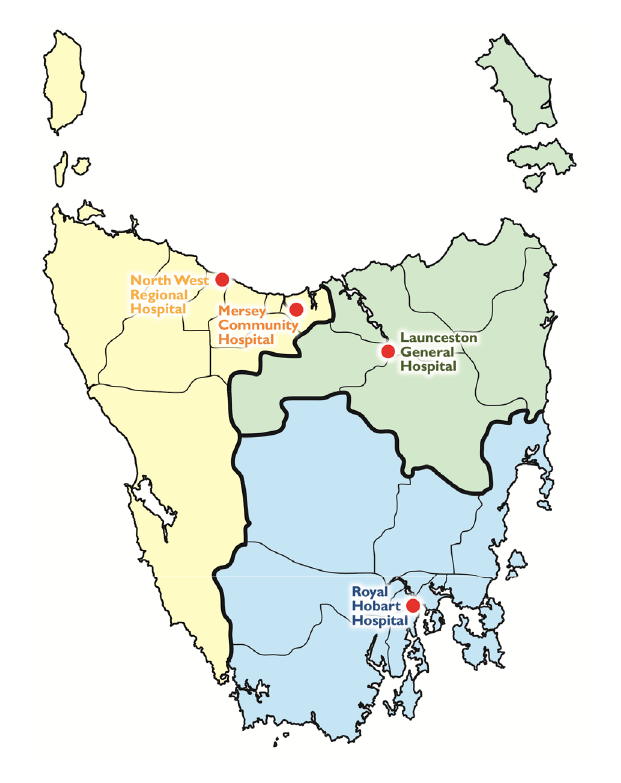
Source: DHHS.
Commonwealth acquisition of the Mersey Community Hospital
6. Under the Tasmanian Government’s ownership and operation of the then Mersey Hospital prior to November 2007, the hospital formed one campus of a single North West Regional Hospital (NWRH), with the other campus at Burnie, 56 kilometres north-west of Latrobe.
7. The Tasmanian Government’s Tasmania’s Health Plan, which was released in May 2007, announced a strategy to address issues of sustainability, service duplication, costs and health care quality in North West Tasmania by consolidating high acuity inpatient, intensive care and emergency services at the Burnie campus of the NWRH. The Mersey campus would focus on lower risk and sub-acute services, short stay services, including day surgery, and specialist outpatient services.
8. In response to the local community’s concerns regarding the proposed service changes, the then Prime Minister, the Hon John Howard MP, announced on 1 August 2007 that the Commonwealth would directly fund a Community Trust to operate the MCH, which it would seek to lease from Tasmania. The Tasmanian Government did not agree to lease the hospital to the Commonwealth, but offered to sell it for $1, subject to conditions.
9. Following negotiations between the two governments, the Commonwealth assumed ownership of the MCH from the Tasmanian Government on 23 November 2007, for a purchase price of $1.10 (GST inclusive), the day before the 2007 Federal election. In summary, the Australian Government’s key policy objectives in assuming ownership of the MCH were to:
- restore and maintain the full range of services provided at the MCH prior to the Tasmanian Government’s announcement of service changes in Tasmania’s Health Plan 2007; and
- introduce community-based operation of the hospital through a Trust, funded by the Commonwealth, and test this as a model for other regional hospitals.
10. During the 2007 election campaign, the Australian Labor Party committed to honour the agreement made between the Howard Government and the Tasmanian Government.4 Following the change of government, in March 2008, the Australian Government decided:
- not to proceed with the Community Trust model announced by the previous Government;
- that it was not practical or cost-effective for DoHA to have direct operational responsibility for the MCH beyond 30 June 2008; and
- to commence a tender process to identify a private sector service provider to operate the MCH from that date.
11. The subsequent tender process did not result in a concluding bid, and the Government opted to enter into a negotiation process with the Tasmanian Government, represented by DHHS, to resume operating and managing the MCH under Commonwealth ownership. Subsequently, a HoA was signed by the Australian and Tasmanian governments on 27 August 2008 establishing the terms and conditions for the Commonwealth owned and funded MCH to be managed and operated by Tasmania until 30 June 2011.
12. The services required to be delivered at the MCH were set out in the Schedule to the HoA as the core clinical activities of the hospital, with the Commonwealth’s objective as owner of the MCH set out in Recital A as follows:
As the owner of the Mersey Community Hospital at Latrobe in the North West region of Tasmania, the Commonwealth seeks to ensure that the people in its catchment area have appropriate access within clinically appropriate times to a range of safe health care services based on clinical need.5
Management and operation of the Mersey Community Hospital by Tasmania
13. The Tasmanian Government resumed managing and operating the MCH on 1 September 2008. A second HoA was signed on 23 June 2011 continuing the arrangement for a further three years, expiring on 30 June 2014. Key provisions of both HoA included the quantum of funding and the clinical services required to be delivered at the MCH.
Funding
14. The funding agreed between the Commonwealth and Tasmania for the management and operation of the MCH under the two HoA is outlined in Table S1. The 2008 HoA did not provide for an annual indexation factor to be applied to the funding, however, an indexation factor of 3.5 per cent was included in the 2011 HoA, to apply after the first year.
Table S.1: Commonwealth funding for the MCH under the HoA

Source: Heads of Agreement for the Management, Operation and Funding of the Mersey Community Hospital, 2008 and 2011.
Notes:
- Less than a full year’s funding due to timing of the Agreement.
- Funding not subject to indexation.
- Funding has been adjusted for indexation.
15. Under both HoA, the funding for the MCH is quarantined from:
- the Commonwealth Grants Commission assessment for the distribution of the Goods and Services Tax (GST) revenue pool to states and territories; and
- funding provided to Tasmania under national health funding arrangements.
16. The Tasmanian Government has accordingly remained eligible for its full entitlement of Commonwealth health-specific and other general funding streams.6 In addition to the Australian Government’s direct funding to the MCH under the HoA of $367 million, the MCH received $0.9 million under the National Partnership Agreement on Improving Public Hospital Services from 2011–12 to 2013–14. The Government has also allocated a total of $14 million to DoHA for the administration of the two HoA.
Clinical services delivery
17. The 2008 and 2011 HoA require Tasmania to ‘carry on the hospital diligently, honestly and in a professional and competent manner’7 and to comply with ‘responsible public hospital practice in respect of the hospital and in relation to any medical, clinical, surgical or other service’ provided at the hospital.8 The Schedule to the Agreements sets out 12 core clinical activities (see Appendix 2) that are to be ‘carried on by Tasmania’ at the MCH, without further specifying individual or relative activity levels.
18. The 12 core clinical activities specified in the 2008 and 2011 HoA were largely determined by the service profile of the hospital existing prior to the proposals for change set out in Tasmania’s Health Plan 2007. While there is flexibility for MCH management to develop and refine services outside the core clinical activities, changes to the core clinical activities can only be made with the agreement of the Commonwealth. There were no changes made to the core clinical activities during the life of the 2008 HoA. Under the 2011 HoA, the Australian Government Minister for Health agreed, on 18 October 2012, to changes in general surgery and paediatric inpatient services. These changes were sought by MCH surgeons to enable the safe delivery of the services.9
Differences between the 2008 and 2011 Heads of Agreement
19. While both HoA are set out in a similar way with a number of common terms and conditions, some key changes were introduced into the 2011 HoA, including:
- a limit of $250 000 on the use of Commonwealth funding for minor capital works to the hospital or its facilities, in contrast to the 2008 HoA, which specified that funding could be used for all upgrades and expansions to the hospital;
- the inclusion of annual indexation for the funding of 3.5 per cent;
- provision to ‘move towards’ activity based costing of services to allow for greater transparency of costs and benefits;
- expenditure reports to be provided monthly by Tasmania rather than quarterly, and an explanation for any variances of more than 10 per cent from the average expenditure for the previous three months; and
- recognition of the MCH’s position within the then NWAHS, providing for the involvement of the hospital and its facilities in Tasmania’s strategy for health service delivery in the state’s North West region.10 This addition formally reflects both parties’ acknowledgement that the MCH could not operate in isolation from other health services in its region.
Request for an audit
20. On 20 December 2011, the Senator for Tasmania, Senator the Hon Richard Colbeck, wrote to the Auditor-General informing him of allegations concerning the misuse of Commonwealth funding for the MCH in contravention of the HoA, and requested an investigation of those allegations.
21. After initial enquiries with DoHA, as the responsible Australian Government department, the Auditor-General drew Senator Colbeck’s request to the attention of the Joint Committee of Public Accounts and Audit (JCPAA) in February 2012, noting that the concerns raised by Senator Colbeck had also been aired in the national and Tasmanian media. The Auditor-General advised the JCPAA that an audit of the administration of the HoA would provide assurance to the Parliament on the use of Commonwealth funding at the MCH and the administrative effectiveness of the HoA, and potentially inform any further agreement between the Commonwealth and Tasmania on the operation of the hospital. The Auditor-General also advised that section 18B of the Auditor-General Act 1997 (the Act) allowed the ANAO to conduct, at the request of the JCPAA, a performance audit of a Commonwealth partner where the Commonwealth has provided money to the partner for a Commonwealth purpose.
22. The Chair of the JCPAA wrote to the Auditor-General on 28 March 2012, advising that the JCPAA had resolved to request the Auditor-General to undertake a performance audit of the administration of the 2008 and 2011 HoA for the management, operation and funding of the MCH. In response to this request, the Auditor-General decided to undertake the audit. It is the first performance audit conducted by the ANAO pursuant to section 18B of the Act. The audit was formally designated and commenced in July 2012.
Audit objectives and criteria
23. The objective of the audit was to assess the effectiveness of the administration, by DoHA and the Commonwealth partners, of the 2008 and 2011 Heads of Agreement for the management, operation and funding of the Mersey Community Hospital.
24. To conclude against the audit objective, the audit assessed whether:
- DoHA effectively established and administered the HoA for the MCH; and
- DHHS and the THO-NW are managing and operating the MCH in accordance with the HoA.
25. There were three organisations involved in the audit: DoHA and DHHS, the departments representing the Commonwealth and Tasmania as parties to the HoA, and the THO-NW, in recognition of its assumption of management responsibility for the MCH from 1 July 2012.
26. The scope of the audit had regard to the terms of the JCPAA request under section 18B(1) of the Auditor-General Act 1997, specifically the administration of both HoA, covering the period from 1 September 2008. Emphasis was given to whether Commonwealth funds were used in accordance with the HoA, and included consideration of whether the Commonwealth’s objectives for acquiring the hospital have been achieved. The audit did not examine operational decision-making within the hospital, such as decisions regarding appointments to clinical positions. The ANAO engaged an external firm with health sector expertise to provide technical assistance in analysing MCH expenditure transactions, performance and costs.
27. While this audit focuses on assessing the effective implementation of the arrangements for the management, operation and funding of the MCH, including the achievement of program objectives, the ANAO does not have a mandate to examine and report on the appropriateness of government policy. As such, this audit does not comment on the merits of the Australian Government’s decision to acquire the MCH from the Tasmanian Government in 2007 or its ongoing ownership.
Overall conclusion
28. In November 2007, the Australian Government purchased the MCH from the Tasmanian Government in response to local community concern over proposed service changes at the hospital. Since 1 September 2008, the Tasmanian Government has managed and operated the MCH under two HoA with the Commonwealth, established in 2008 and 2011. Under the two HoA over the six years from 2008 to 2014, direct Commonwealth funding to Tasmania for the management and operation of the MCH totals $367.3 million.
29. As the only Australian Government owned and funded hospital within a health care system where the delivery of public hospital services falls within the responsibilities of the states and territories, the MCH is uniquely placed. As such, the operation of the MCH necessitates arrangements that sit outside the general approaches adopted by the Australian Government to fund the delivery of health services by state and territory owned public hospitals. The establishment and ongoing management of these arrangements have presented a range of additional costs and challenges for DoHA, representing the Australian Government as the hospital owner, and the two state government entities—DHHS and the THO-NW—which have responsibility to operate the hospital within the broader Tasmanian health care system.
30. The recently expanded mandate of the Auditor-General, which provides for performance audits of Commonwealth partners under s18B of the Auditor-General Act 1997, has facilitated the ANAO’s examination of these unique arrangements. As the first performance audit involving a Commonwealth Partner, this report provides the governments and legislatures in both the Commonwealth and Tasmanian jurisdictions with our assessment of the administration of the arrangements governing the operation of the MCH. The audit does not, however, extend to commenting on the merits of the Australian Government’s decision to acquire the MCH from the Tasmanian Government in 2007 and its ongoing ownership as this decision reflects government policy.
31. In general, the administration of the 2008 and 2011 HoA by DoHA and DHHS has been effective in facilitating delivery, at the Commonwealth-owned MCH, of a range of agreed clinical services, including those specified under the HoA. Under the day-to-day management of DHHS, and more recently, the THO-NW, MCH clinical services have generally been delivered within an effective clinical governance framework. In addition, the majority of these services met or exceeded established national targets and benchmarks, particularly for the emergency department, elective surgery, inpatient management and the High Dependency Unit.11 Notwithstanding these achievements, the cost of service delivery at the MCH, while better than other Tasmanian acute hospitals, is significantly higher than comparable mainland hospitals—primarily driven by higher staff counts per units of weighted activity, more costly medical and surgical supplies, dependence on locum medical staff and higher administrative overheads.
32. The decision to assume ownership and continue existing service delivery at the MCH has come at an additional direct cost to the Commonwealth of $367.3 million over the six years to 30 June 201412 and resulted in greater risk exposure as hospital owner. These additional costs and risks, which arise from the unique arrangements adopted for the MCH, underline the need for effective and ongoing monitoring. At present, system limitations make it difficult for DHHS to readily provide assurance regarding the use of some Commonwealth funds, while weaknesses in the MCH performance framework mean that DoHA is not well positioned to assess whether its ownership and funding of the MCH is effective and whether the Commonwealth is receiving value for money from the arrangements. There remains scope for:
- DHHS, in conjunction with the THO-NW, to improve existing systems to provide greater assurance regarding the use of Commonwealth funds; and
- DoHA to expand its existing performance measurement framework for the MCH program and to strengthen its analysis of reported performance information collected under the framework to better demonstrate the extent to which the program is achieving its objectives.
33. While DoHA’s and DHHS’ administration of the HoA has facilitated the continuation of service delivery at the MCH, the differing objectives for the hospital held by the Commonwealth and Tasmania have not been fully reconciled: the Commonwealth’s objective primarily relates to the delivery of a set of core clinical services in place at the time the hospital was acquired, while Tasmania has sought to rationalise the delivery of hospital services in the state’s North West between the MCH and the NWRH at Burnie in line with the state’s health plan. To support the achievement of its objective, the Commonwealth has invested a substantial amount of direct funding, with the benefits to Tasmania extending beyond this amount, as it also receives a range of indirect financial benefits.13 Although the Commonwealth has retained the range of clinical services at the MCH outlined in the HoA, where it is safe to do so, Tasmania has also advanced the implementation of its health plan objectives for the state’s North West, with the MCH moving during 2012–13 from a 24 hour/seven day a week surgery facility to a mixed day and short stay surgery facility.
34. Notwithstanding a generally sound working relationship, which has supported the ongoing administration of the arrangements governing the operation of the MCH, the differing government objectives has meant that DoHA and DHHS have expended significant time and resources revisiting issues relating to service changes and hospital costs. In particular, the mechanism specified in the HoA for changing its provisions—a Clinical and Financial Services Plan—has not been effective. In addition, while the HoA recognise the need to manage the MCH as part of Tasmania’s health network in the North West, how this principle should apply in practice to the integration of services between the MCH at the NWRH at Burnie has not been settled between the parties. There also continues to be disagreement between the Commonwealth and Tasmania over responsibility for funding capital works at the hospital above the threshold of $250 000, and a compromise on this issue struck to enable the 2011 HoA to be agreed has not resolved this disagreement. The negotiation of any new HoA from July 2014 presents an opportunity to address these issues and establish a clear and agreed strategic direction for the MCH.14
35. Over the period that the Commonwealth has owned and funded the MCH, there have been persistent allegations reported in the Tasmanian and national media that Commonwealth funds for the MCH have been used outside the MCH contrary to the terms of the HoA. With regard to these allegations, the Tasmanian Government has stated that ‘the MCH operates its funding in accordance with the detailed and publicly available Heads of Agreement’.15 Further, DHHS informed the ANAO that it has ‘only used Commonwealth funds for the performance of this project [the MCH program]’. The ANAO’s testing of expenditure transaction samples over a four year period found no evidence to indicate that the MCH was using Commonwealth funds outside the HoA requirements in the categories of employee, supplies and pharmaceuticals expenditure, which have been the subject of such allegations.
36. Nevertheless, the inability of DHHS and MCH systems to readily provide the ANAO with complete transaction listings for MCH expenditure on shared corporate services and cross-charging between the MCH and other hospitals meant that it was not possible during the audit to form an overall judgement on the appropriateness of the use of funds in these categories. There is, therefore, scope for DHHS and the MCH to improve existing systems to better inform hospital management and oversight, provide greater assurance to respective governments, and to more efficiently demonstrate adherence to DHHS’ obligations arising from the HoA.
37. While the MCH performs well in comparison to other Tasmanian hospitals with regard to the cost of delivered services, it does not perform as well against comparable mainland hospitals. For example, while the MCH’s average cost per weighted separation16 of $5125 was $1550, or 43 per cent, higher than the average cost for its peer group of mainland hospitals17, it was $729, or 12 per cent, lower than the other Tasmanian hospitals. As outlined earlier, the higher cost of MCH clinical services in comparison to its peer group is primarily driven by higher staff counts per units of weighted activity, medical and surgical supplies, dependence on locum medical staff and administrative overheads. Some of these costs reflect structural factors within Tasmania that contribute, in part, to the higher cost of service delivery.18 However, there would be benefit in further exploring options to improve the efficiency of service delivery at the MCH by reviewing costs in particular areas, such as for locum medical staff.19
38. The Commonwealth’s objectives for ownership of the MCH, which DoHA terms the ‘core outcome’ of the HoA, have been narrowly defined as the continuing provision of the core clinical activities, with existing performance measures not directly addressing the impact of those activities on the community serviced by the MCH. Furthermore, the Commonwealth preferred that the HoA not define the performance or service quality standards—of a kind that would normally be included in a services contract with a private sector provider—that Tasmania is required to meet as the operator of the MCH.20
39. The categories of operational and clinical information reporting that Tasmania is required to provide have not been updated since 2008 and, while there have been some recent improvements in DoHA’s approach to its scrutiny of MCH performance information, the department’s analysis of data reported under the two HoA has not been undertaken in a consistent and structured manner. These factors limit the Commonwealth’s ability to assess whether the MCH is performing effectively, and whether it is receiving value for the significant amount of direct and indirect funding provided for the MCH program.
40. Commonwealth ownership has resulted in the need to establish unique arrangements for the management and operation of the MCH, which have come at additional cost and complexity as compared to the standard model of providing Commonwealth funding for public hospitals through health care agreements. A range of direct and indirect costs have been borne primarily by the Commonwealth, with the quarantining of funding for the MCH from the CGC’s assessment for the distribution of the GST revenue pool also affecting the funds available for distribution to other states and territories. The ongoing administration of the HoA also necessitates a substantial commitment from administering agencies, relating to ongoing administration and periodic negotiation. Further, the Commonwealth continues to shoulder risk as the owner of the MCH, notwithstanding its day-to-day management and operation by Tasmanian Government entities. In recognition of the additional costs, risks and complexity arising from ad hoc arrangements of this type, it is to be expected that responsible agencies will continue to monitor and keep under review the implementation of desired objectives in order to be in a position to advise governments on the benefits of the current arrangements over alternative options.
41. While the HoA support the continued delivery of a range of clinical services by the MCH to patients in its catchment, the strengthening of elements of the agreement and improvements in aspects of the responsible entities’ administration have the potential to improve overall hospital performance and contribute to enhanced accountability. In this respect, the ANAO has made five recommendations—two directed to DoHA, one directed to DHHS and two directed jointly to both agencies. These recommendations are designed to enhance the utility of the HoA, provide greater assurance regarding the use of Commonwealth funds and strengthen the measurement of achievements against the MCH program objectives. There are also a number of suggestions made in the report to enhance the administration of the HoA, most notably: resolving the issue of responsibility for funding of capital works at the MCH; clarifying the extent of community engagement necessary to underpin decision-making on the MCH’s service profile; and strengthening arrangements for the management of MCH assets.
Key findings
Effectiveness of the Heads of Agreement
42. Negotiations between the Commonwealth and Tasmania to establish both the 2008 and 2011 HoA, and agree the quantum of Commonwealth funding to the MCH under both, delivered HoA that have generally been effective in supporting the operation of the hospital. However, some aspects of the form and content of the HoA as negotiated between the parties have not supported the effective administration of the MCH arrangements.
43. In particular, the HoA specify a Clinical and Financial Services Plan as the mechanism to amend the agreements, but this has not been effective as a means for agreeing changes to the HoA or for negotiating changes to the MCH’s service profile. On the occasions when a Plan has been agreed, the timing of that agreement late in the year21 has not allowed that Plan to be used effectively by the hospital to guide operational activities, and often its finalisation has come at the expense of the timely development of the following year’s Plan. This is undesirable in a dynamic hospital environment. In the context of negotiating any new HoA from 1 July 2014, there would be merit in the parties examining the role of the Clinical and Financial Services Plan, in particular its status as an annual plan and whether an alternative process should be established for negotiating and agreeing ‘supplementation and amendment’ to the HoA.22
44. The form of the two HoA for the management, operation and funding of the MCH is a hybrid between a funding agreement and a services contract. The HoA do not contain any requirement for Tasmania, as the operator of the MCH, to meet performance or service quality standards of the kind that would normally be included in a services contract with a private sector operator.23 Further, the categories of operational and clinical information reports that Tasmania is required to provide to the Commonwealth under the Schedule to the HoA have not been reviewed or amended since 2008. There would be benefit in reviewing these categories to ensure that they align with contemporary measures of hospital performance. Moreover, DoHA’s analysis of the data reported has not been undertaken in a consistent or structured manner over the life of the two HoA. These issues inhibit the Commonwealth’s ability to assess whether the hospital is performing effectively in meeting the Commonwealth’s objectives.
45. There is ongoing disagreement between the parties over the responsibility for capital funding for the MCH. In the negotiation of the 2011 HoA, a compromise was agreed that limited use of Commonwealth funding for any minor capital works to an amount of $250 000 and allowed Tasmania to apply to the Health and Hospitals Fund (HHF)24 for capital funding above that limit. However, Tasmania’s subsequent application to the HHF for $22.8 million in capital funding for the MCH was unsuccessful. It is apparent that the compromise that was agreed to enable the 2011 HoA to be signed was understood differently by the parties. DHHS considers that the terms of the 2011 HoA removed any obligation from Tasmania to fund capital works above $250 000, and placed that obligation on the Commonwealth as the owner of the facility. In response, the Commonwealth has noted that there is no provision in the 2011 HoA for it to fund additional capital works above $250 000. Given the potential impact on the quality of hospital facilities and the delivery of clinically safe services, resolution of the issue of responsibility for capital funding, including an appropriate process for considering specific requirements, should be addressed in the context of negotiating any new HoA from 1 July 2014.
Expenditure of Commonwealth funds for the MCH
46. The Commonwealth’s direct funding for the MCH under the HoA is the subject of financial reporting requirements and subsequent scrutiny by DoHA and DHHS. While areas of concern have been identified through this scrutiny, these concerns have been resolved in consultation between the parties. For example, in 2009 and 2010, the Commonwealth questioned Tasmania’s management of orthopaedic services in the North West region by treating patients from the MCH’s catchment area at the NWRH and charging the MCH for that service. As Tasmania advised that it met those costs from MCH revenue, rather than from direct Commonwealth funding, this approach was not considered by DoHA to be contrary to Tasmania’s HoA obligations.
47. The media has reported claims about the use of Commonwealth funds allocated to operate the MCH for expenses associated with employees, pharmaceuticals and supplies at the NWRH at Burnie.25 The ANAO’s substantive testing of MCH and DHHS accounting records, covering transactions randomly sampled over the four years from 2008–09 to 2011–12, found no evidence to indicate that the MCH was using Commonwealth funds outside the HoA requirements in the categories of employee, supplies and pharmaceuticals expenditure. In the area of expenditure on patient transport, a number of transactions were identified in the accounts analysed where patient travel could not be separated from staff travel, meaning that the ANAO could not form an overall conclusion for the patient transport category. However, the transactions examined did not show that funds were used inconsistently with the HoA, and broader analysis indicates that the MCH’s patient transport costs are not inconsistent with those of other Tasmanian hospitals.
48. While Tasmania is required, under the HoA, to maintain complete and current financial records relating to all aspects of the operation of the MCH, DHHS could not provide the ANAO with complete transaction listings for expenditure on shared corporate services provided to the MCH, and cross-charging between the MCH and other hospitals. This meant that the transaction samples tested by the ANAO did not represent a full population of transactions in these categories and, therefore, it was not possible to form an overall judgement on the appropriateness of the use of funds for these categories. While DHHS has since advised that it has developed an IT solution to provide a full population of cross-charging expenditure transactions, there remains scope to address systems limitations to better inform hospital management and oversight, provide greater assurance to respective governments, and to more efficiently demonstrate adherence to DHHS’ obligations arising from the HoA. Such systems improvements include aligning reporting and conducting periodic system reconciliations, to better position DHHS to fulfil Tasmania’s obligations under the HoA, as well as provide greater transparency around the use of Commonwealth funds.
49. With regard to expenditure on assets, the ANAO examined the controls in place at the MCH to manage the purchase, transfer, repair and disposal of assets at the hospital. These assets are owned by the Commonwealth. The ANAO found that there was scope for the MCH to strengthen its asset control systems, including implementing a regular asset stocktake program, to provide greater assurance regarding the management of hospital assets purchased with Commonwealth funds.
MCH management and performance
50. The MCH’s corporate and clinical governance arrangements align with national standards and are consistent with the requirement under the HoA that Tasmania carry on the hospital in a professional and competent manner and comply with responsible public hospital practice. The ANAO’s analysis of the MCH’s clinical services indicated a number of well-performing areas. Performance results for inpatient management, High Dependency Unit demand and elective surgery wait times under the National Elective Surgery Target26 were all positive. The MCH’s emergency department is performing strongly against national benchmarks for patients to be seen within minimum times for their category of care (triage category), although there is some scope to improve the treatment times for patients in triage categories 3, 4 and 5, to bring these up to the performance levels recorded across the other acute care hospitals in Tasmania.27 The MCH also comfortably achieved the state target in 2012, under the National Emergency Access Target28, for patients being discharged from the emergency department within four hours.
51. The MCH recorded less positive performance results for aspects of its obstetrics service and for infection rates. Obstetrics data showed a higher rate of first birth (primipara) caesareans at the MCH than its peer group hospitals (48 per cent of first time mothers had caesareans at the MCH compared with 22 per cent at peer group hospitals), and a lower percentage compared with its peers of emergency caesareans commenced within the recommended 30 minutes (37 per cent compared to 73 per cent at peer group hospitals). A proposed review of obstetrics at the MCH is likely to assist with identifying practical changes that can improve these performance results. With regard to infection rates, the MCH did not meet the national target for the staphylococcus aureus bacteraemia (SAB)29 infection rate in 2010–11 and 2011–1230, and its rate of clostridium difficile infection (CDI)31 has progressively worsened since 2008–09, to be the highest CDI rate among Tasmanian hospitals in 2011–12. While a proportion of such infections may have been contracted before patients present to the hospital, there would be benefit in the THO-NW investigating potential causes for these infection rate results to inform remedial action.
MCH efficiency
52. The ANAO examined the MCH’s weighted costs32 for acute care and all care types against a national peer group of 10 medium sized inner regional hospitals and against the three other acute care hospitals in Tasmania. The MCH’s average weighted costs for acute care and for all care types were significantly more expensive than its peer group by, respectively, 43 per cent and 23 per cent. However, the MCH is less costly on these weighted measures than the other Tasmanian hospitals, being 12 per cent lower per unit of weighted activity for acute care and seven per cent lower for all care types. While the characteristics of the MCH as a lower acuity hospital, with significant amounts of lower cost activity in day surgery, outpatient care and emergency department presentations, contribute to this result, it broadly indicates that the MCH is operating more efficiently than other Tasmanian hospitals.
53. Two of the key expenditure categories contributing to higher costs at the MCH compared to its peer group were identified as a high staff-to-patient ratio33 and high medical and surgical supply costs34. High costs in these areas are common to the other Tasmanian hospitals, and the ANAO has been informed that work is underway within DHHS to examine options to improve Tasmania’s performance with regard to the cost of supplies. The other drivers of higher costs at the MCH are expenditure on locum medical staff35 and general administration costs36, and it would be timely for the THO-NW and the MCH to review the factors influencing these costs and put in place effective strategies to improve efficiency in those areas of expenditure. The ANAO notes that the Commission on Delivery of Health Services in Tasmania37 has a mandate from the Australian and Tasmanian governments to make recommendations with respect to remediating identified inefficiencies in the delivery of public health services in Tasmania, and recommending improvements to hospital system performance, and will produce a detailed report later in 2013.
Achievement of Commonwealth objectives in owning and funding the MCH
54. There was a high degree of congruence between successive Australian Governments’ objectives in owning and funding the MCH, which emphasised the importance of maintaining, for the benefit of the local community, the clinical services at the hospital that were subject to change under Tasmania’s Health Plan 2007, and ensuring local community engagement in decision-making on the MCH’s service profile.
55. However, measures of performance, including the Key Performance Indicators (KPIs) in DoHA’s Portfolio Budget Statements (PBS), have defined effectiveness narrowly as the continuing provision, at the MCH, of the core clinical activities specified in the HoA. That measure of effectiveness has been achieved. However, the impact of providing those activities—at the MCH—on the health needs of the local community, which was at the heart of the Commonwealth’s intervention, has not been adequately represented in measures of performance and effectiveness for the program.
56. Notwithstanding the inclusion, in Recital A of both HoA, of a statement of objective that contains broader dimensions than that in the PBS, the absence of an adequate performance framework in the HoA to measure these dimensions hampers the Commonwealth’s ability to assess the standard and quality of service provision at the MCH. In addition, until recently, DoHA has not fully utilised the operational and clinical information reported to it under the HoA to evaluate the performance of the MCH. The lack of KPIs addressing the impact and cost-effectiveness of the MCH program means that the Commonwealth is not well placed to assess whether its ownership and funding of the MCH is effective.
57. With regard to whether the Commonwealth has received value for money from its ownership and funding of the MCH, the MCH program has not been subject to value for money analysis by the Commonwealth in either a policy advising context or in the performance management process associated with the establishment and administration of the HoA. There are some positive indicators in relation to the cost component of a value for money judgement, insofar as the quantum of funding agreed for the two HoA conformed closely to the funding envelopes for negotiation agreed by the Australian Government. Further, as previously mentioned, the MCH is a relatively efficiently run hospital compared with the other Tasmanian acute hospitals. However, a robust assessment of the value achieved from funding the MCH’s operations, particularly the core clinical services the Commonwealth requires it to provide, necessitates a focus on the outcomes from the provision of those services, particularly the impact on the health needs of the local community. At present, the Commonwealth’s performance measurement framework for the MCH program, with its focus on the provision of the core clinical activities rather than on their impact, is not capable of supporting an assessment of value for money achieved from the substantial direct and indirect funding provided for the MCH program. Enhancements to the monitoring of the performance of the MCH program would better position DoHA to advise government on the merits and operational benefits of various options for the delivery of the hospital services to the Latrobe region.
Summary of agency responses
58. Summary responses to the proposed report from each of the organisations involved in the audit are provided below, with the full responses provided at Appendix 1 to this report.
Australian Government Department of Health and Ageing
In delivering the Mersey Community Hospital program, the Department’s focus is at all times on the current Australian Government’s established policy priority for the Mersey Community Hospital: the availability to the local community of North West Tasmania of hospital services which are safe, high quality and based on clinical need. As noted in the report, the Department has made enhancements to its administration of the program over time. The Department will continue its efforts in these areas, both as part of normal business practice and in the context of any future agreement with Tasmania. The Department agrees with the ANAO’s recommendations.
Tasmanian Government Department of Health and Human Services
The audit has provided an opportunity for the Department, with Tasmanian Health Organisation – North West, to review current systems and practices at the Mersey Community Hospital (the Mersey), but also systems at a broader state-wide level. In addition to the recommendations, the audit has made a number of observations with regard to shared services and systems that the Department is actively considering, and responding to internally.
The conclusion of the audit is timely, ahead of negotiating the arrangements for the continued management, funding and operation of the Mersey. The findings of the ANAO will inform these negotiations, particularly regarding working towards a mutually agreeable resolution to capital funding for the Mersey and considering the purpose of the clinical and financial services plans in the context of negotiating service change.
Tasmanian Health Organisation–North West
[The Chief Executive Officer of the Tasmanian Health Organisation – North West] concurs with the Secretary of DHSS that the findings of the audit provide direction to the THO-NW, together with DHHS, regarding key improvements that can be made to systems associated with management of the MCH; work has commenced to this end.
With the physical condition of the MCH likely to come under scrutiny through the next accreditation process, [the Chief Executive Officer] is keen to resolve the outstanding ambiguity regarding responsibility for funding of capital works. It is also important that there is a clear mechanism for agreeing service change. Successful resolution of these matters will impact on the extent to which [the Chief Executive Officer] is able to ensure the delivery of quality, safe hospital services at the MCH within the available budget.
Recommendations
|
Recommendation No.1 Paragraph 3.25 |
To assist with the timely finalisation and effective implementation of the Clinical and Financial Services Plan for the MCH, the ANAO recommends that DoHA and DHHS:
DoHA response:Agreed. DHHS response:Agreed. |
|
Recommendation No.2 Paragraph 3.46 |
To improve the Commonwealth’s ability to monitor and assess the performance of the MCH under any future HoA, particularly the quality and safety of the services being delivered, the ANAO recommends that DoHA review the categories of operational and clinical information required to be reported under the HoA, with a view to:
DoHA response:Agreed. |
|
Recommendation No.3 Paragraph 5.69 |
To improve the transparency of expenditure reporting for the MCH and to provide greater assurance that Commonwealth funds are being used in accordance with the HoA, the ANAO recommends that DHHS:
DHHS response:Agreed. |
|
Recommendation No.4 Paragraph 6.97 |
To support the efficient delivery of health care services at the MCH, the ANAO recommends that DoHA and DHHS initiate a targeted review by the THO-NW of the MCH’s use of locums to determine whether there are any additional measures that can be taken by the hospital to better manage these costs. DoHA response:Agreed. DHHS response:Agreed. |
|
Recommendation No.5 Paragraph 7.63 |
To better assess the effectiveness of the Commonwealth’s ownership and funding of the MCH, and whether the Commonwealth is receiving value for money from the MCH arrangements, the ANAO recommends that DoHA expand its performance measurement framework for the MCH program to:
DoHA response:Agreed. |
Footnotes
[1] The full-time equivalent (FTE) staffing level was 300. Department of Health and Human Services, Achieving Results in the NWAHS, April 2012.
[2] The 2008 and 2011 Heads of Agreement are available on the Department of Health and Ageing’s website, at <http://www.health.gov.au/internet/main/publishing.nsf/Content/mersey-community-hospital-HOA>.
[3] Tasmanian Health Organisations are independent statutory authorities managed by a Chief Executive Officer, and each is responsible to a Governing Council, which in turn reports to the Tasmanian Minister for Health and the Treasurer.
[4] Australian Labor Party, ‘Investment in Tasmanian Health’, 25 September 2007.
[5] This objective was retained in the 2011 HoA with two minor modifications to reflect the continuity of the arrangement.
[6] Health-specific funding to Tasmania includes: $265 million in 2010–11 under the National Health Care Specific Purpose Payments; eligibility for up to $89.2 million through to 2016–17 under the National Partnership Agreement on Improving Public Hospital Services; and $325 million over four years under the Commonwealth’s emergency rescue package for the Tasmanian health system announced on 15 June 2012.
[7] Heads of Agreement for the continued management, operation and funding of the Mersey Community Hospital, 2011, Clause 8.2(b).
[8] ibid., Clause 8.2(e).
[9] The changes to surgery agreed on 18 October 2012 limit the surgery performed at the MCH to weekdays between 9am to 5pm, and outside of these hours where clinically necessary, rather than continuing to make surgery available 24 hours a day, seven days a week.
[10] Heads of Agreement for the continued management, operation and funding of the Mersey Community Hospital, 2011, Clause 23.
[11] The cost and performance of the MCH across key areas of clinical activity is discussed in detail in Chapter 6 of the report. For example, in relation to the performance of the emergency department in 2012, the MCH reported a National Emergency Access Target performance level of 77 per cent, against a target of 72 per cent. The NEAT is a key performance indicator (KPI) used to assess the performance of emergency departments under the National Partnership Agreement on Improving Public Hospital Services.
[12] See Table S1, which provides details of annual funding levels under each HoA. A further $14 million has been allocated to cover the cost of administration of the two HoA by DoHA.
[13] These indirect benefits include: the retention of $34 million in annual recurrent savings (in 2008 prices) from its funding of the hospital prior to the Commonwealth’s purchase; the exemption of MCH funding from Commonwealth Grants Commission assessments of GST distribution to the states and territories, and from the calculation of funding levels provided under national health initiatives; and the retention of MCH revenue.
[14] The Tasmanian Government Minister for Health wrote to the Australian Government Minister for Health and Ageing on 27 June 2013 to commence negotiations for the management, administration and operation of the MCH beyond the expiry of the 2011 HoA on 30 June 2014.
[15] Similarly, the Tasmanian Government has also been publicly reported as rejecting allegations of this type, stating that ‘funding and resourcing of the Mersey Hospital is strictly in accordance with the three-year federal agreement’ [‘Hospital funding inquiry urged’, ABC News, 22 December 2011].
[16] A weighted separation is an episode of admitted patient care that incorporates the level and complexity of the treatment provided. These figures are for acute admitted care in 2009–10, the latest data from the National Hospital Cost Data Collection available at the time of the audit’s analysis.
[17] The MCH was compared to 10 mainland hospitals classified as medium inner regional hospitals that displayed a very similar casemix to the MCH.
[18] These factors include Tasmanian’s capacity to achieve savings in medical and surgical supply costs given the size of the health system in comparison to other jurisdictions.
[19] MCH locum costs in 2010–11 represented 15.3 per cent of the hospital’s expenditure on salary and wages, which was significantly (88 per cent) higher than the next highest Tasmanian hospital.
[20] DoHA considered that this high level approach provided Tasmania with clear responsibility and the necessary flexibility for day-to-day hospital management, reduced the Commonwealth’s risk exposure in respect to hospital management and minimised departmental administration.
[21] A Clinical and Financial Services Plan was not agreed for 2009–10. The Plan for 2010–11 was agreed on 17 February 2011. The Plan for 2011–12 was agreed on 29 June 2012.
[22] In the context of the Clinical and Financial Services Plan, the term ‘supplementation’ refers to any additions to the HoA, while the term ‘amendment’ refers to changes to existing clauses.
[23] The information available to the Commonwealth under the HoA relating to the performance of the MCH is relatively limited, is not described as ‘performance’ information, and does not include measurable performance indicators or standards.
[24] The Health and Hospitals Fund (HHF) was established by the Australian Government in the 2008–09 Budget to fund capital investment in health facilities, including renewal and refurbishment of hospitals, medical technology equipment and major medical research facilities and projects. Applications for funding from the HHF are assessed by an Advisory Board against evaluation criteria agreed by the Australian Government Minister for Health. The ANAO recently completed a performance audit of the administration of the HHF (ANAO Performance Audit No. 45 of 2011–12), available at <www.anao.gov.au>.
[25] See, for example, Tingle, L ‘Claims funds bypassed Mersey’, The Australian Financial Review, 1 December 2011, p. 12; Kempton, H ‘Hospital cash switch storm’, The Mercury, 22 December 2011; and ‘Hospital funding inquiry urged’, ABC News, 22 December 2011.
[26] The 2011 National Partnership Agreement on Improving Public Hospital Services commits participating states and territories to targets relating to elective surgery and emergency department care. The National Elective Surgery Target (NEST) sets progressive targets for each state and territory for patients waiting for elective surgery to be treated within the clinically recommended time for their category of urgency.
[27] The NWRH at Burnie, the Royal Hobart Hospital and the Launceston General Hospital.
[28] The National Emergency Access Target (NEAT) sets progressive targets for each state and territory to achieve, by 2015, 90 per cent of all patients presenting to a public hospital emergency department either ready to leave the emergency department for admission to hospital, referred to another hospital for treatment, or discharged within four hours.
[29] Staphylococcus aureus bacteraemia (SAB) is a bloodstream infection with an estimated mortality rate of approximately 25-30 per cent of infected patients.
[30] The MCH recorded an SAB infection rate of 2.3 case per 10 000 occupied bed days in 2010–11 and 2.1 cases in 2011–12, which exceeded the National Healthcare Agreement target of 2.0.
[31] Clostridium difficile infection (CDI) is an infection of the bowel and affects patients in a similar way to SAB in increasing the risk of mortality, and often resulting in longer hospital stays.
[32] As public hospitals have differing profiles in relation to the types of care provided and the mix of patients serviced, which vary in cost, the accepted approach to comparing costs between hospitals involves applying agreed weightings to these variables to produce a standard unit of activity on which comparisons can be made.
[33] In 2010–11, the MCH had 37.8 full-time equivalent (FTE) staff per 1000 units of weighted activity compared with 29.0 FTE for the MCH’s peer group and 39.8 FTE for the other Tasmanian hospitals. Further, the MCH’s average salary and wage cost of $3195 per unit of weighted activity in 2010–11 was 19 per cent higher than the average cost per unit of $2668 for the medium inner regional hospital peer group. However, the MCH’s cost on this measure is five per cent lower than for the other Tasmanian hospitals ($3367).
[34] Expenditure on medical and surgical supplies was 72 per cent higher for the MCH ($717) compared with its peer group of hospitals ($416).
[35] MCH locum costs in 2010–11 represented 15.3 per cent of the hospital’s expenditure on salary and wages, which was significantly (88 per cent) higher than the next highest Tasmanian hospital.
[36] Expenditure on administration was 82 per cent higher at the MCH ($466) than the average for its peer group of hospitals ($255).
[37] The Commission was established as part of a $325 million package of assistance to Tasmania’s health system announced by the Australian Government on 15 June 2012. It presented an interim report to the Commonwealth and Tasmanian Health Ministers in December 2012.